To the Editor:
Recognition of the ventricular rate by an implantable cardioverter defibrillator (ICD) is achieved through the local electrogram obtained from a bipolar electrode situated at the apex of the right ventricle. The amplitude of the electrogram can be drastically reduced during ventricular fibrillation (VF). Consequently, defibrillators incorporate an automatic gain or sensitivity control system to compensate for this phenomenon and ensure appropriate detection in almost all cases when the amplitude of the sinus rhythm is sufficient.1
We present the case of a patient carrying an ICD with adequate ventricular electrograms in sinus rhythm who presented a potentially lethal failure to detect an episode of VF due to the characteristics of the electrical signal during the arrhythmia. The patient was a man aged 65 years, diagnosed with ischemic heart disease associated with 3 vessels and severe ventricular dysfunction. In February 2004, a Guidant Contak Renewal II dual chamber defibrillator was implanted for primary prevention. During the procedure, various episodes of ventricular tachycardia (VT) with prolonged angina were mechanically induced and an induction test was therefore not performed at that time. In postoperative follow-up the electrode was shown to be correctly positioned in radiographs, stimulation impedances and thresholds were stable, and an electrogram of more than 10 mV was obtained in the detection channel in sinus rhythm (Figure 1). The patient refused a VF induction test prior to hospital discharge. The patient was readmitted to hospital 16 months later due to decompensated heart failure, which improved with medical treatment. Prior to discharge, the patient presented a sudden and prolonged loss of consciousness in the cardiology ward and resuscitation maneuvers were initiated with subsequent device discharge and recovery of the patient.
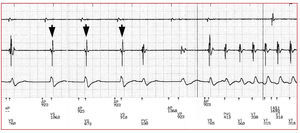
Figure 1. Recordings stored by the defibrillator during the episode. The traces correspond, from top to bottom, to the atrial electrogram, the ventricular detection channel, and the morphology channel. The adequate amplitude of the R wave during paced atrial rhythm can be seen (arrowheads). The onset of ventricular tachycardia is seen after the long cycle that follows a paced ventricular beat.
AP indicates atrial pacing; AS, atrial sensed; VS, ventricular sensed; PVC, premature ventricular contraction; VT, ventricular tachycardia beat; VF, ventricular fibrillation beat.
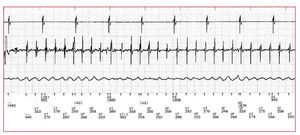
Interrogation of the device revealed an episode of VT with a cycle length of 310-320 ms that degenerated upon antitachycardia pacing to VF, clearly visible in the morphology electrogram (Figure 2). However, the detection channel displayed a relatively organized activity with periodic wide amplitude electrograms that were detected as VT beats and prevented recognition of the fibrillation. The device had antitachycardia pacing therapy programmed between 160 and 200 beats per minute; consequently, it administered various pacing bursts and even treated the episode as finished when intervals above the limit of detection for tachycardia were registered. Finally, detection in the VT zone was maintained for a sufficiently long period to allow pacing therapy to finish and administer the first programmed shock, which terminated the episode of fibrillation some 5 minutes after its onset. The failure to detect the ventricular signal for this reason is very rare. Dekker et al2 recently published a similar case in which they observed a detection failure occurring via the same mechanism during an induction of VF. Those authors reviewed their experience and did not find any similar case in more than 400 implanted devices. The mechanism responsible for this phenomenon remains to be elucidated. It has been suggested that heterogeneous conduction and/or refractoriness could lead to entrance block in the region of the electrode and reduce the frequency of local activation.2 In addition, modulation of ion currents due to local cytoskeletal changes could slow and organize fibrillatory waves.3 Whatever the cause, the phenomenon could be lethal for the patient by delaying or aborting therapy for VF. It is likely that an induction test during implantation would have facilitated early recognition of the problem in the patient presented here and would have allowed exploration of other regions of the right ventricle with a more appropriate signal for detection of VF.
Figure 2. Recordings from the device during the same episode and with the same organization of the channels shown in Figure 1. Ventricular fibrillation is visible in the morphology channel, while the detection channel records a rhythm with quite regular signals that are of larger amplitude, interpreted by the device as tachycardia beats alternating with ventricular fibrillation.
AP indicates atrial pacing; AS, atrial sensed; VS, ventricular sensed; PVC, premature ventricular contraction; VT, ventricular tachycardia beat; VF, ventricular fibrillation beat.