Dual atrioventricular nodal (AVN) physiology is an established cause of AVN reentrant tachycardias, of which the slow-fast variant is the most frequent.1 We present a patient with a mistaken diagnosis of AVN reentrant tachycardia referred for ablation. She actually had a tachycardia due to dual ventricular response, an uncommon presentation of tachycardia due to the presence of dual AVN physiology. We present this case to emphasize the importance of a thorough analysis of the electrocardiogram (ECG) because this tachycardia is frequently misdiagnosed, especially for atrial fibrillation.2
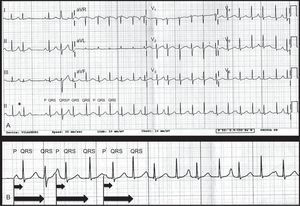
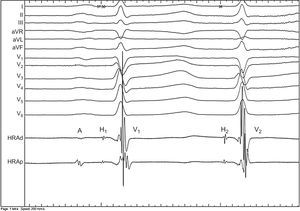
A 54-year-old woman without structural heart disease was referred to our center for an electrophysiology study and possible ablation of an AVN reentrant tachycardia because of persistent rapid palpitations despite treatment with a beta-blocker. On reviewing the ECG we noted a regular irregularity in the ventricular interval and the presence of P-waves, preceding every 2 QRS complexes. This and the positive morphology of the P-waves in the inferior leads ruled out a diagnosis of AVN reentrant tachycardia. A differential diagnosis of sinus rhythm with a dual ventricular response due to the presence of dual AVN physiology, junctional extrasystoles in bigeminy or (less likely) atrial tachycardia was made (Fig. 1). The intracardiac tracing of the electrophysiology study with a catheter positioned at the His showed the same phenomenon of dual ventricular response. A clear electrogram of the atrium (A) can be seen followed by 2 His potentials (H) and 2 ventricular electrograms (V). Because of the fixed relationship of both His- and V potentials to the preceding A, the diagnosis of dual atrioventricular response was found to be most likely (Fig. 2). We proceeded to perform an ablation of the slow pathway, eliminating the dual ventricular response. With programmed stimulation, as previously described in this journal,3 the absence of dual AVN physiology could be confirmed.
A: 12-lead electrocardiogram of the tachycardia. The third and fourth QRS complexes are preceded by one P wave. This phenomenon can thereafter be seen for every 2 QRS complexes, so in fact there is normal sinus rhythm with PP of 830ms (73 bpm) with a dual ventricular response leading to tachycardia with an RR of 350-390ms (154-171 bpm). PR1 is 150ms and PR2, slightly irregular, between 560ms and 610ms. A clear fixed relationship can be observed. The first P wave (*) is a supraventricular beat followed by one QRS, probably because of anterograde conduction block in the slow pathway and the fourth QRS shows aberrance (Ashman Phenomenon). B: Detail of the rhythm strip of lead II. P waves can clearly be seen.
Dual ventricular response to a single supraventricular impulse is a rare presentation of dual AVN physiology. Every supraventricular beat is conducted anterograde both through the fast and the slow pathway. To allow dual ventricular response there has to be retrograde unidirectional block in at least the slow pathway, but probably in both pathways, and critical conduction delay of the slow pathway that is at least greater than the refractory period of the distal common pathway. We excluded the presence of an (atypical) AVN reentrant tachycardia with 2:1 conduction to the atrium because of the positive morphology of the P-waves on the ECG. The disappearance of the dual ventricular response following ablation of the slow pathway, considered to be the gold standard for diagnosis,2 confirmed our suspicion. Sporadic junctional extrasystoles were excluded because of the fixed relationship between the His potentials after conducting through the fast and the slow pathway. Junctional extrasystoles typically have a less predictable coupling interval.2 Although we did not completely rule out the diagnosis of junctional parasystole, the criteria postulated by Massumi et al.4 of a parasystole with a fixed junctional rhythm and the presence of variable A to H2 and V2 intervals could not be met. Patients like ours are often misdiagnosed with other arrhythmias, some of which can lead to referral for unnecessary procedures. Dixit et al. described 3 patients of a total of 456 referred for atrial fibrillation ablation who were erroneously diagnosed with atrial fibrillation while truly having tachycardia due to the presence of dual AVN physiology. Two had runs of dual ventricular response and the other had an atypical AVN reentrant tachycardia. Ablation of the slow pathway was successful in all 3 patients.5 Wang reviewed the literature of dual AVN nonreentrant tachycardia and found 49 cases, reported in 44 citations. Most of these patients had a significant delay to the correct diagnosis (77%) and the most common specific mistaken diagnosis was atrial fibrillation (32%). As in our patient, the most common presentation was symptoms of palpitations and most patients had spontaneous dual AVN nonreentrant tachycardia entering the electrophysiology laboratory and did not need induction. They found a mean difference between the AH1 and AH2 of 350ms (± 52ms) and a maximum of 470ms.2 Our patient showed a difference of 519ms, much longer, as described. Our center also previously described 2 patients transferred for atrial fibrillation ablation while actually having an ECG with a regular irregularity and group beating, excluding atrial fibrillation.
Electrophysiological study in these 2 patients showed a tachycardia that could only be maintained by the participation of 3 different anterograde slow AV pathways conducting in a uniquely alternating sequence. These patients were also treated successfully with radiofrequent ablation at the posterior aspect of Koch's triangle.6 To prevent patient transfers for unnecessary procedures, thorough analysis of the ECG during tachycardia is of critical importance.
.