Keywords
INTRODUCTION
The first artery that originates in the right coronary artery (RCA) is the pulmonary conus artery, or conus artery. In a variable proportion of the population (between 30% and 50%), this artery originates in an independent ostium in the right sinus of Valsalva, anterior and superior to the ostium of the RCA.1
When this is the case, this artery is described as "the third coronary."2 The anterior and superior course of the conus artery is usually short, and irrigates the pulmonary infundibulum and the supraventricular crest. Occasionally, it forms an anastomosis with the left anterior descending artery (left conus artery), thus forming the so-called "arterial circle of Vieussens." In the present article, we describe the clinical and angiographic characteristics of 3 patients with occlusion in the left coronary artery and collateral circulation through a large conus artery up to the proximal and medial segment of the anterior descending artery.
METHODS
The patients described in this article were admitted to our center between February 2006 and December 2008. They all underwent cardiological studies due to angina-like precordial pain episodes. Diagnosis was conducted using coronary angiography and 64-slice multidetector computed tomography (MDCT).
RESULTS
The clinical and angiographic characteristics of the patients are described below and presented in Table.
Case 1
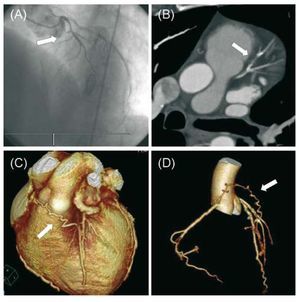
A 54-year-old man, smoker, with hypercholesterolemia, was referred to the center due to stable effort angina pectoris of 3 years duration. He presented inferior Q wave in the basal electrocardiogram (ECG). The echocardiogram showed inferoposterior hypokinesia with a left ventricular ejection fraction (LVEF) of 55%. Coronary angiography demonstrated an independent origin of the LAD and circumflex arteries. The LAD was proximally occluded, and it was impossible to view its distal bed. The RCA was occluded at the distal segment and received homocoronary and heterocoronary collateral vessels from the circumflex artery. Given that anterior contractility was normal, and that coronary revascularization was planned, MRCT was requested to assess the bed distal to the LAD occlusion. The MRCT revealed a conus artery with an independent origin in the right sinus of Valsalva and that provided flow to the LAD from its medial segment and filled its distal bed (Figure 1). Based on these findings, myocardial revascularization was indicated, but the patient refused this procedure. The symptoms improved, but did not disappear, after intensifying the medical treatment.
Figure 1. Case 1. A: anteroposterior view of left coronary angiography; the anterior descending artery is occluded at a proximal level. B: MRCT image processed with MPR (multiplanar reformatting) that shows an occluded segment in the anterior descending artery. C and D: 3D volume rendering reconstruction of MRCT that shows the course of the conus artery until it joins the anterior descending artery.
Case 2
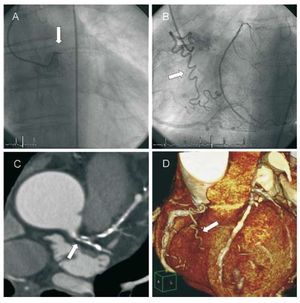
A 74-year-old man, smoker, was admitted to our center due to unstable angina. The basal ECG presented left anterior hemiblock. During admission, he presented a new episode of precordial pain and ECG showed ST-segment elevation of 1 mm in aVR and aVL, with a ST-segment depression of 2 mm in V4-V6 and in leads II and III and aVF. Transthoracic echocardiogram showed mild anterolateral hypokinesia, with an LVEF of 50%. Coronary angiography demonstrated total occlusion of the left main coronary artery (LMCA) at its proximal segment. The LAD was filled by the collateral circulation through a large conus artery that originated within the right sinus of Valsalva, very close to the ostium of the RCA. It coursed with the LAD at the medial segment after following a long and tortuous course. The circumflex artery was not visualized and the RCA was dominant without any significant stenosis. In order to evaluate the relationship between the conus collateral circulation and the sternum before the intervention, MRCT was conducted and this showed a coronary anatomy that matched with the results of the coronary angiography (Figure 2). Coronary revascularization was conducted using a left internal mammary artery graft to the medial segment of the LAD. Patient evolution was good.
Figure 2. Case 2. A: anteroposterior view of left coronary angiography; the left main coronary artery is occluded at the proximal level. B: left anterior oblique view of coronary angiography showing the long and tortuous course of the conus artery. C: multidetector computed tomography image processed with MPR (multiplanar reformatting) that shows occlusion in the left main coronary artery, and that includes the proximal part of the anterior descending and circumflex arteries. D: 3D reconstruction of MRTC that shows the course of the conus artery.
Case 3
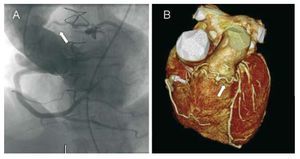
A 60-year-old hypertensive man, surgically treated 12 years earlier for aneurysm in the aortic root. A composite Dacron tube graft with a Carpentier bioprosthetic valve was implanted and coronary reimplantation performed using the Cabrol technique. He was admitted to hospital with symptoms of progressive effort angina pectoris. The ECG showed negative and nonspecific T waves in V1-V2. Global and regional wall motion were normal on echocardiogram. Catheterization of the left coronary artery during coronary angiography was not successful. However, this artery was filled from the RCA through a large conus artery that connected with the LAD at its proximal segment. Due to the patient's history of aortic surgery, the failure to catheterize the left coronary artery, and the need to plan the best surgical approach, MRCT was conducted. It demonstrated proximal occlusion of the LMCA and collateral circulation through the conus artery, with excellent angiographic correlation (Figure 3). The patient underwent coronary revascularization and the left mammary artery used as a sequential graft to the ramus intermedius and the LAD. Patient evolution was good.
Figure 3. Case 3. A: aortogram where the left coronary trunk is not visualized; the left coronary artery is filled through the conus artery. B: 3D reconstruction of MRTC that shows the course of the conus artery.
DISCUSSION
Collateral circulation is a key factor fact in the pathophysiology of coronary disease. The symptoms and prognosis among coronary patients depend on the quality of collateral circulation. We describe 3 patients of left coronary tree occlusion and collateral circulation via a large conus artery which joined the LAD after following a long and tortuous path. This anatomy could be considered a particular form of the so-called "circle of Vieussens," but the conus artery did not present secondary ramification or a capillary network in any of the patients. In patients 1 and 2, the conus artery presented an independent outlet in the right sinus of Valsalva. The first patient also had the peculiarity of presenting 4 different coronary ostia, since the LAD and the circumflex also presented independent ostia.
The collateral circulation from the conus artery was probably crucial, as deduced by the presence of preserved or minimally affected general and regional ventricular functions, regardless of other physiological factors (eg, ischemic preconditioning). Our report emphasizes the importance of always looking for anatomical variants on coronary angiography, especially when LMCA occlusion or equivalent is present and preserved left ventricular function.3 In up to 20% of coronary angiographies, the conus artery is not visualized, mainly due to its independent origin or within the first millimeters of the RCA.1 The clinical implications of this are not only diagnostic, but also therapeutic. It is fundamental for the surgeon to know the origin of the conus artery and its course in order to avoid causing damage during surgery. Surgical interventions involving manipulation of the right infundibulum present the risk of damaging the conus artery, especially when it is partially hidden by an intramyocardial pathway. In the percutaneous treatment of chronic occlusion of the LAD, simultaneous injection through the conus artery has been described as useful in visualizing the distal segment of LAD and advancing the guide correctly. It could even serve as an alternative to the retrograde route when the lesion cannot be successfully crossed using an anterograde approach.3
Multidetector computed tomography has recently been developed for the study of coronary disease. One of the applications of this new technique is the study of distal beds in patients with coronary occlusion.4 This is of special interest in patients referred to surgical coronary revascularization.
Case 1 is a good example of this application, since the distal LAD could not be visualized during coronary angiography. Multidetector computed tomography is the definitive test to study variants in coronary anatomy that could be overlooked in coronary angiography.
In patients 2 and 3, there was chronic occlusion of the LMCA, a very infrequent angiographic finding (between 0.03% and 0.06%, according to different series).5 The clinical signs are nonspecific and cannot be distinguished from other less severe forms of coronary disease. The presence of ventricular wall motion abnormalities is quite common, whereas normal ventricular function is an exception.6
In conclusion, we emphasize the usefulness of MRCT for the study of distal beds in patients with coronary occlusion, as well as for studying the collateral circulation, especially when there is a conflict between the findings of coronary angiography and ventricular function.
Correspondence: Dr. J.A. de Agustín.
Unidad de Imagen Cardiovascular. Hospital Clínico San Carlos. Prof. Martín Lagos, s/n. 28040 Madrid. Spain.
E-mail: albertutor@hotmail.com
Received January 24, 2009.
Accepted for publication June 18, 2009.