Cardiovascular disease is the main cause of morbidity and mortality in Europe. The number of elderly people in Europe will increase over the next decades. Therefore, the relative and absolute numbers of elderly with acute coronary syndromes will steadily rise. As a result, the question about the best treatment strategy in these patients is becoming ever more important. The current guidelines of the European Society of Cardiology for patients with non-ST elevation acute coronary syndrome (NSTEACS) do not provide any definitive recommendations about the preferred approach in the elderly,1 but leave the decision more or less to the treating physician, indicating that “treatment decisions should be tailored according to estimated life expectancy, patient wishes, and co-morbidities.”
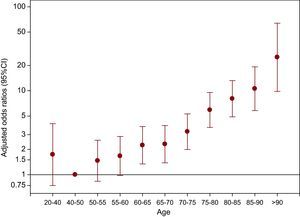
A very important subgroup is that of very elderly patients. Although there is no generally accepted cut-point to classify patients as very elderly, an age > 85 years might be appropriate to define the very elderly. Usually it has been proposed that symptomatic rather than prognostic considerations should guide the treatment strategy in the very elderly. Since the very elderly are included only rarely or not at all in randomized clinical trials, there is huge uncertainty about the best treatment strategy for them.2 In the past, this has resulted in reluctance to perform invasive procedures in elderly patients. Additionally, as the intervention itself conveys a higher risk for complications in the elderly, it has been universally observed that the use of invasive diagnosis and therapy decreases with advancing age. In an analysis of the European Heart Survey for Percutaneous Coronary Intervention3 the cut-off age for an increase in complications was 75 years, followed by a steady upward trend with advancing age (Figure 1). On the other hand all randomised studies have consistently shown that the benefit of an invasive strategy increases with a higher baseline risk, which is usually high in the very elderly.1 In the randomized TACTICS study, an invasive strategy was associated with improved outcome in elderly patients with NSTEACS.4 All of this leaves the treating physican with a high degree of uncertainty on what to do in the very elderly admitted to the hospital with NSTEACS.
Figure 1. Increasing mortality with increasing age in patients undergoing percutaneous coronary intervention in the Euro Heart Survey of Percutaneous Coronary Interventions registry. CI, confidence interval.
Interesting information about the use and outcome of an invasive strategy in the very elderly is reported in the manuscript by Villanueva-Benito et al. published in Revista Española de Cardiología.5 In a series of 228 patients with NSTEACS, 100 underwent an invasive strategy and 68 received percutaneous coronary intervention (PCI). Survival after 2 years was 58% with invasive vs 43.9% with conservative therapy. After adjustment for confounding factors, survival was significantly better in the invasive group. These results are in line with our own results in patients older than 75 years with NSTEACS, where we observed a reduction in 1-year mortality with an invasive strategy.6
One important consideration is that according to the Global Registry of Acute Coronary Events (GRACE) risk score almost all of the very elderly patients were moderate (20%) or even high risk (80%) patients, in whom current European Society of Cardiology guideline recommends an invasive strategy.1 However, it is well known that, paradoxically, the rate of patients undergoing an invasive strategy decreases with increased baseline risk.7 Certainly one important factor in deciding to withhold an invasive strategy is age; another factor is the presence of severe comorbidities. In the present study dementia was an important factor for a conservative strategy. There are a number of other factors, such as social activity or immobility, which were not documented but have a huge influence on our therapeutic strategies.
Another interesting finding of the present study was that PCI could be performed in 68% of the very elderly patients; this figure is not different from the rate of PCI in large studies with NSTEACS patients such as in the EARLY-ACS trial.8 On the other hand, the coronary artery bypass grafting usually indicated in about 10% of NSTEACS cases was not performed in any patient, despite the fact that three-vessel disease was observed in 40% of the cases. It seems that the invasive strategy is selected in an attempt to perform PCI of the culprit lesion rather than complete revascularization. The inhospital complications such as major bleeding, the need for transfusion, and stroke were not increased in the invasive group, while there was a nonsignificant trend towards a higher incidence of deterioration of renal function. These results indicate that an invasive strategy in selected cases does not harm the very elderly patient.
Of note is the relatively low use of guideline-recommended adjunctive therapy such as beta-blockers, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, and statins. Statins in particular, which have only a few contraindications, should be given in almost every patient with acute coronary syndrome. This undertreatment of the elderly has been observed in other analyses as well.9 Therefore there seems to be room for improvement upon conservative therapy in the very elderly with NSTEACS.
In summary, an invasive approach in very elderly patients with NSTEACS seems feasible and can improve midterm outcome. Further research is necessary to identify the subgroup of patients that might especially benefit from this strategy. Meanwhile, very elderly patients with good mental and social status should not be denied an invasive approach solely on the basis of chronological age.
Corresponding author: Klinikum Ludwigshafen, Med. Klinik B, Institut für Herzinfarktforschung Ludwigshafen an der Universität Heidelberg, Bremserstr. 79, D-67063 Ludwigshafen am Rhein, Germany. Uwe.Zeymer@t-online.de