The bioresorbable everolimus-eluting vascular scaffold (Absorb-BVS, Abbott-Vascular; California, USA), designed to reduce late complications of bare-metal stents, received the CE mark in 2011 and became available in Europe in 2012. Although the initial results were promising, recent studies have brought into question the safety of the device due to a high incidence of thrombosis and infarction.1 However, little has been said about the resorption of the device or the structural and functional recovery of the vessel in patients in real-life clinical practice.
We present a single-center prospective cohort study that examined the structure and function of the coronary arteries after Absorb-BVS implantation, using angiography, optical coherence tomography (OCT), and quantitative flow ratio (QFR) in a consecutive series of patients with 5 years of follow-up. The coronary arteries were assessed retrospectively with 3-dimensional reconstruction angiography (QAngio XA-3D research edition 1.0, Medis Special BV; the Netherlands) and OCT images were obtained with Dragonfly catheter at 180 cps and 18mm/s (C7Fourier-Domain System, LightLab-Imaging, Inc.).
OCT analysis (of the treated segment and 5mm adjacent) was performed with LightLab software at 1mm intervals (Abbott; Abbott Park, USA). The markers on the Absorbs-BVS, angiography, and anatomical references were used to locate the treated segment. The morphological aspects studied were: resorption of the device, lumen area, asymmetry index, eccentricity index, residual stenosis area, neointimal thickness, minimum plaque thickness, and side branch ostia.2 These parameters were also reassessed after the intracoronary administration of 200μg of glyceryl trinitrate as part of the functional study.
Data were analyzed with the chi-squared test and Fisher exact test (categorical variables) and with the Student t test for paired data (continuous variables). The Shapiro-Wilk test confirmed normality. P ≤ .05 was considered statistically significant and the analyses were performed with IBM-SPSS-23.0.
Eleven Absorb-BVS were analyzed in 9 patients. Mean age was 70 ± 8 years, 89% were male, acute coronary syndrome was reported in 78% of cases, and the most commonly treated artery was the left anterior descending (64%) with a type B2-C lesion (American Heart Association/American College of Cardiology) in 46%. Predilatation was performed in 91% and postdilatation in 55%. Although there were no complications during implantation, 1 patient had restenosis in the distal right coronary artery after 6 months (underexpansion of the 2.5 × 18mm Absorb-BVS), and was treated, ultimately, with a drug-eluting stent.
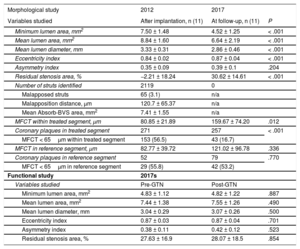
The functional impact of each lesion was evaluated at baseline with quantitative flow ratio, and after implantation a mean 0.59 ± 0.15 was obtained. The mean diameter obtained after implantation was 0.32mm greater than the reference diameter. Late lumen loss was 18.7 ± 21% after 5 years’ follow-up. After implantation, 119 struts were identified on OCT, but none were identified at follow-up (Figure 1). The main changes found in the lumen area, diameter, and morphology are presented in Table 1.
All panels show the OCT findings (implantation-follow-up). The white arrows indicate the radiopaque markers on the Absorb-BVS. The white crosses indicate plaques and calcium nodules. The red asterisks mark the lateral branches. I-L: severe restenosis of the Absorb-BVS (6 months), which was treated with a drug-eluting stent (2013) without compromising resorption (2017). OCT, optical coherence tomography.
OCT Findings in Patients Treated With Absorb-BVS After 5 Years of Follow-up
| Morphological study | 2012 | 2017 | |
|---|---|---|---|
| Variables studied | After implantation, n (11) | At follow-up, n (11) | P |
| Minimum lumen area, mm2 | 7.50 ± 1.48 | 4.52 ± 1.25 | < .001 |
| Mean lumen area, mm2 | 8.84 ± 1.60 | 6.64 ± 2.19 | < .001 |
| Mean lumen diameter, mm | 3.33 ± 0.31 | 2.86 ± 0.46 | < .001 |
| Eccentricity index | 0.84 ± 0.02 | 0.87 ± 0.04 | < .001 |
| Asymmetry index | 0.35 ± 0.09 | 0.39 ± 0.1 | .204 |
| Residual stenosis area, % | −2.21 ± 18.24 | 30.62 ± 14.61 | < .001 |
| Number of struts identified | 2119 | 0 | |
| Malapposed struts | 65 (3.1) | n/a | |
| Malapposition distance, μm | 120.7 ± 65.37 | n/a | |
| Mean Absorb-BVS area, mm2 | 7.41 ± 1.55 | n/a | |
| MFCT within treated segment, μm | 80.85 ± 21.89 | 159.67 ± 74.20 | .012 |
| Coronary plaques in treated segment | 271 | 257 | < .001 |
| MFCT < 65μm within treated segment | 153 (56.5) | 43 (16.7) | |
| MFCT in reference segment, μm | 82.77 ± 39.72 | 121.02 ± 96.78 | .336 |
| Coronary plaques in reference segment | 52 | 79 | .770 |
| MFCT < 65μm in reference segment | 29 (55.8) | 42 (53.2) | |
| Functional study | 2017s | ||
| Variables studied | Pre-GTN | Post-GTN | |
| Minimum lumen area, mm2 | 4.83 ± 1.12 | 4.82 ± 1.22 | .887 |
| Mean lumen area, mm2 | 7.44 ± 1.38 | 7.55 ± 1.26 | .490 |
| Mean lumen diameter, mm | 3.04 ± 0.29 | 3.07 ± 0.26 | .500 |
| Eccentricity index | 0.87 ± 0.03 | 0.87 ± 0.04 | .701 |
| Asymmetry index | 0.38 ± 0.11 | 0.42 ± 0.12 | .523 |
| Residual stenosis area, % | 27.63 ± 16.9 | 28.07 ± 18.5 | .854 |
GTN, glyceryl trinitrate; MFCT, minimum fibrous cap thickness; OCT, optical coherence tomography.
Values are presented as No. (%) or mean ± standard deviation.
The mean distance from the lumen edge of the markers to the endothelium (neointimal growth) was –134.7 ± 30.6μm after implantation and 213.5 ± 112.4μm at follow-up. Regarding atherosclerotic plaques, 271 were identified after implantation and 257 at 5 years; an increase in minimum fibrous cap thickness was recorded, from 80.85 ± 21.89μm to 159.67 ± 74.2μm (P = .012) and there was a reduction in the percentage of vulnerable plaques (< 65μm), from 56.5% to 16.7%, respectively.
Angiographic and OCT analysis revealed that jailed branches remained patent after 5 years with various types of neointimal bridges. The vasodilation test with glyceryl trinitrate did not produce significant changes in the variables analyzed on OCT (Table 1).
In summary, after 5 years of follow-up, we observed: a) complete resorption of the Absorb-BVS scaffolds, neointimal development (golden-tube appearance) and stabilization of vulnerable plaques; b) progressive changes in the lumen area and concentricity, and c) absence of vasodilatation after intracoronary administration of glyceryl trinitrate.
Although the morphological findings are comparable to those found in previous studies, the absence of coronary vasoreactivity differs from the results described in the Absorb trials,3,4 which may have clinical and prognostic effects.5 Thus, while the angiographic assessment of coronary vasomotion may have been subjective, quantification of the lumen area and diameter with OCT is an objective parameter. The authors acknowledge the small sample size and the consequent inability to detect complications such as late thrombosis or neoatherosclerosis. Furthermore, the lack of data on the intermediate phases of the resorption process means that we cannot rule out the possibility that changes occurred in the arterial wall or in the BVS, such as coronary evaginations or strut fracture.6 Finally, although the reduction in lumen area could be due to the sample size and the coronary vasoreactivity test was not compared with healthy coronary segments, this is the first study that reports structural and functional findings in patients in real clinical practice treated with Absorb-BVS after 5 years of follow-up and may represent the first step toward further studies in the area.
CONFLICTS OF INTERESTThe institution received an unconditional grant from Abbott Vascular to conduct the REPARA and REPARA-QALY studies.
.