Detection of carotid atherosclerosis might help to better identify individuals susceptible to cardiovascular events. We aimed to quantify the number of participants with carotid atherosclerosis and low-to-intermediate cardiovascular risk according to the traditional risk factor scoring, and therefore with an elevated risk of cardiovascular events.
MethodsCross-sectional, observational study performed during a cardiovascular screening program. From a total of 3778 volunteers, low-to-intermediate cardiovascular risk individuals (N=2354) were identified and studied. Physical examination, blood test, and carotid ultrasound followed standard procedures. Common, bulb, and internal carotid arteries were examined and common carotid intima-media thickness was measured. SCORE risk value was calculated for all participants. Univariate and multivariate statistical analysis was performed.
ResultsMean age of participants was 58.9 (15) years, 43.8% were men, 23.7% had hypertension, and 20.5% had hypercholesterolemia. The mean SCORE value was 1.47 (1.4). Both carotid intima-media thickness and the prevalence of carotid plaques increased steadily and significantly (P<.005) as advanced decades of life were analyzed. Variables significantly related with the presence of carotid atherosclerosis were age, male sex, and systolic blood pressure. Interestingly, 592 (25.1%) individuals were reclassified to a higher risk due to the presence of carotid atherosclerosis.
ConclusionsThere was a clear dissociation between cardiovascular risk scoring and the presence of atherosclerosis, because 1 of 4 study participants at low-to-intermediate cardiovascular risk had carotid atherosclerosis.
Keywords
.
INTRODUCTIONPrimary prevention of cardiovascular diseases (CVD) is based on the identification of high-risk individuals. However, the traditional cardiovascular risk factor approach is not efficient and not adequately inclusive. Interestingly, just 1 out of 4 young participants with coronary heart disease met the National Cholesterol Education Program criteria for treatment with statins, leading researchers to conclude that the risk factor approach underappreciates risk, especially in young people.1
Consequently, current clinical guidelines recommend additional noninvasive diagnostic tests to assess the presence of atherosclerosis.2 Carotid ultrasound (intima-media-thickness [c-IMT] measurement and identification of plaques) is a validated technique to assess systemic atherosclerosis.3 Initially described in 1986 by Pignoli et al.,4 c-IMT has been extensively utilized in population-based studies5,6 and numerous clinical trials7,8; the findings associated with an increased c-IMT or the presence of plaque are associated with coronary atherosclerosis.9
The additive information provided by c-IMT measurements has been previously addressed. In a study of 409 patients with hyperlipidemia,10 carotid ultrasound was used to reclassify 91(48%) individuals considered at low risk by the traditional Framingham risk score (<5%), due to their increased c-IMT (carotid atherosclerosis). Similarly, participants who were initially classified as low-to-intermediate risk by the Framingham score in the absence of hyperlipidemia were reclassified based on the results of c-IMT measurements.11 Our group has also shown that the use of carotid ultrasound helps to reclassify patients with chronic kidney disease, a group in which the role of classical risk factors is controversial.12 In addition, studies done in healthy individuals and the Spanish population have reported the normality range values of c-IMT.13,14 However, there is a paucity of data aimed at the identification of carotid atherosclerosis in apparently healthy, asymptomatic individuals, including both c-IMT values and the presence of carotid plaque. The aim of the present study is to assess carotid atherosclerosis to quantify the number of patients who would be reclassified from the traditional risk factor scoring.
METHODSDesign and ProceduresThis is a cross-sectional, observational study performed in 7 cities in Spain (Alicante, Ourense, Barcelona, Madrid, Valladolid, Zaragoza, and Sevilla) during a 1-year information campaign run by the Spanish Heart Foundation and both the Spanish and European Societies of Cardiology. The study was organized similarly in each city during a whole weekend (Saturday and Sunday). A specific place (consisting of several large tents) was established in a centric or highly crowded place and appropriately advertised in the local media, hospitals, and patient organizations. Participants were screened during 7 weekends (14 days), from June to October 2009, by 3 nurses, 2 highly trained research nurses to perform carotid ultrasound, and 1 data manager. Individuals were consecutively invited to participate without restrictions and the protocol was as follows:
- 1.
Demographic data: we recorded age, sex, smoking status, and previous CVD (coronary heart diseases, stroke/transient ischemic attack, peripheral vascular diseases) and previous diagnosis of diabetes mellitus or hyperlipidemia/hypertension or current treatment with lipid-lowering/blood pressure drugs.
- 2.
Physical examination: blood pressure was recorded according to Joint National Committee-7 guidelines15 using an Omron M6. Body weight (kg), height (m), and waist circumference (cm) were also measured.
- 3.
Laboratory results: total cholesterol was measured by fingerstick using CardioCheck® (Polymer Technology Systems, Inc.; Indianapolis, Indiana, United States). Based on these results, the SCORE risk value (calibrated for Spanish population) was calculated.
- 4.
Carotid ultrasound was performed as previously described.16 Briefly, participants were screened using a Vivid i (General Electric Healthcare), equipped with a linear transducer (8L) with a frequency range from 8-13MHz. Both carotids were examined following the standard operational procedure and published Mannheim consensus.17 A cross-sectional view of the common, bulb, and internal carotid arteries was initially explored to identify the presence of atheromatous plaques, defined as a focal encroachment into the lumen of the carotid superior or equal to 1.5mm.6 A longitudinal view of the posterior wall of the common carotid artery 10mm proximal to the initiation of the bulb was then identified and the c-IMT was measured on-line using the semi-automated software AutoIMT® (GE Healthcare; Haifa, Israel). For c-IMT purposes, nonevaluable segments were considered as missing. Any c-IMT values above 1.5mm were considered as plaques.6
Data are expressed as mean (standard deviation) and percentages, as appropriate. Conventional tests to assess the normality of quantitative variables were applied. To analyze differences between groups we used analysis of variance with post-hoc Bonferroni test for quantitative variables and chi-squared test for categorical ones. Correlation coefficients were applied to study the relationship between quantitative variables. A logistic regression model was applied to study variables related to the presence of carotid atherosclerosis. The dependent variable was “carotid atherosclerosis,” defined by the presence of a plaque or c-IMT>1.5mm. As independent variables, we used age (decades of life), sex, smoking, hypertension, hypercholesterolemia, body-mass index, blood pressure, total cholesterol, and SCORE value.
Using a specialized reader (B.C.), 10% of the images were randomly remeasured off-line. The intra-class correlation coefficient was 93%.
RESULTSGeneral Characteristics and Atherosclerosis AssessmentWe screened 3778 individuals during the study, excluding 938 because of diagnoses of type 2 diabetes mellitus, previous coronary heart disease or stroke, or a SCORE cardiovascular risk value >5%. Of the remaining pool (2840) of participants, 2354 individuals had the full examination. General characteristics of the population included in the study, by decades of life, are listed in Table 1.
General Characteristics of the Participants Included in the Study
| No high CV risk (N=2354) | Age group | ||||
| <50 years (N=615) | 51-60 years (N=463) | 61-70 years (N=712) | >70 years (N=564) | ||
| Demographic data | |||||
| Age, years | 58,9±15 | 38±8 | 56±2 | 65±2 | 76±4 |
| Sex, male | 1031 (44) [42-46] | 271 (44) [40-48] | 205 (44) [40-49] | 312 (44) [40-47] | 243 (43) |
| Current smokers | 296 (12.6) [11.2-13.9] | 154 (25) [22-28] | 78 (17) [13-20] | 52 (7.3) [5.4-9.2] | 12 (2.1) [0.9-3.3] |
| High blood pressure | 559 (24) [22-26] | 27 (4,4) [2,8-6] | 88 (19) [15-23] | 211 (30) [26-33] | 233 (41) [37-45] |
| Hypercholesterolemia | 482 (20,4) [18.7-22.0] | 28 (4,6) [2.9-6.2] | 96 (21) [17-24] | 202 (28) [25-32] | 156 (28) [24-31] |
| Physical examination | |||||
| Systolic blood pressure, mmHg | 129±19 | 119±16 | 129±19 | 133±18 | 136±19 |
| Diastolic blood pressure, mmHg | 78±10 | 75±10 | 80±11 | 79±10 | 78±11 |
| Body mass index, kg/m2 | 27.1±4.1 | 25.7±4.0 | 27.1±4.0 | 27.7±3.0 | 28.1±3 |
| Abdominal perimeter, cm | 94±11 | 88±13 | 93±11 | 96±10 | 98±9 |
| Laboratory results | |||||
| Total cholesterol, mg/dL | 175±34 | 169±33 | 179±36 | 178±33 | 173±32 |
| Cardiovascular risk assessment | |||||
| SCORE | 1.47±1.40 | 0.02±0.2 | 0.84±0.70 | 2.15±1.14 | 2.70±1.16 |
CV, cardiovascular.
Data are expressed as mean±standard deviation or no. (%) [confidence interval 95%].
Mean age was 58.9 (15) years and 43.8% were males. The distribution between males/females was not significantly different in the different decades of life. Among classical cardiovascular risk factors, 12.6% were current smokers, 23.7% had hypertension or were taking drugs to lower blood pressure, and 20.4% were diagnosed of dyslipidemia. Results found on physical examination are listed in Table 1 and mean SCORE value was 1.47 (1.4). The c-IMT results and prevalence of carotid plaques, stratified by sex and decades of life, are displayed in Figure 1. The c-IMT was significantly higher in males than females except in the fifth decade (51-60 years). As expected, we observed a progressive and statistically significant increase of c-IMT as older individuals were examined (Fig. 1A; analysis of variance; P-value<.005).
Carotid intima-media thickness (A) and prevalence of carotid plaques (B) according to sex and decades of life. IMT, intima-media thickness. Mean carotid intima-media thickness values are displayed at the bottom of each column. aP<.05 when comparing male/female. bP<.05 when comparing across different decades of life.
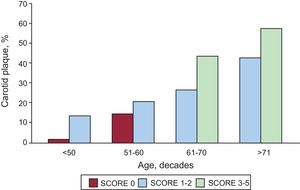
Similarly, the presence of carotid plaques was significantly (P<.05) higher in men than in women in every decade of life. Further, the prevalence of carotid plaques increased steadily and significantly at older ages, ranging from 2.2% in those<50 years old to 48.1% in participants older than 71 (Fig. 2).
Variables Related to Carotid AtherosclerosisThe c-IMT was significantly and positively related to age, systolic and diastolic blood pressure, body-mass index, and abdominal perimeter (P<.001). Conversely, we did not find a significant correlation between total cholesterol and c-IMT (Pearson coefficient, r=-0.03; P=.88). SCORE values were positively (r=0.52) and significantly (P<.001) correlated with c-IMT.
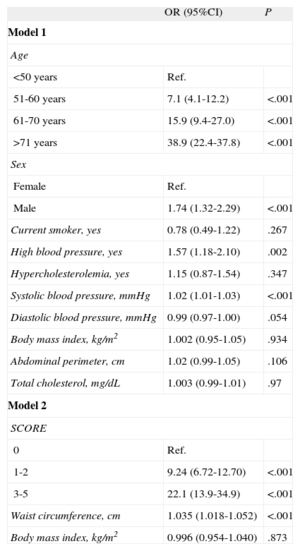
We then performed a multivariate logistic regression analyses, taking carotid atherosclerosis (presence of carotid plaque) as the dependent variable (Table 2). Age, sex, and systolic blood pressure were the 3 variables positively and significantly influencing the presence of carotid atherosclerosis in our population. Participants older than 71 years had a risk of carotid atherosclerosis 39 times greater than participants younger than 50 years (P<.001). Remarkably, we also found a significant increased risk at younger ages; participants 51 to 60 years old have a 7.1-fold greater risk than individuals aged 50 or younger. Men have 1.7 times higher risk than women. We did not find any significant relationship with smoking, hypertension,or hypercholesterolemia. Sex (male vs female) and higher systolic blood pressure were associated with a higher risk of carotid atherosclerosis (odds ratio=1.02; 95% confidence interval [95%CI], 1.01-1.03; P<.001). When all the individual cardiovascular risk factors were replaced by the SCORE value, there was also a significant association with the presence of carotid atherosclerosis (Table 2).
Multivariate Analyses of Carotid Atherosclerosis
| OR (95%CI) | P | |
| Model 1 | ||
| Age | ||
| <50 years | Ref. | |
| 51-60 years | 7.1 (4.1-12.2) | <.001 |
| 61-70 years | 15.9 (9.4-27.0) | <.001 |
| >71 years | 38.9 (22.4-37.8) | <.001 |
| Sex | ||
| Female | Ref. | |
| Male | 1.74 (1.32-2.29) | <.001 |
| Current smoker, yes | 0.78 (0.49-1.22) | .267 |
| High blood pressure, yes | 1.57 (1.18-2.10) | .002 |
| Hypercholesterolemia, yes | 1.15 (0.87-1.54) | .347 |
| Systolic blood pressure, mmHg | 1.02 (1.01-1.03) | <.001 |
| Diastolic blood pressure, mmHg | 0.99 (0.97-1.00) | .054 |
| Body mass index, kg/m2 | 1.002 (0.95-1.05) | .934 |
| Abdominal perimeter, cm | 1.02 (0.99-1.05) | .106 |
| Total cholesterol, mg/dL | 1.003 (0.99-1.01) | .97 |
| Model 2 | ||
| SCORE | ||
| 0 | Ref. | |
| 1-2 | 9.24 (6.72-12.70) | <.001 |
| 3-5 | 22.1 (13.9-34.9) | <.001 |
| Waist circumference, cm | 1.035 (1.018-1.052) | <.001 |
| Body mass index, kg/m2 | 0.996 (0.954-1.040) | .873 |
95%CI, 95% confidence interval; OR, odds ratio.
Results according to different SCORE values and adjusted by decades of life are displayed in Figure 2. The prevalence of carotid plaques increased significantly with higher SCORE values and decades of life. There were no participants older than 61 years with SCORE values of 0. Similarly, there were no participants below 60 with SCORE risk between 3 and 5. However, we did diagnose carotid atherosclerosis in 35 participants with SCORE values of 0: 12 (2%) participants were younger than 50 and 23 (15.4%) were in the next age group (51-60 years). Furthermore, we found 173 (53.1%) individuals with carotid plaques in the intermediate cardiovascular risk group. In this group of participants scoring 1 or 2, we found carotid atherosclerosis in each group of age (overall number of patients with carotid plaques, 424 [31.2%]).
We have to highlight that the overall prevalence of carotid plaques in the 2354 participants studied was 25.1% (592 participants with carotid plaques at low-to-intermediate SCORE risk).
DISCUSSIONCVD are the leading cause of death in industrialized countries and many of them are atherosclerosis-related events. The aim of the current study was to quantify the burden of atherosclerosis (measured by c-IMT and the presence of carotid plaques) noninvasively in a group of apparently healthy individuals with low-to-intermediate cardiovascular risk according to SCORE. The main result is that 25.1% of individuals have carotid plaques. We have to highlight that these participants were not diagnosed of diabetes or previous CVD. In the multivariate analyses, variables significantly related to the presence of carotid atherosclerosis were age, male sex, and systolic blood pressure. Furthermore, SCORE risk was also significantly related to carotid atherosclerosis. These results are partially in accordance with published manuscripts. In a cross-sectional study, Postley et al.18 included 715 individuals with low-to-intermediate Framingham risk, and carotid and femoral arteries were screened. Prevalence of plaques was 32.8% and age, maleness, and dyslipidemia were among the significantly related variables. In the similar Northern Manhattan Study, 1445 participants presented a prevalence of subclinical CVD of 35%, including carotid atherosclerosis and left ventricular hypertrophy.19 Rundek et al.20 reported a prevalence of carotid plaques of 58%, although 459 (21%) of the participants had a previous cardiovascular event, which might affect the higher prevalence of carotid plaques observed in this study. Conversely, several reports have a lower prevalence of carotid plaques than those observed in our population. The CARMELA (Cardiovascular Risk Factor Multiple Evaluation in Latin America) study investigators reported a prevalence of carotid plaques of 8% in 7 different Latin American Countries, including 11550 participants. Potential explanations for these differences include the different rate of atherosclerosis development, since c-IMT was significantly lower than in our study (0.65mm vs 0.74mm, respectively). Further, a geographical influence has been described in c-IMT and plaque (Asians reported to have less c-IMT than Latin Americans), although these differences were not statistically significant in the multivariate analyses.21 In Spain, 2 studies, one in apparently healthy participants14 and a population-based study13, have been recently published. Both studies were aimed at the study of c-IMT and the associated normality range values and clinical factors. Both studies identified age as the strongest predictor in c-IMT, but the presence of carotid plaques had not been reported. In that regard, Our study provides new information on carotid atherosclerosis as a whole, taking into account the c-IMT values along with the presence of carotid plaques, a known predictor of CVD risk 22.
These previous reports, however, unanimously evidenced a clear dissociation between risk scoring and the presence of atherosclerosis detected by ultrasonography, since many participants at low-to-intermediate cardiovascular risk presented with atherosclerosis. We have to highlight that risk scoring (Framingham, SCORE, etc) are aimed at the identification of participants at risk of having a cardiovascular event, and not at the identification of atherosclerosis. However, participants with atherosclerosis should be identified as having a high cardiovascular risk. Indeed, blood pressure guidelines identified the presence of carotid atherosclerosis as a sign of poor prognosis in the hypertensive population.2 Moreover, population-based studies have clearly identified the presence of carotid atherosclerosis as an independent variable in the prediction of cardiovascular events, both coronary heart disease and stroke. In a recent manuscript, Davidsson et al.23 report that the odds ratio of cardiovascular events for those with a carotid plaque was 2.09 (95%CI, 1.05-4.16; P=.03) in a multivariate analysis of 391 males from Sweden. Further, the presence of carotid plaques was associated with a 2.9 (95%CI, 1.22-7.07) times higher risk of cardiovascular events, in an observational study of 767 healthy Mediterranean participants.24 The predictive value of c-IMT for cardiovascular events is more controversial. A measured c-IMT difference of 0.1mm when corrected for age and sex yields a 10% to 15% increase in future cardiovascular events and an increased risk of stroke (13%-18%)25. However, a recently published meta-analysis by Lorenz et al. did not find an association between progression of c-IMT and cardiovascular events.23
Finally, the additive value of including c-IMT in traditional risk factors improves predictive power. Sensitivity, specificity, and ROC (receiver operating characteristic) curves are enhanced after carotid ultrasound results are incorporated into the equation.26 According to the recently published MESA data,27 with the combination of c-IMT and coronary calcium calcification scores added to traditional risk factors, the predictive model acheived the highest efficiency for ROC curves analyses (area under the curve from 0.77 (0.74-0.80) to 0.81 (0.78-0.84). Although the preponderance of clinical evidence supports the use of carotid ultrasound as a powerful, additive surrogate marker for cardiovascular risk, today, there is no prospective, randomized, controlled clinical trial in which c-IMT/plaque serves as the initial, threshold screening test for detection and prediction of CVD.28 Theoretically, the identification of carotid atherosclerosis should be followed by a more strict control of the classical risk factors, and this approach might be followed by a significant decrease in the incidence of cardiovascular events. However, this is a hypothesis that should be tested early. Treating with rosuvastatin healthy, middle-aged participants with a Framingham risk score <10% but with carotid atherosclerosis was tested in the METEOR clinical trial.29 In this trial, participants assigned to receive 40mg of rosuvastatin had statistically significant reductions in the rate of progression of maximum c-IMT over 2 years. Similar prospective trials aimed at the identification of participants with atherosclerosis, compared with the traditional approach, are highly warranted.
LimitationsOur results have several limitations. Cholesterol levels were not measured in a fasting state. However, a recent paper reveals that fasting times showed little association with lipid subclass levels in a community-based population, which suggests that fasting for routine lipid levels is not necessary.30 Similarly, the diagnosis of diabetes and the concomitant medication were self-reported, adding complexity to the study conclusions. This is not a population-based study where participants have been selected randomly. Although investigators did not influence the participation (participants voluntarily accept to be screened), the way the study was conducted might represent a potential limitation in the external validity of the results.
The c-IMT was measured on-line with the patient seated, with a 45o angle in both carotid axis and in the posterior common carotid wall, using the semi-automated software AutoIMT®. This might be interpreted as a limitation, but an experienced reader (B.C.) re-analyzed 10% of the images, randomly and off-line, and the intra-class correlation coefficient was 93%. Further, results concerning c-IMT and its related variables are plausible; consequently, the results of this research clearly advocate the feasibility of carotid ultrasound in performing campaigns of atherosclerosis screening and cardiovascular prevention. Furthermore, the diagnostic assessment for hypertension and dyslipidemia was documented with a questionnaire, and no data on prescribed medications or treatment compliance were recorded.
CONCLUSIONSAs CVD remain the number one killer in the developed world, additional efforts to better define preclinical disease need to be developed and adopted. Carotid ultrasound assessment of preclinical atherosclerosis is valued for the assessment of atherosclerosis and in predicting CVD, and according to our data 25.1% of apparently healthy participants at low-to-intermediate cardiovascular risk according to SCORE presented with carotid plaques. These results are encouraging. Now it may be time to test the first-line efficiency and accuracy of using carotid ultrasound as a predictor of CVD in a large, prospective, randomized clinical trial.
CONFLICTS OF INTERESTNone declared.
We are especially thankful to UDETMA components for their involvement in the current research project. GE Healthcare Spain was actively involved in the logistics and in providing the ultrasound portable devices (Sonia Mora, Mario Lois and Juan Antonio Beceiro). We also thank the Spanish Society of Cardiology and the Spanish Heart Foundation for the organization of the screening program.