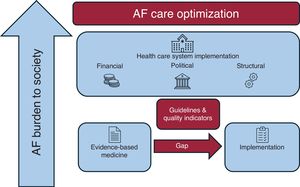
Among the European Society of Cardiology (ESC) member countries, there is a median of 95 cardiologists per million people, amounting to over 60 000 cardiologists across Europe who manage nearly 49 million people with cardiovascular disease. The economic impact on health care across European countries is significant and has been estimated at €210 billion a year. Given that more than 10 million Europeans are diagnosed with atrial fibrillation (AF), a substantial portion of the health care budget is allocated to AF care. This care includes not only the treatment of the arrhythmia per se, but also its associated comorbidities such as stroke, heart failure, and cognitive impairment.1 Therefore, optimizing health care resources for AF care is highly relevant and requires complex coordination of regional financial, political, and structural aspects in each health care system. Importantly, it can also be achieved through the implementation of evidence-based medicine.
In the context of evidence-based medicine, the exponential increase in published studies on AF reflects a growing emphasis on generating robust clinical evidence to guide treatment and management strategies. In 2023 alone, nearly 8 000 papers were published on AF. Consequently, cardiovascular societies face the challenge of evaluating this vast amount of scientific data and condensing it into clinical guidelines designed to provide an up-to-date, concise, and accessible document for clinicians and allied professionals.2 The greatest challenge for clinical societies, however, may not lie in drafting guidelines but in effectively implementing them in everyday clinical practice. Numerous reports indicate considerable variability in guideline adherence among countries (figure 1).3,4 Not surprisingly, improved guideline implementation is associated with better outcomes. For example, data from the Eurobservational Research Programme in AF (EORP-AF) on antithrombotic therapy in AF patients and outcomes demonstrated that good adherence to guideline-recommended therapies (antithrombotic therapy in AF) was associated with increased survival.5
Flowchart depicting the main features of optimization of atrial fibrillation (AF) care. This is represented by the interplay between regional financial, political and structural aspects for each health care system, in parallel with the implementation of evidence-based medicine through guidelines and quality indicators.
Furthermore, the recently presented STEEER-AF randomized trial6 reported improvements in guideline-adherent provision of AF care in European centers (France, Germany, Italy, Poland, Spain, and the United Kingdom) randomized to a structured educational program for health care professionals. Unfortunately, the analysis showed overall poor adherence to AF guideline recommendations. In the intervention group, adherence was only 68% for stroke prevention and 34% for rhythm control. Prof Dipak Kotecha, the chief investigator from the University of Birmingham (UK), commented “While guidelines, such as those from the ESC, aim to support health care professionals in applying optimal care, their recommendations are often not implemented in clinical practice, with the education of health care staff identified as a major barrier”.6
To improve the implementation of evidence-based medicine, as outlined in clinical guidelines, several professional societies have developed quality standards, clinical indicators, and quality measures. In 2021, the European Heart Rhythm Association (EHRA), in collaboration with the Heart Rhythm Society (HRS), the Asia Pacific Heart Rhythm Society (APHRS), and the Latin-American Heart Rhythm Society (LAHRS), published a joint document establishing specific AF quality indicators (QIs).7 They identified 6 domains of care for the diagnosis and management of AF: a) patient assessment (baseline and follow-up); b) antithrombotic therapy; c) rate control strategy; d) rhythm control strategy; e) risk factor management; and f) outcome measures.
These QIs aim to evaluate the quality of AF care and provide mechanisms to assess the effectiveness of quality improvement initiatives. The consensus document was published concurrently with the 2021 ESC AF guidelines, in which it received a Class IIa recommendation (level of evidence: B).8
We therefore read with interest the work by Ruiz-Ortiz et al.,9 who analyzed AF care according to EHRA AF QIs using a SEC-EXCELENCE in AF registry (part of a strategy for quality improvement for cardiovascular diseases, SEC-CALIDAD).10 The study was based on retrospective data from medical records of consecutive adults (n=797) with an AF diagnosis who received medical attention over 1 week in 2019 at 9 Spanish centers. The annual rates of total mortality, stroke and major bleeding were 8.1, 0.8, and 2.6 per 100-patient/y, respectively. Seventy percent of patients with symptomatic paroxysmal or persistent AF were offered catheter ablation after antiarrhythmic drug failure, and very few patients with structural heart disease or end-stage kidney disease were inappropriately prescribed flecainide/propafenone or sotalol/dofetilide, respectively.
However, the results in the domains of patient assessment and anticoagulation were less satisfactory. In particular, documentation of CHA2DS2VASc and HAS-BLED scores was low (25%) and very low (6%), respectively. Although the rate of appropriate anticoagulation in high-risk patients was high (93%), a significant proportion of low-risk patients (58%) were also on anticoagulation (presumably not guideline-indicated). Regarding risk factor management, the 7 modifiable risk factors proposed by the ESC were documented in only 59% of the patients. Interestingly, the authors also assessed potential differences in QIs between general cardiology centers and tertiary referral centers (the latter defined by the presence of an electrophysiology laboratory and cardiovascular surgery services). While general cardiology centers showed better adherence in assessing cardioembolic risk, there was no significant difference between the types of centers in the anticoagulation and outcome domains.
The 2024 version of the AF guidelines has introduced changes to simplify thromboembolic risk stratification, including the use of the CHA2DS2-VA score instead of the CHA2DS2-VASc score and the removal of the HAS-BLED score,2 which may aid implementation in the future.
Currently, only 2 other European studies have evaluated AF QIs,11,12 and we would like to congratulate the authors for their efforts in highlighting the need to evaluate health care processes to identify areas for improvement. Furthermore, it is reassuring that the outcomes of AF care do not seem to depend on center complexity, at least among the participating centers. However, the study has some major limitations, most of which are inherent to its design and have been appropriately acknowledged by the authors.
The outcome analysis does not include data from hospital admissions at centers outside the publicly funded national health service, which may lead to underreporting of clinical events given the presence of a substantial number of private centers in Spain. In addition, although data collection was performed exclusively by clinicians with care responsibilities (cardiologists or cardiology residents) under the supervision of the principal investigators, no external audit of data quality was performed, which may have led to inaccuracies. Missing data (ie, risk factors) may partly explain the high proportion of patients with a CHA2DS2VASc of 0 (or 1 for women) who were nonetheless anticoagulated. Lastly, and most importantly, extrapolating the study results to other Spanish centers is difficult, as all participating centers had shown an active interest in improving AF management by participating in SEC-EXCELENCE. Consequently, lower QI scores might be expected in other centers.
Overall, the results of Ruiz Ortiz et al.9 and other studies evaluating AF care quality through QIs and clinical guideline implementation3,4,6,11,12 reach the same conclusion: there is room for improvement. It is therefore paramount to continue working toward closing the gap between the publication of clinical guidelines and their implementation in our health care systems. Continuous QI assessments and other guideline implementation analyses are therefore a necessity to to get closer to practice what we preach as a clinical society.
FUNDINGNo funding was received for the present article.