INTRODUCTION
Cardiology is the medical discipline or specialty responsible for the prevention, diagnosis, and treatment of cardiovascular disease. As this is the major cause of morbidity and mortality in Spain and the European Union,1 cardiology professionals have, with respect to other medical specialists, an additional moral authority and responsibility derived from the relevance for society of an excellent performance in combating cardiovascular disease. Hence the importance of keeping up with the rapid transitions that are currently taking place at the social, administrative, educational, health care, and professional levels, transitions that necessarily generate novel contexts for the practice of cardiology and for its professionals.
At the end of 2005, the Spanish Society of Cardiology (SSC), by virtue of its leadership role in combating cardiovascular disease, decided to undertake a project, applying a synthetic approach to the process matrix, involving the professionals in cardiology and in other medical specialties, the health care administrations, the pharmaceutical industry, and biotechnology companies, the institutions, the patients and the general population; these processes will ultimately play a role in the development of the field of cardiology, in the work of the professionals in this specialty and, in general, in health care in the area of cardiovascular disease.
Some of the conclusions resulting from this initiative were published in the Madrid Declaration,2 a consensus document arising from the European Conference on the Future of Cardiology held in 2006 in Madrid, Spain. This document included, along general lines, the problems identified by a group of experts from the European Society of Cardiology and from the SSC that would need to be addressed by European cardiology over the next 15 years. For the purpose of applying and adapting this analysis to our specific circumstances, the Executive Committee of the SSC created an ad hoc expert group (Appendix) to carry out an in-depth debate concerning the questions that were considered to be top priorities. In the selection of the members of said committee, in addition to appointing people who were recognised experts in the subject, there was a representation of three age groups from the cardiology community, as well as from the different coreas of activity within the specialty. The present document includes the consensus opinions of that group, generated in periodical meetings held in 2006 and 2007, and based on the evidence in the available literature on the subjects dealt with. The document was reviewed by representatives of the scientific sections, working groups and SSC committees listed in Appendix. Once their comments had been incorporated, the reviewers received a copy of the final document for the purpose of obtaining their definitive approval. Two central issues were debated: the updated definition of the field of cardiology, taking into account our general population, and the profile that the clinical cardiologist will need to have in the novel clinical settings. Thus, this document does not include discussions relative to subjects that, despite their acknowledged importance, have already been studied by other ad hoc committees (for example, the availability of cardiologists in Spain, which was analyzed by a group of SSC experts, whose findings were published in this same journal3) or those that, given their far-reaching implications, are better suited for presentation in the Madrid Declaration as a whole and in the documents cited therein (such as epidemiological trends or problems in cardiovascular research).
IMPORTANCE OF DEFINING THE ROLE OF CARDIOLOGISTS WITHIN THE CURRENT CONTEXT OF THE SPECIALTY
As in other countries,4,5 there is a considerable imbalance between the supply of and demand for cardiologists in Spain at the present time.3 The situation will tend to become worse over the coming years, partly as a result of epidemiological factors that favor a predominant role for cardiovascular diseases, but also due to sociological factors, including the high proportion of active cardiologists who are nearing the age of retirement, a growing demand for specialized care and an increasing complexity of the process of care provision. The growing number of techniques that occupy the activity of the limited number of cardiologists, and constitute the preferences of the youngest professionals, will also influence the availability of specialists. These are 2 factors that may jeopardize the work of the clinical cardiologist, an occupation that could remain vacant and should be taken up by other specialists. This circumstance should be analyzed in light of a number of studies that have compared different indicators of the performance of cardiologists with that of internal medicine or primary care specialists.6-9 Along general lines, these studies point out that the care provided by cardiologists is superior in terms of their greater knowledge and closer adherence to clinical practice guidelines,10,11 higher diagnostic yield, and better adaptation of the indications for diagnostic tests,12-15 lower rates of in-hospital morbidity, and mortality and fewer hospital readmissions.6-9,16 Nevertheless, it should be kept in mind that, in some of these studies, there may be differences in the case mix that could imply a greater complexity of the patients treated by internists, a circumstance that might influence one or more of the indicators employed,16,17
Moreover, at the present time, changes are being introduced in health care practice in general that should be briefly mentioned. Health care administrations are committed to improving the rationality, control and yield of their financial, technical, and human resources. In the attempt to obtain the maximum efficiency and satisfy an informed and demanding middle class, health care has become oriented in line with diagnostic and therapeutic approaches in which different specialties cooperate around a common disease or process, and the patient is the center of activity. The commitment of the administration to these interdisciplinary units also has an economic justification: a large part of the expenditure is attributed to the lack of coordination between departments and specialties and between primary care centers and hospitals, to an excessive number of requests for and duplication of diagnostic tests and to an inadequate follow-up of the chronically ill patient, which increases the incidence of decompensation of the disease, resulting in hospital admission. The scientific societies of different specialties have since assumed the irreversibility of this process and prepare consensus documents addressing strategies for facilitating multidisciplinary work.18 In this new model, the figure of the leader-coordinator responsible for the horizontal integration among specialties will be key for the administration.
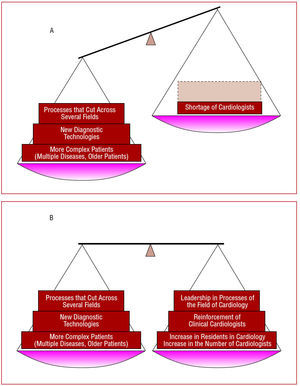
In line with the circumstances described above, the present number of cardiologists would be insufficient to treat all the patients with cardiovascular diseases, despite the existence of scientific evidence that indicates that cardiology is the specialty best prepared to treat them.6-16 The tension existing in this paradoxical situation will tend to increase owing to the interaction of the aforementioned phenomena. Figure 1 illustrates how these circumstances will contribute to upsetting the balance of the central role of cardiology in the treatment of cardiovascular disease. The delimitation of the professional field of the cardiologists is crucial in this situation in order to: a) quantify the future demands for specialists; b) establish those medical care processes that should be headed by a cardiologist; and c) develop future curricula adapted to the novel clinical settings.
Figure 1. A: trend towards an imbalance in the cardiovascular field between the demand for care created by the new health and social care contexts and the availability of specialized care, reduced by the shortage of cardiologists. B: possible mechanisms for recovering the balance.
SPANISH SOCIETY OF CARDIOLOGY RECOMMENDATIONS CONCERNING THE ROLE OF CARDIOLOGISTS SETTING
For the purpose of establishing what the clinical processes should be and how we should participate in them, the Expert Committee and scientific section of the SSC have prepared an account of the various clinical areas that define the field of cardiology in the different diseases and have drawn up a series of recommendations in this respect. The importance of maintaining the spirit of cooperation and the absence of confrontation among the specialists that necessarily have to work with patients with cardiovascular disease is acknowledged.16 The authors and reviewers of the present document are aware of the fact that the contexts in which cardiological care is provided vary considerably depending on the level of care, the institutional tradition, etc. The recommendations do not constitute a value judgment with respect to these variations, but seek a greater rationality in future specialized care in cardiovascular diseases. The cardiologist will sometimes have to play the role of the cardiovascular expert (drawing up guidelines or protocols) or that of leader and consultant for specialized units (administration, coordination, etc), without attempting to be directly responsible for all the health care tasks in said field.
Cardiovascular Risk
A number of studies have demonstrated that, as compared to other specialists, cardiologists are more active in primary and secondary cardiovascular prevention.10,11,19 A consensus document drawn up by European gynecologists and cardiologists that stresses the joint effort of the 2 specialties during the perimenopausal period has recently been published.20 Likewise, a joint effort between cardiologists and endocrinologists in multidisciplinary units for cardiovascular prevention in diabetic patients has been proposed.21 The SSC recommendation is that, in our general population, the cardiologist participate together with all the other specialists, especially with primary care physicians, in the prevention of cardiovascular risk (hypertension, dyslipidemia, diabetes, obesity, smoking) and in the organization and administration of programs established to address this issue.21,22 He should also assume the responsibility of the secondary prevention and early diagnosis of cardiovascular disease, increasingly facilitated by new diagnostic techniques. Given its scientific and institutional importance, the SSC and the Spanish Heart Foundation should take charge of the information relative to cardiovascular risk provided to specialists and to our general population.
Ischemic Heart Disease
Ischemic heart disease is one of the fields in which the excellence of the cardiological care, as compared to that of other specialties, is most clearly established (see, for example, the systematic review of Go et al7 of 13 studies dealing with this subject). Along general lines, the available evidence indicates that cardiological management is related to a better diagnostic yield in the tests performed, a higher incidence of the use of reperfusion therapy in acute myocardial infarction, more frequent use of catheterization and percutaneous or surgical coronary revascularization, greater adherence to the clinical practice guidelines for secondary prevention and lower rates of in-hospital and out-of-hospital morbidity and mortality. Moreover, it has been demonstrated that the intervention of cardiologists in the treatment is beneficial both when they are directly responsible for the patients and when they serve as consultants to other specialists.23,24 The SSC recommendation is that, in tertiary level hospitals, the care of any patient with ischemic heart disease should be the in the hands of the cardiologist. At other health care levels, he should head the management of these patients, working via a network with tertiary level centers. The cardiologist should be responsible for patients with acute coronary syndrome. He should be responsible for the intermediate coronary care units, in agreement with the recommendation of a specific document recently published in this journal.25 It is considered that the cardiologist should establish the basis for the follow-up of the patient with chronic ischemic heart disease. Finally, he should participate in drawing up guidelines for the health care process and in establishing recommendations made particularly for the setting of our health care system, as has been the case in the Ischemic Heart Disease Strategic Plan of the Spanish Ministry of Health.
Heart Failure
A number of studies have reported that the management of patients with heart failure by cardiologists is associated with better results than that observed in other specialties,7,8 although, in some cases, this circumstance may be due to a greater complexity of the population treated by the latter.17 The prevalence of this disease and the health care burden associated with it have led to the debate as to which specialist should be responsible for its treatment.26 The opinion of the SSC is that the cardiologist should take responsibility for the care of heart failure patients, although to different degrees depending on the disease stage. In stage A (risk factors but no structural disorder of the heart), guidelines and protocols that can be applied by both cardiologists and other specialists should be made available.
The patient with stage B or C heart failure (structural disorder of the heart, with or without heart failure) should be the responsibility of the cardiologist if heart failure is the predominant disease, regardless of the age of the subject. Treatment of stage D heart failure (heart failure that requires specialized treatment) is invariably the province of the cardiologist, whose activity in these cases is increasingly carried out in the context of specialized units.27 In these units, which we have found to produce excellent results,28 the cardiologist will act as coordinator of the interdisciplinary heart failure programs.
Infectious Endocarditis
Infectious endocarditis is a serious and complex disease that should be treated in hospitals with experienced staff.29 The SSC recommends that, although different professionals intervene in the care of these patients (specialists in infectious diseases, microbiologists, surgeons), the cardiologist should direct the diagnosis and treatment. This point of view is based on the fact that the cardiologist is the specialist best prepared to perform an emergency echocardiographic evaluation in any patient in whom endocarditis is suspected, in order to properly assess and treat the hemodynamic complications and establish the surgical indications on which the survival of patients with this disease depends.
Acute Aortic Syndromes
The clinical presentation of acute disease of the ascending aorta is frequently derived from the associated cardiac complications. The recommendation of the SSC is that the cardiologist direct the care process which, in virtually every case, includes the specialties of cardiac surgery and radiology.30 The development of percutaneous techniques for the treatment of aortic dissection, far from making it the exclusive province of the cardiologist, will further consolidate the multidisciplinary approach in the diagnosis and treatment of this disease.31,32
Pulmonary Thromboembolism
A diagnostic study of suspected pulmonary thromboembolism is often performed in patients admitted to intensive care units, emergency departments, or internal medicine wards. The cardiologist acts as a consultant in a large number of cases: in a recent registry, echocardiography was the diagnostic imaging technique most frequently utilized (91% of the cases).33 Together with the specialists in these departments, the cardiologist should participate in the care of these patients, collaborating with the radiology department (spiral computed tomography) and, less frequently, with the nuclear medicine department (ventilation-perfusion scan).
Pulmonary Hypertension
In the current context, the diagnosis and treatment of pulmonary hypertension is usually performed not only in the cardiology department, but in pneumology, rheumatology, and internal medicine departments, as well. It is a disease that frequently requires an interdisciplinary effort in which the cardiologist should always participate together with other specialists34 and take on a leadership role in those cases in which the pulmonary hypertension is of primary origin or of cardiac etiology.
Cardiac Arrhythmias and Syncope
Cardiac arrhythmias indisputably pertain to the field of cardiology, and we were unable to find publications comparing their management by different specialties. There is consensus among the authors and reviewers of the document in that patients with clinically relevant cardiac arrhythmias should be treated exclusively by cardiologists. In the specific case of atrial fibrillation, 2 reports have demonstrated that cardiologists were more successful in the administration of antithrombotic therapy than the internists or family physicians24,35 and that, in addition, they played a key role in the diagnosis and management of these patients. The SSC considers that the cardiologist should take the lead in the medical care of this entity when the clinical condition or disease of the patient with atrial fibrillation indicates it to be necessary. The widespread use of the techniques of ablation and isolation for this arrhythmia will very likely increase the demand for the study of a greater number of patients with atrial fibrillation on the part of cardiologists. Finally, the indication for, implantation of and follow-up of devices for the control of arrhythmias (pacemakers, resynchronizers, automatic defibrillators) should be the province of the cardiologist, in collaboration with surgeons, when necessary.
Congenital Heart Disease
The cardiologist will work in collaboration with specialists in obstetrics and pediatrics in the management of prenatal, neonatal, and childhood congenital heart diseases. Likewise, the coordination of adult congenital heart disease units, increasingly necessary because of the longevity of these patients, should be studied, as well as the need for interaction between pediatric and adult and pediatric cardiologists (who are not familiar with the anatomical and functional complexity of congenital heart diseases) and heart surgeons.
IMPORTANCE OF THE ROLE AND PROFILE OF CLINICAL CARDIOLOGISTS IN NEW HEALTH CARE SETTINGS
Parallel to the discussion concerning the field of cardiology in the new health and social care contexts, the importance of the role of the clinical cardiologist took up a great part of the debate involved in the preparation of this document. The analysis carried out by the SSC extends and individualizes for our general population some of the considerations previously outlined in the Madrid Declaration2 with respect to the possible threats affecting the role of the clinical cardiologist.
First, the influence of the introduction of new technologies in cardiology and in medicine in general was considered. To reach a level of proficiency in the use of these technologies, and to obtain certification of the necessary level of excellence in their utilization, the professional often has to devote himself exclusively to a cardiology subspecialty.36 The excessive fragmentation of cardiology that follows from this trend, in accordance with the aforementioned circumstances, may result in a decrease in the traditional clinical activity of the cardiologist, which could reach the point in which it would be substituted by that of other specialties.37,38 The new generations of cardiologists aspire to achieve mastery of most novel techniques, which is associated with a greater possibility of recognition and professional opportunities, and take on the challenge of the required training period, knowing that this proficiency adds to their professional qualification. This trend is not offset by any policy of promotion and stimulus of the figure of the clinical cardiologist, which is understood to be someone who devotes most of his health care activity to patient management and/or the coordination of health care processes. This would explain why in a recent survey, carried out in the United States among 252 final-year cardiology residents, only 16% of them planned to devote their practice exclusively to general clinical care of cardiology patients.39,40 In this scenario of gradual "abandonment" of clinical cardiology, in the United States, a short-format specialty has been proposed that basically seeks to cover the health care vacuum in the field of cardiovascular disease.39 Another trend we are observing as a result of the lack of cardiologists in Spain is the incorporation of other specialists to functions that pertain to the field of cardiology.
The Madrid Declaration2 pointed out the fact that the future of the specialty would require making the process management of the hospital compatible with the potentiation of the role of the clinical cardiologist. The document also stressed the expected increase in the complexity of patients with cardiovascular diseases, who would have more concomitant diseases and a more advanced mean age. At the present time, the training of specialists is based on rotations that take into account the structure and care needs of the existing departments, but not the profile of the specialist that in all likelihood will be necessary in the new integrated health services. In this respect, it is important to consider the Core Curriculum for the general cardiologist41 proposed by the European Society of Cardiology in 2006, the purpose of which was to serve as the basis for uniform training of all European cardiologists. The Core Curriculum bases training in each of its topics on a triad of knowledge, skills and attitudes that every cardiologist should possess in his different areas of activity.
The figure of the clinical cardiologist that will serve as the cornerstone of future cardiovascular care will be that of a cardiologist with specific training for the role described above: he should have a greater knowledge of diseases frequently associated with cardiovascular disease (diabetes, renal failure, genetics, etc), be qualified to participate in the management of all the cardiac disorders, possess knowledge of administration and be capable of coordinating and communicating with different specialists, as well as those peers who perform tests or interventions. The aim is to prepare him to achieve a key role both in taking the lead in processes that involve several areas including that of cardiology and in caring for the growing population of cardiovascular patients. As has been shown in previous studies, the care of cardiovascular patients benefits from the support of the cardiologist both as the professional directly responsible for that care and as a cardiovascular consultant.23,24
This revaluation of the figure of the clinical cardiologist will prove to be key in permitting the constitution of his field as a competitive professional option that can be assumed by the new generations of specialists in cardiovascular medicine. It is important to understand that, in the eyes of the public, the disappearance or reduction of the role of the clinical cardiologist would have a critical effect on the perception that society has of cardiology as a specialty. This is because the only figures clearly recognized as professionals specialized in heart diseases are the clinical cardiologist and the cardiovascular surgeon, and these figures are the repository of the prestige and soundness of the specialty in the public mind. The authors and reviewers of the present document acknowledge that, on the other hand, at the present time, the system does not provide the means for this much needed motivation or revaluation of the clinical cardiologist, and that the training syllabus for the clinical cardiologist should be adapted as soon as possible to these changes, possibly reducing the current lengths of rotations in certain areas (electrophysiology and hemodynamics, for example) and promoting others in which their training should be more complete.
RECOMMENDATIONS OF THE SPANISH SOCIETY OF CARDIOLOGY CONCERNING THE FUNCTION AND PROFILE OF THE CLINICAL CARDIOLOGIST
1. In order that the training in cardiology be uniform with respect to the rest of the European Union, the specialized training program should closely follow the guidelines of the Core Curriculum developed by the European Society of Cardiology.41 Its proposal of the triad of knowledge, skills and attitudes for assessment account is considered to be a positive approach.
2. In this respect, the syllabus of the clinical cardiologist should be adjusted permanently to address the ever-greater exigencies of a society that is increasingly demanding and well informed.
3. The innovation and development of ways to motivate and revaluate the figure of the clinical cardiologist is crucial to making this professional option more attractive and competitive. For this purpose, the syllabus must also include specific contents that distinguish him and qualify him for his future occupation. For example, among other things, the clinical cardiologist should receive training in team leadership (group dynamics and relationship skills), should develop health care management capabilities (at the level of units, departments or institutions), should have a broader knowledge of certain areas of internal medicine that enable him to serve as a consultant, should receive specific training in bioethics in order to perform effectively on health care ethics or clinical research ethics committees and should have training and skills that enable him to take part in expert assessments involving matters related to the specialty of cardiology. Among these forms of motivation, we should also consider the possibility that the clinical cardiologist experience rotations in the subspecialties in order to ensure his management skills and a deep, updated knowledge of the different fields of the specialty. In the potentiation of the figure of the clinical cardiologist, together with the administration and other agents involved, the department heads themselves should also assume part of the responsibility. Thus, the figure of the clinical cardiologist should in no case be considered that of the cardiologist "by default," with no specific preparation.
4. During the period of residency, the cardiologist in training should learn everything concerning the subject of the clinical relationship, while studying the indications for, interpretation of and performance of invasive and noninvasive diagnostic tests, under the supervision and guidance required in each case.
5. Transthoracic echocardiography is considered to be a basic test that every cardiologist should master, with the exception of special studies.
With respect to the clinical cardiologist, proficiency in this technique is important for the optimization of his performance and ability to resolve questions in outpatient consultations.
EPILOGUE
The objective of the present document is to provide consensus opinions concerning the subjects addressed, confident that ultimately it will be the citizens who benefit from them through the improvement of health care practices and policies on the part of the different agents involved. The document thus expresses, in agreement with its motto, the commitment of the SSC to cardiovascular health.
ACKNOWLEDGMENTS
The authors acknowledge the valuable secretarial assistance of Paquita Burgos and Sharon Legendre.
APPENDIX. REVIEWERS OF THE DOCUMENT
Scientific Sections of the Spanish Society of Cardiology
Alfredo Bardají Ruiz, Ischemic Heart Disease and Coronary Units
Camino Bañuelos de Lucas, Geriatric Cardiology
Fernando Arribas Ynsaurriaga, Electrophysiology and Arrhythmias
José Martínez Ferrer, Cardiac Stimulation
Josepa Mauri Ferré, Hemodynamics and Interventional Cardiology
Juan Carlos Paré Bardera, Cardiac Imaging
Juan F. Delgado Jiménez, Heart Failure, Transplantation and Other Therapeutic Alternatives
M. Carmen de Pablo y Zarzosa, Preventive Cardiology and Rehabilitation
Nekane Murga Eizagaechevarría, Clinical and Outpatient Cardiology
Rosa María Perich Durán, Pediatric Cardiology and Congenital Heart Disease
Vicente Bertomeu Martínez, Hypertension
Working Groups of the Spanish Society of Cardiology
Alfonso del Rio Ligorit, Dyslipidemia
Antonio Salvador Sanz, Cardiovascular Thrombosis
Araceli Boraíta Pérez, Sports Cardiology and Physical Activity
Arturo Evangelista Masip, Aortic Disease
Esteban García Porrero, Secondary Prevention and Cardiac Rehabilitation
Felipe Hernández Hernández, Intracoronary Diagnostic Techniques
Francisco García Gallego, Cardiac Histopathology
Gonzalo Baron Esquivias, Syncope
José A. Jurado López, Nuclear Cardiology
José Luis Moya Mur, Cardiovascular Magnetic Resonance-Cardiovascular Computed Tomography
José Luis Palma Gámiz, Heart and Diabetes
Josep Lluís Mont Girbau, Cardiac Resynchronization
Juan Carlos Kaski, Inflammation and Cardiovascular Disease
Juan Cosín Sales, Experimental Cardiology
M. Pilar Escribano Subias, Pulmonary Circulation
Mauel Abeytua Jiménez, Smoking Habit
Manuel Penas Lado, Hypertrophic Cardiomyopathy
Milagros Pedreira Pérez, Cardiovascular Diseases in Women
Rafael Peinado Peinado, Implantable Cardioverter-Defibrillator
Societies Affiliated with the Spanish Society of Cardiology
Bartolomé Vallbona Adrover, Society of Cardiology of the Balearic Islands
Ángel Llácer Escorihuela, Society of Cardiology of Valencia
Concepción P. Suárez Suárez, Society of Cardiology of Asturias
Fernando Olaz Preciado, Society of Cardiology of the Basque Country-Navarre
Germán Pérez Ojeda, Society of Cardiology of Castile-Leon
Luis Escosa Royo, Society of Cardiology of Aragon
Luis F. Pastor Torres, Society of Cardiology of Andalusia
Manuel García García, Society of Cardiology of Galicia
Marcelino Jesús Montero Plaza, Society of Cardiology of Extremadura
Matías Pérez Paredes, Society of Cardiology of Murcia
Ruperto Vargas García, Society of Cardiology of the Canary Islands
Francesc Carreras Costas, Society of Cardiology of Catalonia
Ethics Committee of the Spanish Society of Cardiology
Manuel de los Reyes López
Fernando Martin Burrieza
Ginés Sanz Romero
Josep Brugada Terradellas
Cándido Martín Luengo
Rosa M. Lidón Corbi
National Specialty Committee
Alfonso Castro Beiras
Carlos Macaya Miguel
Francisco Fernández-Aviles
Gisela Teixidó i Turà
Juan M. Gual Julià
Juan M. Cinca Cuscullola
Luis Alonso-Pulpón Rivera
María Jesús Salvador Taboada
María Soledad Alcasena Juango
Rafael Vázquez García
Rafael Vidal Pérez
Tutor's Committee of the Spanish Society of Cardiology
Joan Antoni Gómez Hospital
Domingo A. Pascual Figal
Oscar Díaz Castro
Ernesto Lage Gallé
Ángel Sánchez Recalde
Residents' Committee
Ramón Bover Freire
M. Victoria Cañadas Godoy
Juan García de Lara
Pablo García Pavía
Gisela Teixidó i Turá
Rafael Vidal Pérez
The Spanish Society of Cardiology (SSC) project "The Future of Cardiology" was supported by an unrestricted educational grant from Bayer HealthCare.
Correspondence: Dr. J. Escaned.
Sociedad Española de Cardiología.
Nuestra Señora de Guadalupe, 5-7. 28028 Madrid. España.