Bystander assistance is decisive to enhance the outcomes of out-of-hospital cardiac arrest. Despite an increasing number of basic life support (BLS) training methods, the most effective formula remains undefined. To identify a gold standard, we performed a systematic review describing reported BLS training methods for laypeople and analyzed their effectiveness.
MethodsWe reviewed the MEDLINE database from January 2006 to July 2018 using predefined inclusion and exclusion criteria, considering all studies training adult laypeople in BLS and performing practical skill assessment. Two reviewers independently extracted data and evaluated the quality of the studies using the MERSQI (Medical Education Research Study Quality Instrument) scale.
ResultsOf the 1263 studies identified, 27 were included. Most of them were nonrandomized controlled trials and the mean quality score was 13 out of 18, with substantial agreement between reviewers. The wide heterogeneity of contents, methods and assessment tools precluded pooling of data. Nevertheless, there was an apparent advantage of instructor-led methods, with feedback-supported hands-on practice, and retraining seemed to enhance retention. Training also improved attitudinal aspects.
ConclusionsWhile there were insufficiently consistent data to establish a gold standard, instructor-led formulas, hands-on training with feedback devices and frequent retraining seemed to yield better results. Further research on adult BLS training may need to seek standardized quality criteria and validated evaluation instruments to ensure consistency.
Keywords
Bystander basic life support (BLS) is a well-known critical factor to improve prognosis of out-of-hospital cardiac arrest.1 The acknowledged role of education in overcoming knowledge and psychological barriers in this regard has placed laypeople BLS training in a priority position in clinical practice guidelines.2,3 Over the last decades, increasing interest in this field has been reflected in a growing number of studies reporting different BLS training approaches targeted at citizens, describing a wide range of training contents, formats, and tools. Nevertheless, this vast amount of emerging information has not served to define the optimal training strategy.
The ideal situation would be to train as many people as possible effectively with the least time and resources. However, the same educational objectives may or may not be achieved by different methods and, more to the point, with different levels of investment of time and resources. Nevertheless, there is no clear consensus on the minimum contents and instruments that should be included, the optimal length of training, or how the effectiveness of the intervention should be measured. This lack of consistent quality standards has made it difficult to recommend a particular approach to train citizens in BLS. Reviewing the state-of-the-art on the different reported training methods and weighing their success might be the first essential step to define the most effective formula. Therefore, the aim of this systematic review was to describe different reported BLS training methodologies for laypeople and to analyze their effectiveness in terms of practical skill acquisition and/or retention, identifying key educational aspects or, ideally, a gold standard.
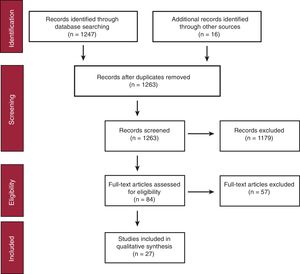
METHODSWe conducted a comprehensive search of the scientific literature in MEDLINE (PubMed), using a combination of MeSH terms and free text words (). The initial literature search was performed on January 2018 and was updated until July. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) recommendations were followed in this systematic review.4
Our PICO (Population, Intervention, Comparison, Outcomes)5 question was as follows: “Among adult laypeople (P), which is the best BLS training method (I) compared with no training or different methods (C) regarding practical skills acquisition and/or retention (O)?”.
Inclusion and Exclusion CriteriaParticipants: we included studies with adult (>18 years old) participants with no health care background or duty to assist, or recent BLS training (< 1 year previously). If data on last training diverged between participants, only studies with = 10% of the sample trained in the previous year were considered. Studies omitting data on previous training were considered ineligible.
Intervention: we considered all BLS training methods addressing the steps of the chain of survival, cardiopulmonary resuscitation (CPR) and/or use of a defibrillator (AED), provided their principal aim was to identify the effectiveness of 1 or more educational intervention.
Comparison: the intervention was compared with no training or with different BLS training methods.
Outcomes: main outcomes were a) performance of BLS skills, and/or b) BLS skills retention, measured at least once by means of a practical test with objective quality measurement. Secondary outcomes were attitudinal aspects, such as comfort with training and willingness to share knowledge and to use skills.
Type of study: we included original articles published in English or Spanish, adhering to international resuscitation guidelines released in 2005 or later. No minimum sample size was required.
Exclusion criteria: we excluded studies performed in health care professionals or first responders with a duty to assist, students from second year or onwards studying for health care-related degrees (Medicine, Dentistry, Nursing, or Pharmacy), scholars, and populations with distinctive characteristics that would preclude extending conclusions to the general population (such as psychological or physical impairment). Studies on advanced life support or pediatric BLS were excluded, as well as those not providing sufficient information about the intervention. Also excluded were studies with no practical and objective evaluation of posttraining skills, those focused on the analysis of the effect of rescuer-, victim- or scenario-related factors on BLS performance or those in which the effects could not be attributed to the intervention. Commentary and opinion papers, abstracts and animal studies, and those performed in undeveloped countries were also excluded.
Study Selection and Data ExtractionA first selection based on the titles and abstracts was performed and full text articles were independently assessed by 2 reviewers (E.R-R. and V.G-S.). If there were disagreements and no consensus after discussion, a third reviewer (C.A-G.) was consulted to reach a decision. The reference list of included studies was also searched. Data were independently extracted by the 2 reviewers based on minimum requirements recommended in the Inclusion and exclusion criteria,6 and were then cross-checked. Corresponding authors were contacted on 6 occasions due to missing or unclear data.
Quality AssessmentQuality was independently appraised by the 2 reviewers (E.R-R. and V.G-S.) using the Medical Education Research Study Quality Instrument (MERSQI),7 a numeric scale ranging from 5 to 18 to score education research studies, previously used in this field.8 Cohen's Kappa statistic was used to measure interrater reliability and level of agreement was stated according to Landis and Koch interpretation.9
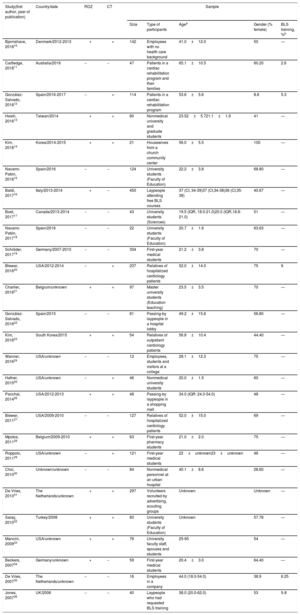
RESULTSType of Studies and Participants’ CharacteristicsThe initial search retrieved 1247 abstracts and 16 additional studies were identified by checking the list of references (Figure 1). Twenty-seven studies were finally included, with characteristics detailed in Table 1. Ten were individually randomized controlled trials and the sample size ranged from 12 to 450 participants. There was marked participation of University students (n=11), particularly of first-year health care-related degrees and Education Sciences, and a lesser presence of patients with a cardiac condition or their relatives (n=5). Participants were usually young and around 60% were women.
Type of Studies and Participants
| Study(first author, year of publication) | Country/date | RDZ | CT | Sample | ||||
|---|---|---|---|---|---|---|---|---|
| Size | Type of participants | Agea | Gender (% female) | BLS training, %b | ||||
| Bjørnshave, 201810 | Denmark/2012-2013 | + | + | 142 | Employees with no health care background | 41.0±12.0 | 50 | — |
| Cartledge, 201811 | Australia/2016 | -- | -- | 47 | Patients in a cardiac rehabilitation program and their families | 65.1±10.5 | 60.20 | 2.6 |
| González-Salvado, 201812 | Spain/2016-2017 | -- | + | 114 | Patients in a cardiac rehabilitation program | 53.6±5.6 | 8.8 | 5.3 |
| Hsieh, 201813 | Taiwan/2014 | + | + | 60 | Nonmedical university and graduate students | 23.52±5.721.1±1.9 | 41 | — |
| Kim, 201814 | Korea/2014-2015 | + | + | 21 | Housewives from a church community center | 56.0±5.5 | 100 | — |
| Navarro-Patón, 201815 | Spain/2016 | -- | -- | 124 | University students (Faculty of Education) | 22.2±3.8 | 68.80 | — |
| Baldi, 201716 | Italy/2013-2014 | + | -- | 450 | Laypeople attending free BLS courses | 37 (CI, 34-39)37 (CI,34-38)36 (CI,35-38) | 40.67 | — |
| Boet, 201717 | Canada/2013-2014 | -- | -- | 43 | University students (Sciences) | 19.5 (IQR, 18.0-21.0)20.0 (IQR,18.8-21.0) | 51 | — |
| Navarro-Patón, 201718 | Spain/2016 | -- | -- | 22 | University students (Faculty of Education) | 20.7±1.6 | 63.63 | — |
| Schröder, 201719 | Germany/2007-2010 | -- | -- | 334 | First-year medical students | 21.2±3.8 | 70 | — |
| Blewer, 201620 | USA/2012-2014 | -- | + | 237 | Relatives of hospitalized cardiology patients | 52.0±14.0 | 75 | 9 |
| Charlier, 201621 | Belgium/unknown | + | + | 97 | Master university students (Education teaching) | 23.5±3.5 | 70 | — |
| González-Salvado, 201622 | Spain/2015 | -- | -- | 81 | Passing-by laypeople in a hospital lobby | 49.2±15.6 | 56.80 | — |
| Kim, 201623 | South Korea/2015 | + | + | 54 | Relatives of outpatient cardiology patients | 56.8±10.4 | 44.40 | — |
| Wanner, 201624 | USA/unknown | -- | -- | 12 | Employees, students and visitors at a college | 28.1±12.3 | 75 | — |
| Hafner, 201525 | USA/unknown | -- | + | 46 | Nonmedical university students | 20.0±1.5 | 60 | — |
| Panchal, 201426 | USA/2012-2013 | + | + | 48 | Passing-by laypeople in a shopping mall | 34.0 (IQR: 24.0-54.0) | 48 | — |
| Blewer, 201127 | USA/2009-2010 | -- | -- | 127 | Relatives of hospitalized cardiology patients | 52.0±15.0 | 69 | — |
| Mpotos, 201128 | Belgium/2009-2010 | + | + | 63 | First-year pharmacy students | 21.0±2.0 | 75 | — |
| Roppolo, 201129 | USA/unknown | -- | + | 121 | First-year medical students | 22±unknown23±unknown | 48 | — |
| Choi, 201030 | Unknown/unknown | -- | -- | 84 | Nonmedical personnel at an urban hospital | 40.1±8.6 | 28.60 | — |
| De Vries, 201031 | The Netherlands/unknown | + | + | 297 | Volunteers recruited by advertising, scouting groups | Unknown | Unknown | — |
| Saraç, 201032 | Turkey/2008 | + | + | 60 | University students (Faculty of Education) | Unknown | 57.78 | — |
| Mancini, 200933 | USA/unknown | + | + | 76 | University faculty staff, spouses and students | 25-65 | 54 | — |
| Beckers, 200734 | Germany/unknown | + | -- | 59 | First-year medical students | 20.4±3.0 | 64.40 | — |
| De Vries, 200735 | The Netherlands/unknown | -- | -- | 16 | Employees in a company | 44.0 (18.0-54.0) | 38.9 | 6.25 |
| Jones, 200736 | UK/2006 | -- | -- | 40 | Laypeople who had requested BLS training | 38.0 (20.0-62.0) | 53 | 5-8 |
BLS, basic life support; CI, confidence interval; CT, controlled; IQR, interquartile range; RDZ, individually randomized (1:1); SD, standard deviation.
As shown in Table 2, 5 studies referred to the most recent 2015 resuscitation guidelines, 12 followed the 2010 recommendations and 10 adhered to the 2005 guidelines. Most studies included training in BLS skills (n=23) (including at least victim assessment and calling for help) and CPR (n=26), comprising chest compressions (CC) and ventilations in more than half of the studies (n=15). In contrast, AED use was taught in less than half of the studies (n=13). Instructor-led training was the most frequent alone, in combination or as opposed to self-instruction formulas, including video self-instruction kits or web-based methods (n=19). Long-duration methods prevailed (90-300minutes, n=13), followed by intermediate (40-60minutes, n=7), brief (15-20minutes, n=5) and very brief formulas (= 10minutes, n=5), and only 2 studies considered retraining. Most studies included hands-on practice (n=25) and feedback devices were used to guide CPR during training in nearly one-third of cases (n=9/26).
Training Methodologies
| Study (first author, year of publication) | Guidelines | BLS | CPR | AEDuse | Training method(average duration in minutes) | Hands-on practice | Feedback devicesa | Instructor: pupil ratio | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bjørnshave, 201810 | ERC 2010 | + | CC-V | + | 4-stage (demonstration, deconstruction, formulation, performance): instructor, manikin, AED trainer(240) | 2-stage (deconstruction, performance): instructor, manikin, AED trainer(233) | + | -- | -- | 1:6 | |||||||
| Cartledge, 201811 | ERC 2015 | + | CC-V | + | Instructor-led training with video and CPR training kit (manikin with feedback, AED trainer, BLS card)(35) | + | + | Unknown | |||||||||
| González-Salvado, 201812 | ERC 2015 | + | CC | + | Standard: instructor-led training (manikin, AED trainer), no retraining(20) | Instructor-led training (manikin, AED trainer)(20) | -- | + | -- | 1:10 | 1:10 | ||||||
| Retraining: 24 CPR rolling refresher sessions over 2 mo (manikin)(30) | 1:6 (retraining) | ||||||||||||||||
| Hsieh, 201813 | ILCOR 2010 | + | CC-V | + | Instructor-led training (video, manikin with feedback, AED trainer) followed by similar retraining (240) | + | + | 1:6 | |||||||||
| Retraining every 3 mo(83) | Retraining every 6 mo(83) | Retraining every 12 mo(83) | |||||||||||||||
| Kim, 201814 | AHA 2010 | + | CC | + | Standard BLS video, instructor-guided practice on manikin and debriefing(60) | Telephone-assisted BLS video, simulation and instructor-led debriefing(60) | + | -- | Unknown | ||||||||
| Navarro-Patón, 201815 | ERC 2015 | -- | CC | + | Instructor-led training(46) | Video-only self-instruction(10) | Instructor and feedback devices(8) | + | -- | -- | + | 1:10 course,1:2 practice | |||||
| Baldi, 201716 | ILCOR 2010 | + | CC-V | + | Instructor-led training(300) | Instructor and short feedback(300) | Instructor and long feedback(300) | + | -- | + | + | 1:5 | |||||
| Boet, 201717 | AHA 2010 | + | CC-V | + | Mastery learning: instructor-led training and practice on manikin until proficient performance, with continuous instructor feedback(108) | Time-based: instructor-led training and practice on manikin during a limited period of time, instructor feedback at the end(95) | + | -- | 1:3.5-4 | 1:4-5 | |||||||
| Navarro-Patón, 201718 | ERC 2015 | + | CC | -- | Dispatcher-assisted simulation, instructor-led training and practice on manikin(90) | + | -- | 1:6 | |||||||||
| Schröder, 201719 | ERC 2010 | + | CC-V | -- | Instructor-led training(240) | + | -- | Unknown | |||||||||
| Blewer, 201620 | AHA 2010 | + | CC | -- | Video-only self-instruction(22)b | Self-instruction kit (video, manikin)(22)b | -- | + | -- | N/A | |||||||
| Charlier, 201621 | ERC 2010 | + | CC-V | -- | Jigsaw model: instructor-led and peer-learning, manikin(54) | Instructor-led training, manikin(54) | + | -- | Unknown | ||||||||
| González-Salvado, 201622 | ERC 2015 | -- | CC | -- | Very brief instructor-led training, manikin with real-time visual feedback(5) | + | + | 1:1 | |||||||||
| Kim, 201623 | AHA 2010 | + | CC | -- | Patient centered education: instructor-led training with video, manikin and real-time feedback+phone call reminder at 2 wk(40) | Self-instruction kit (video, manikin)(40) | + | + | -- | Unknown | |||||||
| Wanner, 201624 | AHA 2010 | -- | CC | -- | Self-instruction (video, homemade manikin)(6)b | + | -- | N/A | |||||||||
| Hafner, 201525 | AHA 2010 | + | CCc | Unknown | Instructor-led training, video and manikin(150) | Instructor-led training, video, manikin and musical metronome (song)(150) | + | -- | + | Unknown | |||||||
| Panchal, 201426 | AHA 2010 | +c | CC | -- | Ultra-brief video self-instruction(1)b | -- | -- | N/A | |||||||||
| Blewer, 201127 | AHA 2005 | + | CC-V | -- | Self-instruction kit (video, manikin)(45) | + | -- | N/A | |||||||||
| Mpotos, 201128 | ERC 2005 | + | CC-V | -- | Introduction lecture, instructor-led training, manikin(180) | Introduction lecture, self-instruction kit (video, manikin with feedback)(no time limit)d | + | -- | + | 1:6 | N/A | ||||||
| Roppolo, 201129 | ERC 2005 | + | CC-V | + | Online training, manikin with feedback(120) | Online training, self-instruction kit (video, manikin)(135) | Instructor, video, manikin(270) | + | + | -- | -- | N/A | N/A | 1:6 | |||
| Choi, 201030 | AHA 2005 | + | CC-V | -- | Self-instruction kit (video, manikin)(22d) | + | -- | N/A | |||||||||
| De Vries, 201031 | ERC 2005 | + | CC | + | AED video-only(2.5) | AED video and practice on manikin(4.5) | AED video and practice on clinical scenario(9) | Instructor-led AED training(90) | -- | + | + | + | -- | N/A | N/A | N/A | 1:6 |
| Saraç, 201032 | ERC 2005 | + | CC-V | -- | Traditional instructor-led training, manikin(120) | Case-based instructor-led training, manikin(120) | Web-based self-instruction, practice on manikin(free accessd) | + | -- | 1:15 | 1:15 | N/A | |||||
| Mancini, 200933 | AHA 2005 | + | CC-V | + | Instructor-led training, booklet, video, manikin(22)c | Self-instruction kit (video, manikin with feedback)(45) | + | -- | + | 1:6 | N/A | ||||||
| Beckers, 200734 | ILCOR 2005 | -- | -- | + | Instructor, AED trainer(15) | -- | -- | Unknown | |||||||||
| De Vries, 200735 | ILCOR 2005 | + | CC-V | + | Self-instruction with web-based application(189) | -- | -- | N/A | |||||||||
| Jones, 200736 | ERC 2005 | + | CC-V | -- | Instructor-led training, manikin(30) | Self-instruction kit (video, manikin)(30) | + | -- | 1:6 | N/A | |||||||
AED, automated external defibrillator; AHA, American Heart Association; BLS, basic life support; CC, chest compressions; CC-V, chest compressions-ventilations; CPR, cardiopulmonary resuscitation; ERC, European Resuscitation Council; ILCOR, International Liaison Committee on Resuscitation; N/A, not applicable.
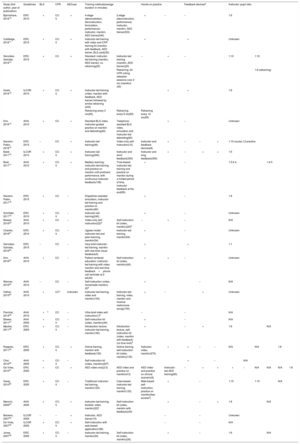
Table 3 summarizes the different timing, evaluation tools and variables used to assess the efficacy of the educational interventions. Almost half of the studies assessed correct performance of the BLS sequence (n=12). All studies teaching CPR evaluated performance (25/25) considering at least CC, while ventilation quality was only reported by 11 of the 15 studies that trained participants in both CC and ventilation CPR. A validated or self-made checklist completed by the evaluators while watching participants’ performance was the most common tool to assess approach to the victim (n=18). Skill-reporting manikins were mostly used (n=21) to appraise CPR quality, whereas AED trainers were used in one-third of studies evaluating defibrillation skills (n=9). Evaluation timing was highly variable: posttraining assessment–arbitrarily considered up to 2 weeks after training–was the most frequent (n=24), while practical skill retention–from 2 weeks in advance after initial training–was assessed by around 50% of the studies (n=14) at a mean period of 14 weeks. Only 4 studies evaluated participants’ skills at baseline, posttraining, and in the follow-up.
Evaluation Methodologies
| Study(first author, year of publication) | Evaluation tools | Evaluated variables | Evaluation moments | Evaluated attitudes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Survey | Checklist | QCPRManikin | AED trainer | BLS sequence | CPR | AEDuse | Baseline | Posttraining | Follow-up | Comfort with training | Willingness to share knowledge | Self-confidence | |
| Bjørnshave, 201810 | + | + | + | + | + | CC-V | + | -- | + | -- | -- | -- | + |
| Cartledge, 201811 | + | -- | + | -- | -- | CC | -- | -- | + | 4 wk | + | + | + |
| González-Salvado, 201812 | + | + | + | + | + | CC | + | + | + | 8 wk | -- | -- | + |
| Hsieh, 201813 | -- | + | + | + | + | CC-V | + | -- | -- | 48 wk | -- | -- | -- |
| Kim, 201814 | -- | -- | + | -- | -- | CC | -- | -- | + | 24 wk | -- | -- | -- |
| Navarro-Patón, 201815 | -- | + | + | + | -- | CC | + | + | + | -- | -- | -- | -- |
| Baldi, 201716 | -- | -- | + | -- | -- | CC | -- | -- | + | -- | -- | -- | -- |
| Boet, 201717 | + | + | + | -- | + | CC | -- | +a | + | 16 wk | -- | -- | -- |
| Navarro-Patón, 201718 | -- | + | + | -- | +b | CC | -- | +a | + | 16 wk | -- | -- | -- |
| Schröder, 201719 | + | + | + | -- | + | CC | -- | + | + | -- | -- | -- | -- |
| Blewer, 201620 | + | -- | + | -- | -- | CC | -- | -- | -- | 24 wk | -- | -- | -- |
| Charlier, 201621 | -- | -- | + | -- | -- | CC-V | -- | + | +c | -- | -- | -- | -- |
| González-Salvado, 201622 | -- | -- | + | -- | -- | CC | -- | -- | + | -- | -- | -- | -- |
| Kim, 201623 | + | + | +d | -- | +b | CC | -- | + | + | 4 wk | -- | -- | + |
| Wanner, 201624 | + | + | + | -- | -- | CC | -- | + | + | -- | -- | -- | + |
| Hafner, 201525 | + | -- | + | -- | -- | CC | -- | -- | + | 6 wk | -- | -- | + |
| Panchal, 201426 | -- | + | + | -- | +b | CC | -- | -- | + | -- | -- | -- | -- |
| Blewer, 201127 | + | -- | + | -- | +b | CC-V | -- | -- | + | 4 wk | + | + | -- |
| Mpotos, 201128 | -- | -- | + | -- | -- | CC-V | -- | -- | +e | 7 wk | -- | -- | -- |
| Roppolo, 201129 | -- | + | + | + | -- | CC-V | + | -- | + | -- | -- | -- | -- |
| Choi, 201030 | -- | + | +f | -- | -- | CC-V | -- | + | + | 8 wk | -- | -- | -- |
| De Vries, 201031 | -- | + | -- | + | -- | -- | + | -- | + | 8 wk | -- | -- | -- |
| Saraç, 201032 | -- | + | + | -- | + | CC-V | -- | + | + | 18 wk | -- | -- | -- |
| Mancini, 200933 | + | + | + | + | +b | CC-V | + | -- | + | -- | -- | + | + |
| Beckers, 200734 | -- | + | -- | + | -- | -- | + | + | +c | 24 wk | -- | -- | -- |
| De Vries, 200735 | -- | + | + | + | + | CC-V | + | -- | -- | 8 wk | -- | -- | -- |
| Jones, 200736 | -- | + | + | -- | +b | CC-V | -- | + | + | -- | -- | -- | -- |
AED, automated external defibrillator; BLS, basic life support; CC, chest compression; CC-V, compression-ventilation; CPR, cardiopulmonary resuscitation.
Only theoretical knowledge evaluation by means of a questionnaire was performed.
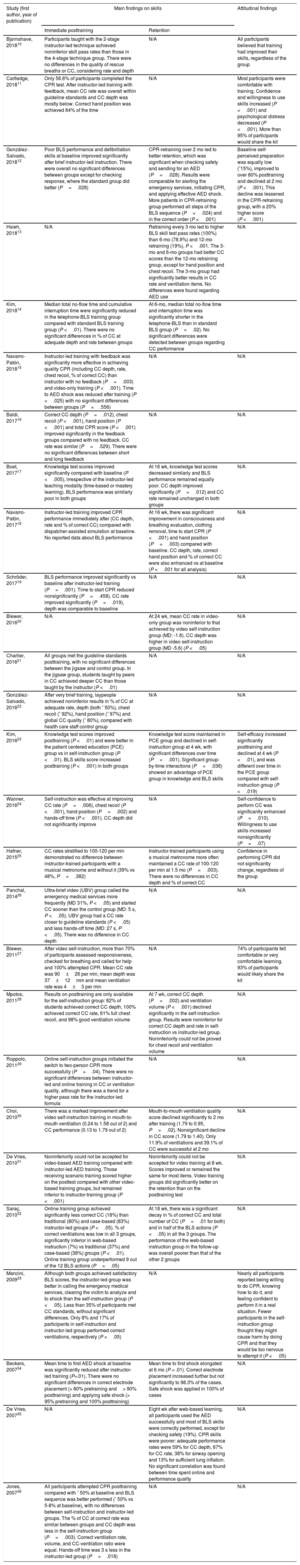
The main findings are detailed in Table 4. In addition, we addressed the effect of several strategic teaching factors on skill acquisition and/or retention:
Results
| Study (first author, year of publication) | Main findings on skills | Attitudinal findings | |
|---|---|---|---|
| Immediate posttraining | Retention | ||
| Bjørnshave, 201810 | Participants taught with the 2-stage instructor-led technique achieved noninferior skill pass rates than those in the 4-stage technique group. There were no differences in the quality of rescue breaths or CC, considering rate and depth | N/A | All participants believed that training had improved their skills, regardless of the group |
| Cartledge, 201811 | Only 56.6% of participants completed the CPR test. After instructor-led training with feedback, mean CC rate was overall within guideline standards and CC depth was mostly below. Correct hand position was achieved 84% of the time | N/A | Most participants were comfortable with training. Confidence and willingness to use skills increased (P <.001) and psychological distress decreased (P <.001). More than 95% of participants would share the kit |
| González-Salvado, 201812 | Poor BLS performance and defibrillation skills at baseline improved significantly after brief instructor-led instruction. There were overall no significant differences between groups except for checking response, where the standard group did better (P=.028) | CPR-retraining over 2 mo led to better retention, which was significant when checking safety and sending for an AED (P=.028). Results were comparable for alerting the emergency services, initiating CPR, and applying effective AED shock. More patients in CPR-retraining group performed all steps of the BLS sequence (P=.024) and in the correct order (P <.001) | Baseline self-perceived preparation was equally low (˜15%), improved to over 80% posttraining and declined at 2 mo (P <.001). This decline was lessened in the CPR-retraining group, with a 20% higher score (P <.001) |
| Hsieh, 201813 | N/A | Retraining every 3 mo led to higher BLS skill test pass rates (100%) than 6-mo (78.9%) and 12-mo retraining (19%), P <.001. The 3-mo and 6-mo groups had better CC scores than the 12-mo retraining group, except for hand position and chest recoil. The 3-mo group had significantly better results in CC rate and ventilation items. No differences were found regarding AED use | N/A |
| Kim, 201814 | Median total no-flow time and cumulative interruption time were significantly reduced in the telephone-BLS training group compared with standard BLS training group (P <.01). There were no significant differences in % of CC at adequate depth and rate between groups | At 6-mo, median total no-flow time and interruption time was significantly shorter in the telephone-BLS than in standard BLS group (P=.02). No significant differences were detected between groups regarding CC performance | |
| Navarro-Patón, 201815 | Instructor-led training with feedback was significantly more effective in achieving quality CPR (including CC depth, rate, chest recoil, % of correct CC) than instructor with no feedback (P=.003) and video-only training (P <.001). Time to AED shock was reduced after training (P <.025) with no significant differences between groups (P=.556) | N/A | N/A |
| Baldi, 201716 | Correct CC depth (P=.012), chest recoil (P <.001), hand position (P <.001) and total CPR score (P <.001) improved significantly in the feedback groups compared with no feedback. CC rate was similar (P=.529). There were no significant differences between short and long feedback | N/A | N/A |
| Boet, 201717 | Knowledge test scores improved significantly compared with baseline (P <.005), irrespective of the instructor-led teaching modality (time-based or mastery learning). BLS performance was similarly poor in both groups | At 16 wk, knowledge test scores decreased similarly and BLS performance remained equally poor. CC depth improved significantly (P=.012) and CC rate remained unchanged in both groups | N/A |
| Navarro-Patón, 201718 | Instructor-led training improved CPR performance immediately after (CC depth, rate and % of correct CC) compared with dispatcher-assisted simulation at baseline. No reported data about BLS performance | At 16 wk, there was significant improvement in consciousness and breathing evaluation, clothing removal, time to start CPR (P <.001) and hand position (P=.003) compared with baseline. CC depth, rate, correct hand position and % of correct CC were also enhanced vs at baseline (P <.001 for all analysis) | N/A |
| Schröder, 201719 | BLS performance improved significantly vs baseline after instructor-led training (P=.001). Time to start CPR reduced nonsignificantly (P=.458). CC rate improved significantly (P=.019), depth was comparable to baseline | N/A | N/A |
| Blewer, 201620 | N/A | At 24 wk, mean CC rate in video-only group was noninferior to that achieved by video self-instruction group (MD: -1.6). CC depth was higher in video self-instruction group (MD -5.6) (P <.05) | N/A |
| Charlier, 201621 | All groups met the guideline standards posttraining, with no significant differences between the jigsaw and control group. In the jigsaw group, students taught by peers in CC achieved deeper CC than those taught by the instructor (P <.01) | N/A | N/A |
| González-Salvado, 201622 | After very brief training, laypeople achieved noninferior results in % of CC at adequate rate, depth (both ˜ 50%), chest recoil (˜ 92%), hand position (˜ 97%) and global CC quality (˜ 80%), compared with health care staff control group | N/A | N/A |
| Kim, 201623 | Knowledge test scores improved posttraining (P <.01) and were better in the patient centered education (PCE) group vs in self-instruction group (P <.01). BLS skills score increased posttraining (P <.001) in both groups | Knowledge test score maintained in PCE group and declined in self-instruction group at 4 wk, with significant differences over time (P=.001). Significant group-by-time interactions (P=.036) showed an advantage of PCE group in knowledge and BLS skills | Self-efficacy increased significantly posttraining and declined at 4 wk (P <.01), and was different over time in the PCE group compared with self-instruction group (P <.019) |
| Wanner, 201624 | Self-instruction was effective at improving CC rate (P=.006), chest recoil (P <.001), hand position (P=.002) and hands-off time (P <.001). CC depth did not significantly improve | N/A | Self-confidence to perform CC was significantly enhanced (P=.010). Willingness to use skills increased nonsignificantly (P=.07) |
| Hafner, 201525 | CC rates stratified to 100-120 per min demonstrated no difference between instructor-trained participants with a musical metronome and without it (39% vs 48%, P=.382) | Instructor-trained participants using a musical metronome more often maintained a CC rate of 100-120 per min at 1.5 mo (P=.003). There were no differences in CC depth and % of correct CC | Confidence in performing CPR did not significantly change, regardless of the group |
| Panchal, 201426 | Ultra-brief video (UBV) group called the emergency medical services more frequently (MD 31%, P <.05) and started CC sooner than the control group (MD: 5 s, P <.05). UBV group had a CC rate closer to guideline standards (P <.05) and less hands-off time (MD: 27 s, P <.05). There was no difference in CC depth | N/A | N/A |
| Blewer, 201127 | After video self-instruction, more than 70% of participants assessed responsiveness, checked for breathing and called for help and 100% attempted CPR. Mean CC rate was 90±26 per min, mean depth was 37±12mm and mean ventilation rate was 4±3 per min | N/A | 74% of participants felt comfortable or very comfortable learning. 93% of participants would likely share the kit |
| Mpotos, 201128 | Results on posttraining are only available for the self-instruction group: 82% of students achieved correct CC depth, 100% achieved correct CC rate, 61% full chest recoil, and 98% good ventilation volume | At 7 wk, correct CC depth (P=.002) and ventilation volume (P <.001) declined significantly in the self-instruction group. Results were noninferior for correct CC depth and rate in self-instruction vs instructor-led group. Noninferiority could not be proved for chest recoil and ventilation volume | N/A |
| Roppolo, 201129 | Online self-instruction groups initiated the switch to two-person CPR more successfully (P=.04). There were no significant differences between instructor-led and online training in CC or ventilation quality, although there was a trend for a higher pass rate for the instructor-led formula | N/A | N/A |
| Choi, 201030 | There was a marked improvement after video self-instruction training in mouth-to-mouth ventilation (0.24 to 1.58 out of 2) and CC performance (0.13 to 1.79 out of 2) | Mouth-to-mouth ventilation quality score declined significantly to 2 mo after training (1.79 to 0.95, P=.02). Nonsignificant decline in CC score (1.79 to 1.40). Only 11.9% of ventilations and 39.1% of CC were successful at 2 mo | N/A |
| De Vries, 201031 | Noninferiority could not be accepted for video-based AED training compared with instructor-led AED training. Those receiving scenario training scored higher on the posttest compared with other video-based training groups, but remained inferior to instructor-training group (P <.001) | Noninferiority could not be accepted for video training at 8 wk. Scores improved or remained the same for most items. Video training groups did significantly better on the retention than on the posttraining test | N/A |
| Saraç, 201032 | Online training group achieved significantly less correct CC (18%) than traditional (80%) and case-based (83%) instructor-led groups (P <.05). % of correct ventilations was low in all 3 groups, significantly inferior in web-based instruction (7%) vs traditional (37%) and case-based (38%) groups (P <.01). Online training group underperformed 9 out of the 12 BLS actions (P=.05) | At 18 wk, there was a significant decay in % of correct CC and total number of CC (P=.01 for both) and in half of the BLS actions (P <.05) in all the 3 groups. The performance of the web-based instruction group in the follow-up was overall poorer than that of the other 2 groups | N/A |
| Mancini, 200933 | Although both groups achieved satisfactory BLS scores, the instructor-led group was better in calling the emergency medical services, clearing the victim to analyze and to shock than the self-instruction group (P <.05). Less than 35% of participants met CC standards, without significant differences. Only 8% and 17% of participants in self-instruction and instructor-led group performed correct ventilations, respectively (P <.05) | N/A | Nearly all participants reported being willing to do CPR, knowing how to do it, and feeling confident to perform it in a real situation. Fewer participants in the self-instruction group thought they might cause harm by doing CPR and that they would be too nervous to attempt it (P <.05) |
| Beckers, 200734 | Mean time to first AED shock at baseline was significantly reduced after instructor-led training (P=.01). There were no significant differences in correct electrode placement (> 80% pretraining and> 90% posttraining) and applying safe shock (> 95% pretraining and 100% posttraining) | Mean time to first shock elongated at 6 mo (P = .01). Correct electrode placement increased further but not significantly to 98.3% of the cases. Safe shock was applied in 100% of cases | N/A |
| De Vries, 200735 | N/A | Eight wk after web-based learning, all participants used the AED successfully and most of BLS skills were correctly performed, except for checking safety (19%). CPR skills were poorer: adequate performance rates were 59% for CC depth, 67% for CC rate, 38% for airway opening and 13% for sufficient lung inflation. No significant correlation was found between time spent online and performance quality | N/A |
| Jones, 200736 | All participants attempted CPR posttraining compared with ˜ 50% at baseline and BLS sequence was better performed (˜ 50% vs 5-8% at baseline), with no differences between self-instruction and instructor-led groups. The % of CC at correct rate was similar between groups and CC depth was less in the self-instruction group (P=.003). Correct ventilation rate, volume, and CC-ventilation ratio were equal. Hands-off time was 3 s less in the instructor-led group (P=.018) | N/A | N/A |
AED: automated external defibrillator; BLS, basic life support; CC, chest compression; CPR, cardiopulmonary resuscitation; MD, mean difference; N/A, not applicable.
Instructor-led vs self-instruction: self-instruction kits, video-only or web-based strategies were tested alone (n=3) or opposed to instructor-led formulas (n=10). Considering BLS sequence, 2 studies reported positive results of self-instruction on immediate skill acquisition26,27 and 1 study did so on retention at 8 weeks.35 When self-instruction was compared with instructor-led courses, immediate BLS skills improvement was found to be similar23,36 or slightly inferior32,33 in an equal number of studies, with 1 study reporting worse skill retention at 4 weeks.23 Regarding CPR quality, 12 studies assessed the effectiveness of self-training methods alone or compared with others. Even if CPR skills enhanced after self-instruction compared with no training, this improvement was generally insufficient to meet the recommended standards and tended to be inferior to instructor-led methods. Achieving adequate CC depth24,26–29,36 and ventilation quality27,28,30,32,33 remained especially difficult, particularly in the follow-up. Only 3 studies assessed self-instruction AED training methods: 2 yielded positive results15,35 and another reported inferior results compared with instructor-led learning.31
Hands-on practice and feedback devices: a wide majority of studies included hands-on practice; however, only 3 compared different strategies with and without it.22–24 Compared to video alone, self-instruction with video and practice on manikin was useful to enhance CC depth at 24 weeks20 and practice on a clinical scenario resulted in higher scores in AED use,31 respectively. Moreover, brief CPR hands-on practice over a 2-month period helped participants to remember the BLS sequence.12 Ten studies used feedback devices to guide CPR,11,13,15,16,22,23,25,28,29,33 but only 7 were not feedback-supported.15,16,23,25,28,29,33 Of these, feedback devices constituted the key distinct feature to the other strategy in 3 studies, which led to better CPR quality either posttraining15,16 or in the follow-up.25
Training duration and retraining: although long- or intermediate-duration methods were used in almost 75% of studies, there was an emerging presence of brief and very brief formulas (up to ˜ 20 minutes) (n=10). Most were self-instruction methods, with only 4 cases of instructor-led training,12,22,33,34 and were generally focused on a certain aspect of BLS training, with only 2 studies addressing all of them.12,15 Before-after or controlled studies assessing brief training formulas showed improvement in some BLS skills12,26 and CPR components such as hand position, hands-off time, CC rate, and chest recoil, while adequate CC depth was more difficult to achieve.22,24,26 Five studies reported enhanced defibrillation skills after brief training,12,15,31,33,34 which were maintained quite effectively in the follow-up.12,31,34 Retraining was only considered in 2 studies, either as frequent brief refreshers12 or as repeat course.22 Frequently retrained participants displayed better results in the follow-up,13 although the impact was less evident on defibrillation skills.
Attitudinal Aspects of TrainingAttitudes toward learning were addressed by a minority of studies (n=8). Comfort with training and decreased psychological distress were described in 1 instructor-led study.11 Two studies reported participants’ increased willingness to share knowledge with others after training.11,27 Finally, 7 studies addressed self-confidence or willingness to use skills, with overall positive results10–12,23,24,33 regardless of the method, and neutral effect was reported by another study.25
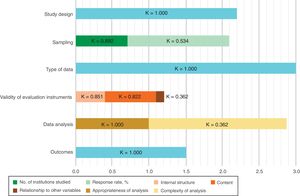
Quality of StudiesMERSQI scores of the included studies ranged from 11 to 15.5, with a mean score of 13 out of 18 and substantial agreement between reviewers (Cohen's kappa coefficient: 0.758) (Figure 2 and ). The main limitations were the lack of randomized controlled designs, single-center settings, the absence of reports of the validity of the evaluation instrument used, and skill measurement rather than behaviors or patient/health outcomes.
Study quality assessment and interrater reliability. MERSQI, Medical Education Research Study Quality Instrument. Horizontal bars represent the mean score achieved by the studies (n=27) for each MERSQI scale item, of a maximum score of 3 (18 in total). Cohen's kappa coefficient (K) to measure interrater reliability on each item is shown.
The markedly heterogeneous nature of the studies included in this systematic review hampered data pooling and the establishment of definitive recommendations on the optimal strategy to train adult laypeople in BLS. However, there was an apparent advantage of instructor-led methods, with hands-on practice, supported by real-time feedback. Retraining enhanced skill retention, especially if this was frequent and included hands-on practice, but was only reported in 2 studies.
Regarding study designs, it was striking that few were randomized controlled trials and, although many shared similar methods and instruments, multicenter collaboration was marginal. This may reveal the need to establish networks and joint efforts to design solid, sufficiently powered studies to test the effectiveness of training approaches in the long-term. However, guaranteeing the reproducibility of educational interventions might be challenging and the results might be biased by various factors involved in the learning process. In an effort to standardize BLS training, official courses were developed by various organizations committed to improving outcomes of out-of-hospital cardiac arrest, ie, the American Heart Association Heartsaver and the European Resuscitation Council BLS/AED provider course, frequently used as control methods in the reviewed studies. However, the need to make learning accessible to more citizens has led to new emergent formulas, including just-in-time or self-directed training, as an alternative to traditional courses.
Despite a rising number of BLS teaching initiatives, results are not always consistently reported. Although we considered only studies including practical skill evaluation to guarantee a minimum homogeneity and relevance of the results, several factors made it difficult to establish reliable comparisons among them. First, there was wide variability in contents, protocols, testing tools, variables, and assessment time. While some studies assessed the whole BLS sequence in detail,10,12,13,17,19,32,33,35 others assessed the programs less thoroughly or examined only certain steps.18,23,26,27,36 Likewise, most studies reporting CPR quality focused on CC, with only 40% assessing ventilations,10,13,21,27–33,36 but used different testing protocols and quality indicators. Second, there was a striking mismatch between imparted and evaluated contents. For instance, while correct performance of the BLS sequence was taught in> 90% of studies, less than half of these reported any results.3,10,12,13,17–19,23,26,27,32,35,36 Similarly, scarcely half the studies expressly taught AED use10,11,13–17,22,29,31,33–35 and only one-third reported results.10,12,13,15,29,31,33–35 Thirdly, data regarding the validity of the evaluation instruments were mostly lacking, resulting in lower MERSQI scores. Moreover, a certain degree of temporary offset of 2 to 3 years was detected in some studies that referred to previous guidelines rather than to those in use at the time of their publication.10,13,14,16,17,19 Consequently, there might be a need to pursue homogeneous updated quality standards and validated assessment instruments to ensure consistency,37 regardless of the training strategy applied.
Included participants were predominantly young female university students. This profile is, according to the literature, far from that of those most likely to witness out-of-hospital cardiac arrest, who are women but usually older, frequently spouses or other relatives of the victims.38 Focused training on high-risk groups has been acknowledged in both resuscitation2,3 and cardiology guidelines for the prevention of sudden cardiac death.39 In this review, positive results regarding skill acquisition and attitudes were reported by the 5 studies that analyzed training cardiac patients and/ or their relatives.11,12,20,23,27 This aligns with a previous review focused on this population,40 which nevertheless failed to prove effects on patient outcomes. Targeted training might be a sensible action complementary to others to enhance bystander resuscitation, but further research is needed.
Concerning the effectiveness of different methods, instructor-led training seemed to yield slightly better results than self-instruction, although with caveats. The wide spectrum of self-directed learning methodologies appraised made it difficult to draw definitive conclusions. Hsieh et al.8 already described this heterogeneity when they attempted to compare the effectiveness of BLS self-instruction to that of traditional instructor-led courses, failing to prove the superiority of one method over another. Although only methods including hands-on practice were included in their analysis, the high inconsistency among studies regarding participants, teaching and evaluation instruments or training duration was mentioned as a significant limitation. Self-instruction methods have been recommended as a possible alternative to traditional instruction and may have their role in reaching more citizens, increasing awareness, and being used as skill refreshers.2,3 Nevertheless, thorough design tailored to the needs of the target learners and hands-on practice might be crucial to enhance their effectiveness.
In this line, hands-on practice, especially if supported by feedback devices, was particularly important to improve CPR skills. “Simple” concepts such as correct hand position, hands-off time, and CC rate were quite well retained. Conversely, achieving correct depth was substantially more challenging. Likewise, ventilations were far from meeting quality standards. This agrees with current recommendations that support a simplified approach, promoting CC-only CPR training among laypeople without duty of care, especially in the case of time-limited or opportunistic training.2,3 Regarding defibrillation skills, several approaches resulted in enhanced performance that was quite well maintained in the follow-up. Again, hands-on practice, particularly if conducted on a simulated clinical scenario,31 led to better results. This finding, along with further evidence supporting the association between bystander defibrillation and improved clinical outcomes,41 may well encourage this training. However, it should be supported by a currently lacking common regulation on bystander AED use across European countries, in addition to other measures to overcome barriers to bystander defibrillation.42
Brief formulas were able to improve skills fairly well compared with longer methods, but the diversity of contents and tools used precluded drawing conclusions about training duration alone. Additionally, although exemplified in only 2 studies, the role of brief, frequent retraining was decisive to prevent BLS skill deterioration, as acknowledged in the current guidelines.2,3 Finally, only a minority of studies assessed attitudinal aspects of training with overall positive results, such as for self-confidence and willingness to use skills and to share knowledge. Watching these “invisible outcomes”43 might nevertheless be critical to build a favorable training environment and help overcome psychological barriers to bystander assistance.
Optimizing educational strategies and identifying why bystanders fail to respond are recognized major knowledge gaps that may affect public health.44 In addition to evaluating the effectiveness of different methodologies, it would be desirable to assess whether the efforts to train laypeople in BLS have any impact on clinical outcomes and study cost-effectiveness of interventions. There is recent evidence suggesting a positive association between an increased number of trained citizens and improved survival after out-of-hospital cardiac arrest.41,45 However, studies powered for these outcomes are difficult to undertake and their results might be confounded by several factors. A good example is the national campaign launched in Denmark in 2005, comprising obligatory BLS training at elementary schools and to get a driving license, distributing training kits, implementing a dispatcher-assisted program to guide bystanders, and enhancing public access defibrillation. This resulted in 2-fold increase in bystander-assisted cardiac arrests, doubled the percentage of victims arriving alive at the hospital and tripled 30-day and 1-year survival, all in less than 10 years.45 However, such interventions are usually part of a set of measures targeting the same goal, which makes it difficult to ascertain a causal relationship between training and clinical outcomes.
LimitationsThis review has several limitations. First, a single database (MEDLINE) was searched. However, the list of references of all included articles was manually assessed to detect potentially includible studies. Also, we did not include in this review conference abstracts, letters to editors, opinion papers or information in the gray literature; consequently, additional information might be available but was not reported. As previously mentioned, the wide heterogeneity of studies was an important obstacle to pooling data and obtaining more reliable conclusions. Additionally, methods were reported with very different levels of detail across studies. This left some quality assessment to subjective interpretation, carrying a nonnegligible risk of bias. However, there was substantial agreement between reviewers when appraising quality. Developing a scale specifically designed to evaluate this type of studies could be a further step to help to standardize quality assessment.
CONCLUSIONSA systematic review of strategies to train laypeople in BLS was not able to define the gold standard method, given the wide heterogeneity of contents, methods, assessment tools, and variables that precluded the establishment of definitive conclusions. The simplicity of BLS protocols, intended to reach the entire population, allowed a wide diversity of training approaches to obtain positive results to some extent in the short-term. However, instructor-led methods with hands-on feedback-supported practice seemed to be superior to alternative strategies. To enhance skill retention, brief frequent refreshers showed an advantage over other options. Further studies on the subject are needed to recommend standardized quality training criteria and validated evalution instruments at an international level, assessing effectiveness both in the short- and long-term.
- –
Bystander assistance is crucial to enhance outcomes of out-of-hospital cardiac arrest.
- –
International recommendations call for generalizing BLS training to the entire population.
- –
Despite a large number of educational initiatives, there is no definitive evidence on the most effective method.
- –
The scientific literature on adult BLS training shows wide heterogeneity.
- –
Different strategies were able to improve results in the short-term, but there were fewer data concerning retention.
- –
Instructor-led training and feedback-supported hands-on practice seemed to have an advantage over other methods.
- –
There were scarce data about the effects of frequent training sustained over time in favor of one-time initiatives.
None declared.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2018.11.013