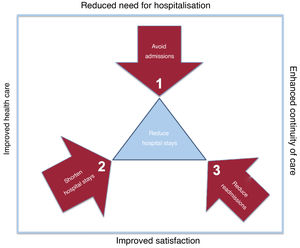
Care outcomes in cardiology inpatient units do not depend exclusively on their internal functioning. The main quality indicators of hospitalization units are determined by the influence of external factors that are dependent on other cardiology service units, other hospital services, the emergency department, or the organization of care for chronic cardiovascular disease.1 From this perspective, it seems reasonable to suggest that it should be the hospitalization units themselves that, by extending their boundaries, promote and participate in the implementation of strategies to positively influence these factors. This approach is what we define as “extended hospitalization” (figure 1).
Within the service itself, cardiology hospitalization units should ensure the prompt performance of complementary tests by managing delays and establishing agreements and prioritization criteria with the imaging, electrophysiology, and cardiac catheterization units. The cancellation of scheduled diagnostic and therapeutic procedures should be minimized, because, in addition to interfering with the effectiveness and efficiency of health care, it has relevant negative implications for the patient's perception of service quality and is a frequent cause of complaints. Promoting bedside echocardiography by physicians in the hospitalization unit avoids patient travel, improves satisfaction and the doctor-patient relationship,2 and reduces the workload of the imaging units by reserving their participation for doubtful or more complex cases. In addition, it provides enormous educational value, because it allows the immediate establishment of correlations with exploratory findings. This aspect facilitates the improvement of these skills which, sadly, are currently in disuse. These advantages can be extended to the use of techniques such as signal-averaged electrocardiography or vectorcardiography, whose use, despite their proven clinical benefit, is unjustifiably marginal.
Beyond the boundaries of the cardiology department, the establishment of rapid and efficient cardiology care in the emergency department by hospitalization unit physicians reduces the need for hospitalization by avoiding unnecessary admissions and shortening hospital stays, given that specialized assessment of patients is guaranteed from the early stages of hospital care. Interdepartmental consultation in hospitals, a role model service for the rest of the hospital, is a complex medical activity with high health care value, and should therefore be promptly and efficiently performed. Prioritizing interdepartmental consultation among hospitalization units, while committing to promptness and efficiency, projects an image of excellence to the rest of the hospital's specialties, promotes a positive feedback effect regarding the resolution of requests from the cardiology service, and establishes an ideal platform for the development and integration of multidisciplinary units.
During the discharge process, it is essential to systematize the clinical report, which must be accurate, concise but complete, reliable, objective and, above all, clear and intelligible. The use of acronyms and abbreviations should be minimized or avoided and never be used in diagnoses and recommendations because they contribute nothing to the quality of care, beyond saving the person preparing the report a certain amount of effort. In its preparation, it should be taken into account that it is aimed at patients, caregivers, primary care physicians, other cardiologists, other specialist physicians, and coders, and should be of use to all of them. At the time of discharge, it should be ensured that prescribed medications are reconciled with those already taken by patients, and that patients and caregivers should fully understand the therapeutic recommendations and the adjustments that have been established in their medication list.
Finally, strategies should be developed to minimize readmissions. Continuity of care and early discharge can be facilitated and guaranteed by providing a telephone number and contact person to resolve questions or communicate incidents arising in the first few weeks after discharge, having an “open door” policy, and providing early consultation after discharge by the cardiologists who attended the patient during admission.
In conclusion, given that hospital admission generates large amounts of knowledge about the health of patients that we should capitalize on, progress must be made toward hospitalization units extending their boundaries and committing to the development of strategies to improve quality of care, guarantee continuity of care, and reduce the need for hospitalization (figure 2).
FUNDINGNone declared.
AUTHORS’ CONTRIBUTIONSBoth authors contributed to the original concept, performing the project, and writing the manuscript.
CONFLICTS OF INTERESTNone declared.