Acute myocardial infarction (AMI) is a major cause of death and disability worldwide.1–3 The risk of death and the benefit from early revascularization are highest within the first hours, and therefore early diagnosis is critical. Biomarkers play a critical role in the early diagnosis of AMI. In fact, an elevation in cardiac troponin (cTn) of at least one measurement above the 99th percentile of a healthy reference population has become a condition sine qua non for the diagnosis of AMI.1–3
WHAT IS THE UNMET CLINICAL NEED?Biomarkers, to be more precise cTn, complement clinical assessment and the 12-lead electrocardiogram in the diagnosis and management of patients with suspected AMI. In AMI, cTnI and cTnT are released from necrotic myocardium. A major limitation of conventional cTn assays is their low sensitivity at the time of patient arrival to the emergency department (ED), owing to a delayed increase of circulating levels in peripheral blood that requires serial sampling and prolonged monitoring for 6 to 12h in a significant number of patients.1–3 This sensitivity deficit contributes substantially to diagnostic uncertainty, delays in the initiation of the appropriate therapy, and increases in resource use and treatment costs.1–3
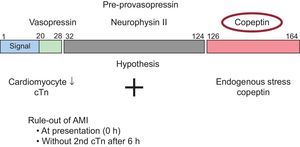
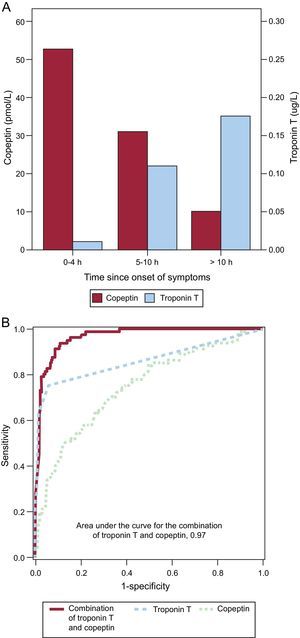
WHAT IS COPEPTIN?Copeptin is a novel blood biomarker that has entered the clinical arena thanks to the development of an analytically sound method to measure a signal that is released stoichiometrically with biologically active vasopressin. Although our insights into the exact pathophysiology of vasopressin and copeptin are still incomplete, currently available data can best be summarized as suggesting that copeptin levels reflect and quantify endogenous stress. As a signal, copeptin is therefore distinct from B-type natriuretic peptides, which reflect hemodynamic cardiac stress (end-diastolic wall stress). Copeptin, the c-terminal part of the vasopressin prohormone, is secreted stochiometrically with arginin-vasopressin from the neurohypophysis. Copeptin levels seem to closely reflect the individual endogenous stress level as well as the risk of death in multiple medical conditions, including AMI4–14 (Figure 1). As endogenous stress is present already at the onset of AMI, copeptin appears to be able to identify AMI very early after symptom onset, even when cTn is still negative (Figure 2A).4–15 As endogenous stress is a very unspecific signal, it can only be used in this indication in combination with cTn. When used in conjunction with conventional 4th generation cTnT (a well characterized conventional cTn assay), the added value of copeptin regarding diagnostic accuracy upon ED arrival was substantial.4–6 As the time course of endogenous stress and detectable cardiomyocyte damage is reciprocal, copeptin seems to be the ideal marker to compensate for the sensitivity deficit of conventional cTn assays in early presenters.
A: Copeptin and troponin T levels on arrival at emergency department in relation to time since onset of symptoms. Levels of copeptin and cardiac troponin T according to the time since the onset of acute chest pain in patients with acute myocardial infarction. As the time course of endogenous stress and detectable cardiomyocyte damage seems to be reciprocal, copeptin seems to be the ideal marker to compensate for the sensitivity deficit of conventional cardiac troponin T assays in early presenters. B: receiver operating characteristic curves at presentation for the diagnosis of acute myocardial infarction. When used in conjunction with conventional fourth generation cardiac troponin T, the added value of copeptin regarding diagnostic accuracy at presentation is substantial. Adapted from Reichlin et al.,4 with permission.
Initial pilot studies investigating the combination of copeptin with high-sensitivity cTnT (hs-cTnT) suggested that copeptin may still provide some incremental value regarding diagnostic accuracy upon ED arrival (Figure 2B), but of much smaller magnitude than that observed with the conventional 4th generation cTnT.4–14 Copeptin also provides substantial added prognostic information regarding the risk of short-term and long-term mortality in addition to either cTn or hs-cTn. The concept in which copeptin seems to have the greatest appeal to clinicians is its use within a dual-marker strategy for very early rule-out of AMI: patients with acute chest pain presenting to the ED with initial negative values (< 99th percentile) of hs-cTn and also low levels of copeptin (e.g. < 10pmol/L) do have a very high negative predictive value (around 99%) for AMI and seem to be ideal candidates for very early rule-out of AMI and rapid discharge from the ED without the need for serial cTn testing. Obviously, the potential for economic savings with this approach is enormous. In fact, data from a large, multicenter, randomized, controlled study evaluating the safety and efficacy of this approach as compared to standard of care (2nd cTn measurement after 3-6h) have confirmed the safety and efficacy of this strategy.11
Currently there is no consensus among experts whether the incremental value provided by copeptin is sufficient to merit its introduction into routine clinical care of patients with acute chest pain in the ED. In institutions currently using conventional cTn assays such as the fourth generation cTnT or all currently available point-of-care cTn assays (which achieve sensitivities similar to the 4th generation cTnT), the incremental value is very large and in our opinion strongly argues in favor of routine addition of copeptin testing at the first blood draw. In institutions using hs-cTn assays and the 99th percentile as the decision point for AMI as recommended in the universal definition of AMI,1–3 future studies as well as clinical acceptance issues will define whether the additional use of copeptin will become a clinically accepted early rule-out strategy.
APPLICATION OF COPEPTIN BEYOND ITS USE FOR RAPID RULE-OUT OF ACUTE MYOCARDIAL INFARCTIONCopeptin may provide substantial additive information also in patients with mild hs-cTn elevation. As mild elevations in hs-cTn may also be caused by multiple chronic conditions, including heart failure, hypertensive heart disease, or valvular heart disease, copeptin may help to separate these stable chronic conditions, which are expected to be associated with rather low copeptin levels, from patients with AMI or myocarditis, both of which associated with very high copeptin levels.
CONCLUSIONIn conclusion, the dual-marker strategy combining the quantitative signals of cardiomyocyte damage (cTn) and endogenous stress (copeptin) provides high accuracy for the early diagnosis of AMI and may well become one of the preferred clinical strategies in the near future.
CONFLICTS OF INTERESTDr. Mueller has received research support from the European Union, the Swiss National Science Foundation, the Swiss Heart Foundation, Basel University, the University Hospital Basel, the Cardiovascular Research Foundation Basel, Abbott, Brahms, Roche, Siemens, and 8sense, as well as speaker or consulting honoraria from Abbott, BG Medicine, bioMérieux, Brahms, Massachusetts General Hospital, Novartis, Roche, and Siemens.