A 58-year-old woman with history of congenital heart defect presented to the pulmonary hypertension (PH) center in World Health Organization functional class III.
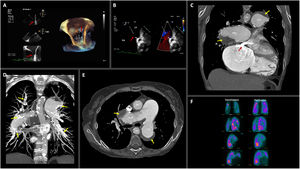
A transesophageal echocardiogram demonstrated an ostium secundum atrial septal defect with 14 x 11mm diameter (figure 1 A-B, red arrows, left atrium [LA], right atrium [RA]) and dilated right heart chamber. Right heart catheterization with compartmental oximetry for calculating pulmonary blood flow/systemic blood flow (Qp/Qs) depicted PH with a precapillary phenotype [mean pulmonary artery pressure of 66mmHg, pulmonary vascular resistance of 11.4 WU and pulmonary capillary wedge pressure of 13mmHg] alongside a Qp/Qs of 0.9. Specific PH drugs were started in an upfront combination, including a phosphodiesterase type 5 inhibitor and an endothelin receptor antagonist.
Contrast-enhanced chest computed tomography revealed aneurysmal pulmonary arteries partially filled with chronic, laminated, and calcified fibrothrombotic deposits (figure 1 C-E; yellow arrows, right pulmonary artery [RPA], left pulmonary artery [LPA], right upper pulmonary vein [RUPV], left atrial appendage [LAA], aorta [Ao], left ventricle [LV], right ventricle [RV]).
At this stage, differential diagnosis with distinct nosological entities is of upmost importance. The differential diagnosis should include: a) in situ thrombosis due to dilation of pulmonary arteries with stasis, endothelial dysfunction, and a state of hypercoagulability secondary to severe pulmonary arterial hypertension. The etiology would be congenital heart disease: Eisenmenger vs coincidental atrial septal defect (due to its small size); and b) chronic thromboembolic PH with an incidental atrial septal defect.
In this context, a lung perfusion/ventilation scintigraphy was performed revealing multiple ventilation defects with no perfusion mismatch (figure 1F), thereby excluding chronic thromboembolic PH.
This clinical case illustrates in a paradigmatic way the existence of phenocopies regarding distinct pathological conditions. Adequate integration of all clinical elements and demonstration of the absence of ventilation/perfusion mismatch were key elements to correct diagnosis.
FUNDINGNone.
ETHICAL CONSIDERATIONSPatient informed consent was obtained.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence was used in the preparation of this manuscript.
AUTHORS’ CONTRIBUTIONSJ. Brito and R. Placido contributed equally to this work. Joana Brito contributed with conceptualization, writing, and editing. F.J. Pinto contributed with reviewing. Rui Placido contributed with conceptualization, reviewing, and supervision.
CONFLICTS OF INTERESTNone.