To the Editor,
Transposition of the great arteries (TGA) is the most common type of cyanotic heart disease in newborn infants. The atrial switching procedures (Mustard and/or Senning procedures) have permitted these infants to survive to adulthood.1 Sudden death is a substantial cause of late mortality. Presence of flutter or atrial fibrillation, syncope, or heart failure are predictors of sudden death in such patients.2 Ventricular arrhythmias are uncommon when ventricular dysfunction is not present. Implantation of an implantable cardioverter-defibrillator (ICD) can be a complex procedure and, although there have been reports of implantation using the subclavian venous approach,3 this might not always be feasible.
We present the case of an adolescent girl with TGA who underwent implantation of a atrio-biventricular ICD.
The 16-year-old patient had been born with interventricular shunting and persistent ductus arteriosus. She had undergone a Rashkind balloon atrial septostomy and, when 6 months old, a Mustard-type repair. For several years, she had asymptomatic paroxysmal complete atrioventricular block with narrow QRS interval and was in functional class II. She was admitted after cardiogenic syncope. An ejection fraction of 25% was observed in the echocardiogram and there were no obvious abnormalities in the baffles for redirection of atrial flow. We performed a catheterization study with induced syncopal ventricular tachycardia, with cardioversion at 200J. It was decided to place an ICD and resynchronize because of the possible need for antibradycardia pacing as she had a history of CAVB with severe systemic ventricular dysfunction. Implantation by the subclavian approach was impossible as the electrode could not be advanced further than the upper area of the right atrium. It was decided to operate and place an epicardial pacing system. During opening of the sternum, rupture of the right ventricle occurred, requiring extracorporeal circulation and repair with sutures and Teflon. Epicardial pacing and sensing electrodes were placed on the right atrium and both ventricles. In addition, conventional 2-coil defibrillation electrodes were placed in the pericardial sac, around both ventricles, and were fixed with loose stitches. The electrodes were tunneled until reaching an infraclavicular left subcutaneous bag and a high-energy (41J) Guidant Contak Renewal 4 generator was implanted. It was confirmed that defibrillation was effective with 21J and pacing thresholds less than 1V in the 3 chambers. During the postoperative period, the patient developed bacteriemia due to Serratia, which was successfully treated with a targeted antibiotic. The patient was discharged after 20 days. After 18 months of follow-up, she had not had any arrhythmic episodes and the device is currently functioning normally (Figure 1).
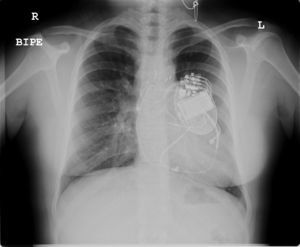
Figure 1. Posteroanterior chest X-ray. Three pacing/sensing electrodes can be seen, along with the defibrillation electrode surrounding both ventricles.
The increased number of ICDs in pediatric patients with congenital heart diseases faces, among other problems, the limitations of percutaneous access in many patients, either because of small vessel size or the particular anatomy of the patient. The traditional placement of epicardial patches is associated with problems of pericardial restriction and increases in the defibrillation thresholds. Stephenson et al4 and Cannon et al5 both published series (22 and 8 patients, respectively) with complex heart diseases and alternative approaches: a) implantation of 1 to 3 subcutaneous electrodes as the high-energy electrode or the transvenous defibrillation electrode itself in a subcutaneous position4; b) transatrial approach with implantation of the defibrillation electrode directly through the right atrium5; and c) implantation of the defibrillation electrode in the pericardial sac.4,5
Given the small number of patients and the limited follow-up, it is hard to predict the complications associated with these procedures in the medium term. Stephenson et al4 proposed annual monitoring of the defibrillation thresholds, which can become fundamentally elevated with subcutaneous electrodes. Cannon et al5 recommend performing an annual echocardiography when there are electrodes in the pericardial sac to detect the possibility of progressive strangulation of the myocardium. This technique is considered preferable in patients with larger body surface areas,4 as was the case in our patient.
Due to the increase in the population with congenital heart disease reaching adulthood, we will need to use this and other approaches increasingly often.
Corresponding author: sugonzalez@humv.es