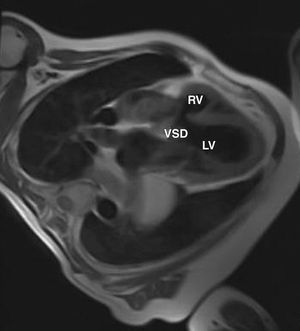
We report the case of a 56-year-old asymptomatic man with a pulmonary grade III/VI holosystolic murmur. No electrocardiographic changes were observed. On echocardiography, the left ventricle was normal with normal systolic function, and the right ventricle (RV) was hypertrophic with a midventricular gradient (maximum, 56; mean, 33 mm Hg) and a perimembranous ventricular septal defect (VSD). On magnetic resonance imaging, the RV was seen to be divided into 2 chambers (pRV: proximal chamber, dRV: distal chamber) separated by a muscle band (Figure 1) and the VSD (Figure 2). A hemodynamic study showed an intraventricular (not transvalvular) gradient of 50 mm Hg and a VSD with a pulmonary-to-systemic flow ratio of 1.4. Since the patient was asymptomatic and the obstruction was not severe, the initial decision was to clinically follow-up the patient.
Figure 1. Double-chambered right ventricle. dRV indicates distal chamber; pRV, proximal chamber; LV, left ventricle.
Figure 2. Double-chambered right ventricle. VSD indicates ventricular septal defect; RV, right ventricle; LV, left ventricle.
This is an interesting case because these patients usually present with symptoms in infancy or adolescence secondary to right ventricular failure due to the gradient between the 2 RV chambers or associated lesions (ventricular septal defect or subaortic stenosis). The mid-ventricular obstruction often progresses and results severe between the third and fifth decade of life. Survival without surgery is unusual after the age of 50. Surgical repair is recommended in the presence of symptoms or, in asymptomatic patients, when there is a significant gradient between the proximal and distal RV chambers (>40 mm Hg). Long-term follow up of patients who have undergone surgical repair demonstrates in nearly all cases that the obstruction does not recur.