To the Editor,
Rheumatoid arthritis (RA) is an inflammatory immune system disorder that is associated with a higher level of morbidity and mortality than found in the general population, mainly because of cardiovascular disease. In Switzerland, mortality due to RA increased by >50% and, in England, it was 1.5–1.6 times higher, principally due to myocardial infarction but also to valvular dysfunction.1,2 We report the case of a patient with RA who was admitted for acute aortic syndrome (i.e. an aortic intramural hematoma developing into a dissection). A literature search carried out using PubMed and the keywords “rheumatoid arthritis” AND “aortic dissection” revealed no evidence of an association between the two, which we believe is a possibility.
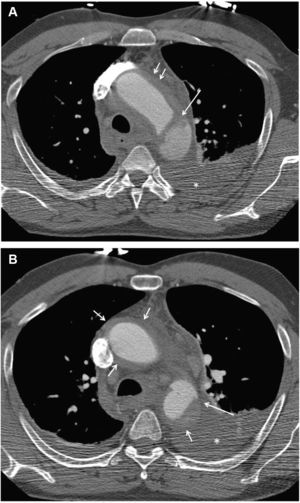
The patient was a 47-year-old man who smoked 70 cigarettes/day and had high blood pressure of recent onset, which was being treated with enalapril. He had been diagnosed with RA 7 years earlier and was currently receiving methotrexate, leflunomide, indometacin, folic acid, and deflazacort. He presented with severe retrosternal pain that radiated to the neck and back and which was associated with autonomic symptoms. On admission, his blood pressure was 110/60mmHg and his heart rate was 80 beats/min. A hemogram and biochemical study gave normal results: the erythrocyte sedimentation rate was 79mm/h. Thoracic multidetector computed tomography CT (Figure 1) showed an aortic hematoma associated with a Stanford type-B dissection (i.e. distal to the left subclavian artery). The patient was admitted to intensive care unit where his blood pressure was maintained at <120/80mmHg. The chest pain disappeared and subsequent examinations revealed partial resolution of the aortic hematoma. An aortic endoprosthesis was used to stabilize the patient's condition.
Figure 1. Thoracic multidetector computed tomography. A: aortic intramural hematoma (short arrows) associated with dissection (long arrow); hemothorax (asterisk). B: (lower level than A) hematoma in the wall of the ascending and descending aorta (short arrows) associated with dissection (long arrow); hemothorax (asterisk).
The association between RA and loss of elasticity in the aorta is principally due to inflammatory changes and structural alterations, such as smooth muscle hypertrophy and changes in the extracellular matrix characterized by an increase in collagen and a reduction in elastin, all of which predispose to increased rigidity of the arterial wall. Moreover, smooth muscle cells can produce bioapatite (they express osteoblastic markers under inflammatory conditions) which causes calcification of the aortic tunica media. Perivascular inflammation and cellular infiltration around the vasa vasorum have been observed to result in ischemia.3 It is widely recognized that aortic intramural hematoma is caused by rupture and bleeding from the vasa vasorum. We believe that these mechanisms (principally ischemic phenomena in the vasa vasorum themselves) may have triggered the condition in our patient. Moreover, in RA, a type of peripheral neuropathy caused by necrotizing vasculitis of the vasa vasorum has been reported.4
Hollan et al.5 studied changes in the aortic wall (i.e. inflammatory changes) in specimens obtained following coronary artery revascularization surgery, and compared findings in patients with and without RA. They excluded patients with infiltration close to the intima, which can occur in normal individuals, and focused on observations in the tunica media and tunica adventitia. They concluded that the observed changes were greater in patients with RA and that they could represent an inflammatory state that promotes the development of arteriosclerosis and the formation of aneurysms by decreasing the resistance of the arterial wall.
Although initially the vasculitis was attributed to occlusive vascular disease associated with giant cell arteritis (which corresponds to the current understanding of RA, principally with regard to the coronary arteries), it was subsequently clear that inflammatory changes in the aorta associated with high blood pressure can also lead to the formation of an aneurysm and dissection.6,7
Corresponding author:. hunter1@ono.com