Keywords
INTRODUCTION
The management of patients with non-ST-segment elevation acute coronary syndrome (NSTEACS) has been a permanent issue of debate in recent years.1-3 One of the problems most frequently posed is the question of the usefulness of an invasive strategy (IS).1-8
The results of the last three large studies demonstrate the benefit of this strategy.6-8 Consequently, recent guidelines recommend routine invasive management of the patient with high-risk NSTEACS (electrocardiographic changes or rise of myocardial injury markers).9,10 However there is little information with regard to the applicability and clinical impact of these recommendations in the real world.
The aim of the present work is to analyze the prognostic impact involved in the use of an IS in the management of patients with NSTEACS with high-risk characteristics admitted to our center over a 1-year period.
PATIENTS AND METHODS
Study Group
We reviewed all the patients consecutively evaluated in our chest pain unit between October 1, 2001 and September 30, 2003, with high clinical suspicion of NSTEACS when assessed by the duty cardiologist. Following the protocol previously described,11 serial troponin I studies were carried out (immunometric method, DPC, Los Angeles, California, USA) as well as an electrocardiogram (ECG). With the aim of only analyzing those cases where current recommendations suggest a prognostic benefit upon being treated with an IS,9,10 the study group included 504 patients with typical chest pain who fulfilled some of the following criteria: a) electrocardiographic evidence of ischemia: ST segment depression (>1 mm at 80 ms after the J-point) or T-wave inversion (>1 mm), and b) evidence of myocardial injury (troponin I 1 ng/mL in some of the serial measurements). Basal characteristics are shown in Table 1.
In all cases, treatment was begun with low molecular weight heparin, acetylsalicylic acid, nitrates and beta-blockers (except for strict contraindications for any of these drugs) in the emergency area. Glycoprotein IIb/IIIa inhibitors were only administered to patients undergoing percutaneous revascularization based on the decision of the catheterization specialist and treatment begun in the hemodynamic laboratory. The use of intracoronary stents was general throughout the study period. When stents were implanted, a loading dose of 300 mg clopidrogrel was administered, and combined antiplatelet aggregation drugs were maintained (100 mg acetylsalicylic acid and 75 mg clopidrogrel) for 1 month.
Conservative and Invasive Management Groups
Between October 1, 2001 and September 30, 2002, a conservative strategy (CS) was followed so that if the patient remained stable during admission an exercise stress test was carried out prior to discharge. Depending on the decision of the clinical cardiologist, the patient was discharged (when more than 85% of the expected maximum frequency was achieved and the result was negative) or cardiac catheterization was done (if the result of the exercise stress test was positive or the patient had shown clinical instability during admission: a new episode of chest pain of coronary origin, signs of heart failure, electric or hemodynamic instability). The cohort of 272 patients included in this period (intention to treat conservatively) formed the CS group.
From 1st October 2002, and in line with current guidelines,9,10 the team of clinicians and catheterization specialists in our unit implemented a routine invasive management strategy for patients with high-risk NSTEACS (changes in ECG and elevated troponin I). Cardiac catheterization and revascularization was recommended if it was anatomically possible prior to discharge. In no case was invasive management "demanded" by the protocol and the clinical cardiologist always had the final decision on whether to carry out cardiac catheterization or not in a given patient. Between October 1, 2002 and September 30, 2003, 232 patients were included (intention to treat invasively) in the IS group. The baseline characteristics of the IS and CS groups are presented in Table 1.
Surgery was recommended for all the patients included in the present study who had undergone catheterization, in case of left main coronary artery disease or multivessel disease with severely depressed systolic function. Angioplasty was done in the case of one-vessel or multivessel disease amenable to percutaneous treatment providing systolic function was not severely depressed.
Events and Follow-up
The aim of the study was to analyze the differences between the cohorts of patients managed with either intention to treat conservatively or invasively regarding: a) major events: cardiac death or infarction. Reinfarction was defined in line with current recommendations on the basis of the existence of elevated troponin I, with typical chest pain or conclusive electrocardiographic changes.12 In the patients treated with revascularization, necrosis markers were determined during the first 12 h post-revascularization. In addition, patients in whom troponin I (MB fraction of creatine kinase if troponin I was already high) increased by more than twice its normal upper limit (in the case of angioplasty) or more than 3 times (in the case of surgery) were considered to have had an infarction; b) minor events: readmission for acute coronary syndrome or need for revascularization after discharge; and c) any event: major or minor event. A 12-week follow-up was done in all cases via outpatient services, case-history review, and telephone interviews. In the case of a combined event it was considered that the event had taken place when any of these had occurred.
Statistical Analysis
The quantitative variables are expressed as mean±standard deviation and were compared through unpaired Student t test. The qualitative variables are expressed as percentages and were compared through the Chi-squared test.
The relationship between the treatment strategy used (intention to treat conservatively period vs intention to treat invasively period) and the appearance or otherwise of major events (cardiac death or infarction), minor events (readmission or post-discharge revascularization) and any event (major or minor) in the univariate studies was carried out via Kaplan-Meier survival curve analysis (log-rank test).
Finally, we analyzed the prognostic role--regarding the appearance of major events, minor events, and any event--of the type of strategy used (intention to treat conservatively period vs intention to treat invasively period) adjusted for the following variables: age, sex, smoking habit, arterial hypertension, background of hypercholesterolemia, diabetes mellitus, background of ischemic heart disease, background of infarction, background of angioplasty, background of heart surgery, kidney failure (creatinine 1.5 mg/L), signs of heart failure, depressed ST segment, T-wave inversion, and high troponin I level. The multivariate studies were conducted via Cox regression, including the treatment period (IS vs CS) and all the cited variables. Hazard ratio (HR) and confidence intervals (95% CI) were calculated. P<.05 was considered significant in all cases. The SPSS 9.0 statistical package was used (Chicago, Illinois) for statistical analysis.
RESULTS
The baseline clinical characteristics of the entire study group, as well as the IS and CS groups, are shown in Table 1. Both groups were adjusted regarding all the variables collected except for age, which was slightly greater in the IS group (69±12 vs 67±12 years; P=.02).
Management in the Invasive and Conservative Groups
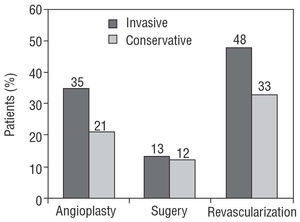
The initial management of platelet aggregation inhibitors and anticoagulants was similar in the IS and CS groups: acetylsalicylic acid, 96% versus 97% (P=NS), and low-weight heparin 89% versus 90% (P=NS). Clear differences in management were found between the IS and CS groups during admission. Use of the exercise stress test in the IS group was reduced by 64% (13% vs 36%; P<.0001). However, cardiac catheterization increased by 20% in the IS group (73% vs 61%; P=.006), percutaneous revascularization by 67% (35% vs 21%; P<.0001) and percutaneous or surgical revascularization by 45% (48% vs 33%; P=.001). No differences were found regarding surgical revascularization (13% vs 12%) (Figure 1, Table 2).
Figure 1. During the intention to treat invasively period, predischarge angioplasty (P<.0001) and predischarge revascularization (P=.001) significantly increased, but not predischarge coronary revascularization surgery.
In the CS group cardiac catheterization was carried out in 167 (61%) patients due to refractory angina in 62 patients, heart failure or hemodynamic instability in 41 patients, and pre-discharge positive exercise stress test in 64 patients. Cardiac catheterization was not carried out in 62 (27%) patients in the IS group, due to patient refusal in 15 cases, previous non-revascularizable study in 12 patients, some type of contraindication in 8 cases, death prior to the study in 2 cases and by the decision of the acting physician in 25 patients.
There were no significant differences between the IS and CS groups regarding hospital stay (9±6 vs 9±7 days) or the day on which catheterization was carried out (4±3 vs 4±3 days).
Regarding the management of patients treated with percutaneous revascularization (n=139), no differences were observed between the IS period (n=82) and the CS period (n=57) concerning the use of stents (92 vs 92%; P=NS) or the use of IIb/IIIa inhibitors (41% vs 41%; P=NS) (Table 2).
Differences Between the Invasive and Conservative Group Regarding Events
During hospital admission a reduction in refractory angina in the IS group was found (12% vs 23%; P=.004), with a nonsignificant reduction in mortality (4% vs 7%; P=NS) and a nonsignificant increase in infarction (6% vs 4%; P=NS) in the IS group. No differences were observed between the 2 groups regarding major events during admission (IS, 10%; CS, 11%; P=NS).
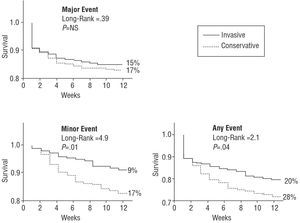
During the 12-week follow-up, no significant differences were found between the IS and CS groups regarding mortality (6% vs 9%; P=NS), infarction (10% vs 10%; P=NS) and major events (15% vs 17%; P=NS) (Table 3, Fig. 2). In the multivariate study, after adjusting for the rest of the variables, the IS yielded a nonsignificant trend toward a reduced probability of a major event during follow-up: HR=0.6; 95% CI, 0.4-1.1; P=.09 (Table 4).
Figure 2. Kaplan-Meier survival curve analysis comparing event-free survival in the intention to treat invasively and intention to treat conservatively periods during 12-week follow-up. During the invasive period a nonsignificant trend was found toward fewer major events (death or infarction, upper left) and a significant reduction in minor events (readmission for acute coronary syndrome or postdischarge revascularization, lower left) and of any event (minor or major, lower right). NS indicates nonsignificant.
During follow-up, the IS was related to a lower probability of readmission for acute coronary syndrome (9% vs 16%; P=.03), post-discharge revascularization (2% vs 7%; P=.006) and a minor event (9% vs 17%; P=.01) (Figure 2). In the multivariate study, after adjusting for the remaining variables, the IS was related to a smaller probability of a minor event during follow-up: HR=0.5; 95% CI, 0.3-0.8; P=.008 (Table 4).
Finally, the IS group showed a lower incidence of any event (major or minor) during follow-up (20% vs 28%; P=.04) (Figure 2). After adjusting for the rest of the variables, the IS was independently related to a lower probability of any event during follow-up: HR=0.5; 95% CI, 0.3-0.8; P=.005 (Table 4).
After analyzing 383 (76%) patients with elevated troponin I, the same trend as in the group as a whole was found when comparing the IS and the CS regarding major events (15% vs 20%; P=NS), minor events (7% vs 16%; P=.02) and any event (20% vs 27%; P=.1).
DISCUSSION
The main findings are that in patients admitted for NSTEACS with high-risk criteria, intention to treat invasively made it possible to reduce the events due to the decreased need for readmission or postdischarge revascularization. When comparing this with intent to treat conservatively (optimized according to the current guidelines), major events were not significantly reduced with IS.
Previous Studies
Numerous studies have attempted to compare a CS with an IS in the management of NSTEACS, but only 5 of these have had a real impact on the scientific community because they were random trials with a sufficient number of patients enrolled.4-8
The TIMI-IIIB study4 was carried out between the end of the 1980s and beginning of the 1990s. No reduction was found in major events, but there was a clear reduction in minor events during follow-up. The VANQWISH5 study was carried out at the beginning of the 1990s. This study had an impact on clinical practice since it showed an increase in events.
The intense changes occurring in the areas of redefining acute coronary syndrome,12 risk stratification (troponins, the prognostic value of changes in ECG),13-18 medical treatment and improvements in invasive treatment (intracoronary stents)3 have made new studies necessary which are more in keeping with the current situation.
The FRISC-26 study was the first to clearly demonstrate a reduction in major events and the only one that found a reduction in mortality with an IS. The management of the conservative group was far from what is normal in our setting: a strongly positive exercise stress test was required in order to carry out catheterization in this group, and only 9% of the patients were revascularized before discharge (vs 71% in the invasive group). This "excessively conservative" management could magnify the differences in favor of invasive treatment. The maximum benefit with the IS was found in the patients with elevated troponin or depressed ST segment.19
The TACTICS study8 attempted optimal management (which is difficult to fulfill in daily practice), by using glycoprotei n IIb/IIIa inhibitors in all cases and catheterization (in the invasive group) between the 4th and the 48th hours. Once again, the readmission rate for acute coronary syndrome was dramatically reduced, whereas the reduction of major events (due to infarction but not of death) was only just significant.
The RITA-39 study is the most recent one with a management approach very similar to the registry we present. A reduction was found in combined death-infarction-refractory angina events at 4 months with the IS, mainly due to a lower rate of angina. The combined death-infarction event decreased, albeit in a nonsignificant way, after a year in the invasive group.
Bearing all this in mind, the most recent guidelines already recommend a routine IS in the patients with high-risk NSTEACS.9,10 In any case, the extrapolation of the data observed in large studies to daily practice is always complex due to the different characteristics of the patients (in general, there is more risk in the real world) and the difficulty in strictly applying the recommendations (it is Utopian to assume that every patient with NSTEACS with elevated troponin or changes in ECG will undergo catheterization).
The Current Study
In our center we began with a 2-year period, strongly motivated by risk stratification in NSTEACS,11,13,15-18 with the development of a chest pain unit and the attempt to properly manage these patients in line with current recommendations.20
Following the guidelines,9,10 clinicians and catheterization specialists jointly decided to carry out catheterization and revascularization whenever possible in patients with NSTEACS with elevated troponin or changes in ECG. During year 1 (October 2002-September 2003), this "intention to treat invasively" approach was applied and its evolution was compared over 3 months with the group with the same characteristics included in our chest pain unit registry during the immediately previous 1-year period (October 2001-September 2002), which was managed with an "intention to treat conservatively" approach.
Recommendations for an IS was reflected both in the management of the patients by the clinicians (exercise stress test was reduced by a third and catheterization increased by 20%), and especially by the catheterization specialists (angioplasty increased by 67%). The reduction of refractory angina from 23% to 12% is probably explained by the different therapeutic approach (direct intention to treat with catheterization in the invasive group, whereas in the conservative group one of the indications was to wait for the reappearance of this symptom).
With regard to patient evolution, the results generally coincide with the last three random trials. A reduction was achieved in events due to fewer minor events: readmission and post-discharge revascularization. Both groups were adjusted regarding baseline characteristics, although the invasive group were older (Table 1). Previous studies have demonstrated that being older is related to worse prognosis in the unstable patient11,15 as well as fewer interventions.21 In our series, age was an independent predictor of all events; thus, after adjustment in multivariate analysis, the benefit contributed by the IS was still greater regarding the reduction of minor events and any event, with a 50% reduction in the adjusted risk of a minor event and of any event (95% CI, 30%-80%).
Regarding major events, no harmful effect was found with the IS, but a trend was found (almost significant when adjusting for the remaining variables) toward the reduction of events with intention to treat invasively; some results were similar to the ones found in the TACTICS7 and RITA-38 studies and worse than in the FRISC-26 study where the conservative arm was probably penalized by an excessively conservative approach.
These data suggest that a CS in which interventions are applied rationally is capable of achieving a similar rate of major events as routine IS, although the latter makes it possible to reduce the percentage of readmissions and post-discharge revascularization.
Finally, it is worth pointing out some differences with large studies when transferring the IS to the real world (Table 5). Age and the percentage of diabetics (the main clinical variables related to prognosis) are clearly higher than that found in random studies and similar to registries in our setting,22 which reflects the worst baseline profile of patients in the real world and can also explain the higher rate of events. The pre-discharge use of catheterization in the invasive group was high (73%) but less than in the random studies (>90%),4-8 due to the difficulty of applying this technique in daily practice to all the patients (e.g. patient refusal, history of a non-revascularizable study, baseline characteristics, clinician's decision). However, the use of catheterization and revascularization in the conservative group was higher than in the majority of the random studies.4-8 This suggests a bias toward little intervention in the conservative group in previous studies and underlines the benefit, in terms of reductions in minor events, found in our series with "intention to treat invasively" when comparing it with an optimal CS.
Limitations
Obviously, our series does not reflect the results of a random study, with all the limitations this involves. Furthermore, our study did not strictly compare a CS versus an IS in patients with NSTEACS, but rather two cohorts of patients with NSTEACS managed with a more or less invasive treatment strategy. On the other hand, a greater number of patients or a more prolonged follow-up could modify the results, although marked changes in the trends presented are unlikely, when observing the temporal evolution of previous studies.6,7
CONCLUSIONS
The most solid conclusions of recent large studies have been confirmed in the real world. The IS in high-risk NSTEACS is capable of reducing short-term events, especially lowering the probability of readmission for acute coronary syndrome and post-discharge revascularization. Compared to an optimal CS, intention to treat invasively does not significantly reduce the rate of major events.
This work was financed with grant PI-106/2004 from the Escuela Valenciana de Estudios para la Salud (EVES), Conselleria de Sanitat de la Generalitat Valenciana, and grant 1/2003 from the Societat Valenciana de Cardiología.
Correspondence: Dr. V. Bodí.
Servicio de Cardiología. Hospital Clínic i Universitari.
Avda. Blasco Ibáñez, 17. 46010 Valencia. España.
E-mail: vicentbodi@hotmail.com