Over 100 years ago, animal studies and observations in isolated patients indicated that therapeutic hypothermia could be useful after a cardiac arrest. However, its use has only been recommended in cardiopulmonary resuscitation guidelines since 2003,1 specifically in patients with a shockable rhythm who fail to regain consciousness after the return of spontaneous circulation, based on 2 small randomized studies published in 2002.2,3 Subsequently, this treatment has slowly been adopted by critical care units. Its clinical usefulness seemed unmistakable, and multiple Spanish and international series have reported prognostic improvements in their centers since the incorporation of hypothermia into their standards of care.4,5 The questions that subsequently arose focused on the method, the timing of initiation, the target temperature, and its duration. One year ago, all knowledge gleaned from the previous century was shaken by the publication of the 2 largest randomized studies of patients resuscitated from out-of-hospital cardiac arrest (OHCA).6,7 These studies failed to show a benefit of hypothermia. Both publications have considerably impacted patient management. The Global Emergency Medicine Journal Club8 analyzed 18 blogs and 7 podcasts, despite their lack of scientific validity. In an online poll, more than 65% of participants responded that, in view of the results of these 2 studies, the standard of care for OHCA in their centers had changed to a target of 36°C or should be set at this threshold to avoid hyperthermia, instead of inducing hypothermia. Nevertheless, several months after learning of these results, most respondents acknowledged that this change remained to be applied.
Apart from hypothermia, no approach has shown a benefit in randomized clinical trials of comatose patients resuscitated from OHCA. Thus, physicians attending these patients must wonder what approach they should now take in daily clinical practice. Although patient prognosis has clearly improved and these results have coincided with the introduction of therapeutic hypothermia, this upswing could be because a change in attitude toward these patients has improved their care, with staff now believing that patient prognosis can be improved if they are treated according to an established standard of care. Until more information becomes available, the daily clinical management of these patients could be guided by consideration of the available evidence.
STUDIES IN EXPERIMENTAL ANIMALSThe common characteristics of the animal studies are that all of them used samples with arrests of controlled durations and, additionally, most used cardiopulmonary bypass to ensure subsequent circulation, guaranteeing homogeneous reperfusion in all animals. Such homogeneity is difficult to achieve in human studies. Using small samples in controlled conditions, most of the animal studies have shown significant differences in favor of functional and anatomical improvements in experimental animals treated at between 32°C and 34°C.9 There is even a dose-dependent effect of temperature on brain damage—the lower the temperature reached, the lesser the resulting damage.10 However, below 32°C, there can be increased arrhythmic complications and coagulopathy.
In contrast to the studies performed in humans, many aspects related to hypothermia in the animal studies could largely explain the differences found vs human studies. In animal studies, hypothermia was induced soon after restoration of circulation. The greater the delay in the instauration of hypothermia, the smaller the benefit.11 There might be differences in the hemodynamic stability obtained by cardiopulmonary bypass and that of patients with spontaneous circulation treated with hypothermia. Additionally, human studies included much more heterogeneous samples, greatly impacting the calculation of the sample size needed to show an effect. An illustration is provided by reperfusion in the setting of acute myocardial infarction. In the animal models, the efficacy of hypothermia was evident in small samples, but several thousand patients were required to show its efficacy in humans, due to the inclusion of heterogeneous patient samples. In contrast, in samples of homogeneous patients, such as those with recent-onset ST-segment elevation only, the efficacy of reperfusion could be demonstrated with just 250 patients.12
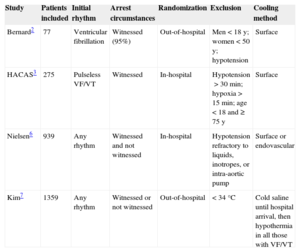
STUDIES IN HUMANSBasically, only 4 studies have randomized comatose patients to hypothermia or normothermia after a return of spontaneous circulation. Two of these2,3 showed a beneficial effect of hypothermia, whereas the 2 more recent studies6,7 failed to find a benefit. The main differences among the 4 studies are shown in the Table. The distinction between explanatory and pragmatic clinical trials is not dichotomous, because both are part of a continuum, and their differentiation is rarely easy, because most trials have both explanatory and pragmatic aspects. Those trials that failed to obtain good results with hypothermia6,7 had a fundamentally pragmatic design, that is, they were performed in real-world circumstances. Pragmatic clinical trials evaluate the effects of interventions just as they would be performed in standard practice, have fewer barriers to the inclusion of patients who might benefit from a treatment, obtain much more generalizable results, and aid decision-making by considering the different ways interventions are implemented in the real world. Pragmatic studies serve to determine the effectiveness of treatments in general practice, but they generally need large sample sizes to obtain usable and reliable evidence, due to the inclusion of heterogeneous groups. The inclusion of a greater number of confounders, such as comorbidities or different management approaches, makes it much more difficult to detect significant differences between groups (β error), even if these factors are adequately considered in the statistical analysis. In contrast, the designs of the clinical trials that obtained favorable results were closer to those of an explanatory clinical trial2,3 and to those of animal studies: these trials included only shockable rhythms and witnessed arrests and used the same cooling method in all patients. Explanatory trials are performed in more controlled settings and generally aim to acquire knowledge on the effects of specific interventions in a disease, to select groups with similar application conditions, and to allow evaluation of the effect of a specific technique. Unfortunately, their generalizability is limited, but they have the advantage of requiring smaller samples, being cheaper, and testing the effectiveness of the concepts.
Characteristics of Studies Analyzing the Effect of Therapeutic Hypothermia in Coma Patients Resuscitated from Out-of-hospital Cardiac Arrest
| Study | Patients included | Initial rhythm | Arrest circumstances | Randomization | Exclusion | Cooling method |
|---|---|---|---|---|---|---|
| Bernard2 | 77 | Ventricular fibrillation | Witnessed (95%) | Out-of-hospital | Men<18 y; women<50 y; hypotension | Surface |
| HACAS3 | 275 | Pulseless VF/VT | Witnessed | In-hospital | Hypotension>30 min; hypoxia>15 min; age<18 and ≥ 75 y | Surface |
| Nielsen6 | 939 | Any rhythm | Witnessed and not witnessed | In-hospital | Hypotension refractory to liquids, inotropes, or intra-aortic pump | Surface or endovascular |
| Kim7 | 1359 | Any rhythm | Witnessed or not witnessed | Out-of-hospital | <34°C | Cold saline until hospital arrival, then hypothermia in all those with VF/VT |
VF/VT, ventricular fibrillation/ventricular tachycardia.
Undoubtedly, the most controversial study is the TTM study.6 This study was an international, multicenter, randomized trial that randomized patients to 33°C or 36°C. Survival at the end of the trial was 50% in the 33°C group and 48% in the 36°C group. There were no differences between different subgroups of age, sex, resuscitation time, initial rhythm, state of shock on admission, and size of the participating center. One of the main sources of controversy, praised by some and criticized by others, was the protocolized restriction of the therapeutic intervention to a similar duration in both groups. Importantly, because the 33°C group spent significantly more days on mechanical ventilation, these patients were less likely than the 36°C group to have awakened before the predetermined evaluation of prognosis (44% vs 52%; P=.03). Additionally, the lower the temperature reached by patients, the more delayed their awakening,13 chiefly because of a slower metabolism due to the sedative medication. There may be other possible explanations for the differences between the TTM study and other studies. In the TTM study, hyperthermia was not permitted and the temperature was controlled in both treatment arms, which is why the authors concluded that this was the beneficial mechanism. However, the difference between arms could have been narrowed by the improved care in both groups, due to the active treatment in both arms. In the TTM study, the mean time until the return of spontaneous circulation of 25minutes showed a wide interquartile range that may have caused imbalances not taken into account in the analysis. Moreover, the patients assigned to the 33°C group generally showed a worse risk profile than those assigned to the 36°C group. Another striking aspect was the high percentage of patients with pupillary and corneal reflexes on hospital arrival (77% and 65%, respectively), much higher than in other studies, possibly indicating a high percentage of patients with good prognosis. The presence of a pupillary response is one of the strongest predictors of a good neurological outcome. The high percentage of patients with a good pupillary and corneal reflexes could be because basic cardiopulmonary resuscitation was initiated a median of 1minute after cardiac arrest. At the other end of the scale, a considerable number of patients arrived with temperatures<33°C, possibly indicating a subgroup of patients with considerable neurological damage. Patients with extensive damage clearly died independently of the treatment, and the hypothermia possibly had no effect in patients with minimal neurological damage. This leaves open the possibility of a positive effect of hypothermia in patients with moderate damage who could be underrepresented in the TTM study.
Importantly, the TTM study was designed as a study of the superiority of 33°C vs 36°C. It was not designed to show the non-inferiority of 36°C vs 33°C. Therefore, the only possible conclusion is that the TTM study failed to show the superiority of 33°C vs 36°C as a target temperature; it was also unable to show that 36°C is not inferior to 33°C.
Perhaps the most relevant aspect of the study by Kim et al,7 in addition to its pragmatic design, is that it only compared the effect of hypothermia from the return of spontaneous circulation until hospital arrival. Most patients in the 2 treatment arms were treated with hypothermia once they arrived at the hospital, with a mean delay of 50minutes. The only possible conclusion is that cooling with cold saline delayed less than 1 hour has no therapeutic benefit in this setting.
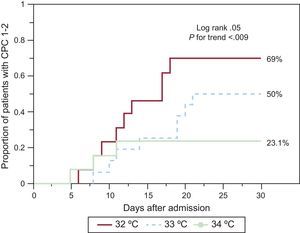
FUTUREGiven the current controversy, new trials with explanatory designs may have to be considered to more accurately define the issues that have arisen, before outlining a new study with the most pragmatic design possible. Thus, we designed a pilot explanatory study to evaluate the value of exploring different target temperatures.14 This pilot study aimed to reproduce the most controlled conditions possible in 36 patients resuscitated from OHCA. An attempt was made to minimize the variability in the existing prognosis in these patients. Randomization to the 2 temperatures was stratified according to the initial rhythm, only witnessed arrests were selected, and the same method of endovascular cooling and the same protocol were used in all patients. In this study, in patients whose initial rhythm was asystole, the degree of hypothermia had no relation to prognosis, whereas patients with an initial shockable rhythm assigned to 32°C had better results than those assigned to 34°C. A pilot study does not aim to modify the treatment guidelines, but to merely act as a source of information for future research. Because the differences in the results between the 2 temperatures could also be due to chance or distinct risk profiles, further analyses were considered. Contemporaneously with this pilot study, our center recorded all patients treated with hypothermia during the inclusion period. For nonrandomized patients treated with hypothermia, a target temperature of 33°C was selected, which was standard practice in the center. The remainder of the protocol was similar to that of the randomized patients regarding cooling and management. To improve understanding in a setting with such high morbidity and mortality, the ethics committee of the center allowed anonymous analysis of the results of patients with a shockable rhythm who were not randomized, despite meeting the inclusion criteria and none of the exclusion criteria. Typically, these patients were not randomized because there was no legal representative available during the inclusion window to provide give consent for participation. However, in 3 patients, the representatives objected to the treatment randomization and preferred the intermediate value of 33°C. To determine the results of the pilot study, neurological outcome was assessed at discharge and at 6 months’ follow-up by physicians blinded to the temperature assignment. Given that 1 patient who had neurologically recovered died without undergoing a blinded evaluation, an additional analysis was performed of the time until first detection of neurological recovery, as determined by the physician attending the patient and grades 1 or 2 of the Cerebral Performance Category (CPC) scale. The results of this analysis are shown in the Figure. Obviously, these results are purely informative, but they indicate a possible dose-dependent effect of the target temperature. This observation is the basis of a new ongoing explanatory study, the multicenter international FROST-I (Finding the Optimal Cooling tempeRature After Out-of-HoSpiTal Cardiac Arrest; NCT02035839) trial, with a predominantly Spanish participation, which is attempting to obtain more information by randomizing patients with a shockable rhythm to a target temperature of 32°C, 33°C, or 34°C. There may be results in the first half of 2016, which would allow determination of whether it is reasonable to perform a pragmatic study in this area.
Kaplan-Meier estimation of the time until the detection of a Cerebral Performance Category (CPC) grade 1 or 2 in survivors of out-of-hospital cardiac arrest at 30 days according to target temperature in the study of López-de-Sá et al14 and a simultaneous registry.
Based on the available data, a decision must be taken on how to treat these patients in daily practice. Pending a formal consensus on the optimal target temperature for these patients, the International Liaison Committee on Resuscitation (ILCOR) recommends that hypothermia be induced to 32°C - 34°C in patients resuscitated from OHCA with shockable rhythm, although a target temperature of 32 - 36°C may now be accepted.15
CONFLICTS OF INTERESTThe author has received research grants, consultancy fees, and lecture honoraria from ZOLL Circulation Inc.