Chest pain is a common presenting complaint in the emergency room. The guidelines recommend using different techniques for diagnosis of chest pain of possible coronary origin.1 The most important factor for choosing one technique over another is the competence of the local imaging laboratory. In Spain, the technique of choice is exercise stress echocardiography (ESE). This is a simple, inexpensive physiological test that is widely available. However, a certain percentage of ESE studies are inconclusive.
Our objective was to analyze the clinical determinants of inconclusive ESE in 452 consecutive patients who attended our emergency room for chest pain of probable coronary origin between January 2011 and December 2014. The symptom-limited Bruce protocol was used, although use of other protocols such as the modified Bruce protocol or the Naughton protocol was left to the discretion of the clinician, who also determined whether atropine or contrast echocardiography was used. ESE was considered inconclusive when the test was not positive for ischemia due to echocardiographic criteria and a heart rate (HR) of 85% the age-predicted maximum heart rate or a sufficient work load (6 MET for ages ≤ 75 years and 4 MET for ages above 57 years) was not reached or when contractility could not be assessed at the time of peak exercise.2 For selection of the predictive logistic regression model, the allsets command of STATA version 13.0 was used and the coefficients of the regression model were calculated by binary logistic regression (enter method).
In total, 132 ESE (29%) were inconclusive (106 [80%] because they did not reach the HR target, 36 [27%] because they did not reach a sufficient work load, and 11 [8%] because it was impossible to assess segmental contractility at peak exercise). The characteristics of the study population are shown in Table 1. The patients with inconclusive ESE had a longer hospital stay (3 [1-4] days vs 1 [1-2] days; P<.001) and a higher number of additional tests (27% vs 4%; P<.001). In 23 patients with inconclusive ESE, coronary anatomy was studied and significant coronary artery disease was detected in 8 of these (34%).
Baseline Characteristics of the Study Population by ESE Outcome
| Variables | Total population (n=452) | ESE result | ||
|---|---|---|---|---|
| Conclusive (n=320) | Inconclusive (n=132) | P | ||
| Age, y | 62±12 | 62±12 | 63±12 | .302 |
| Sex, male | 301 (67) | 207 (65) | 94 (71) | .181 |
| BMI | 29±4 | 29±5 | 30±4 | .187 |
| Hypertension | 327 (72) | 227 (71) | 100 (76) | .298 |
| Diabetes mellitus | 140 (31) | 94 (29) | 46 (35) | .252 |
| Dyslipidemia | 342 (76) | 239 (75) | 103 (78) | .451 |
| Current smoker | 112 (25) | 87 (27) | 25 (19) | .065 |
| Ischemic heart disease | 166 (38) | 100 (31) | 66 (50) | < .001 |
| Atrial fibrillation | 44 (10) | 18 (6) | 26 (20) | < .001 |
| Peripheral artery disease | 15 (3) | 10 (3) | 5 (4) | .774 |
| COPD | 26 (6) | 11 (3) | 15 (11) | .001 |
| Anxiety/depression | 118 (26) | 77 (24) | 41 (31) | .123 |
| LVEF< 50% | 28 (6) | 19 (6) | 9 (7) | .724 |
| SCA in baseline echocardiogram | 92 (20) | 56 (18) | 36 (28) | .017 |
| Left bundle branch block | 5 (1) | 3 (1) | 2 (2) | .632 |
| Creatinine, mg/dL | 0.9±0.3 | 0.9±0.3 | 1.0±0.4 | .002 |
| Hemoglobin, g/dL | 14.1±1.4 | 14.2±1.4 | 14.0±1.5 | .185 |
| Baseline HR, bpm | 80±16 | 81±16 | 76±10 | .008 |
| Baseline HR < 70 bpm | 133 (29) | 78 (24) | 55 (42) | < .001 |
| Baseline SBP, mmHg | 138±23 | 139±23 | 135±23 | .060 |
| Maximum HR, bpm | 132±21 | 138±17 | 118±22 | < .001 |
| Maximum SBP, mmHg | 156±25 | 159±25 | 149±25 | < .001 |
| Exercise duration, min | 7 [4-9] | 7 [5-9] | 6 [4-8] | < .001 |
| MET | 8±3 | 8±3 | 7±3 | < .001 |
| Use of atropine in ESE | 22 (5) | 14 (4) | 8 (6) | .443 |
| Use of contrast-enhanced echocardiography in ESE | 7 (2) | 6 (2) | 1 (1) | .384 |
| ESE protocol | .011 | |||
| Bruce | 416 (93) | 301 (95) | 115 (88) | |
| Modified Bruce/Naughton | 33 (7) | 17 (5) | 16 (12) | |
| ESE in less than 24 h | 273 (60) | 198 (62) | 75 (59) | .318 |
| Negative chronotropic agents | 200 (44) | 125 (39) | 75 (57) | .001 |
| Negative chronotropic agents and ESE in less than 24 h | 115 (26) | 71 (22) | 44 (33) | .014 |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; ESE, exercise stress echocardiography; HR, heart rate; LVEF, left ventricular ejection fraction; SBP, systolic blood pressure; SCA, segmental contractility abnormalities.
Values expressed as No. (%), mean±SD, or median [interquartile range].
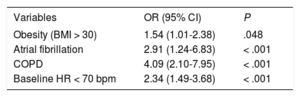
Table 2 shows the best-fit model for predicting inconclusive ESE, with C statistic=0.69 (95% confidence interval [CI], 0.63-0.74), Akaike information criterion index=485, Bayesian information criterion=509, and adequate calibration (Hosmer-Lemeshow test, P=.87). All factors included in the model for predicting inconclusive ESE were related to the criteria with an impact on the result. Obese patients and those with chronic obstructive pulmonary disease had a worse acoustic window and, along with patients with atrial fibrillation, usually had worse functional class. On the other hand, baseline HR<70 bpm increased the probability that the HR target for a conclusive test was not reached.
Factors Included in the Model for Predicting Inconclusive ESE
| Variables | OR (95% CI) | P |
|---|---|---|
| Obesity (BMI > 30) | 1.54 (1.01-2.38) | .048 |
| Atrial fibrillation | 2.91 (1.24-6.83) | < .001 |
| COPD | 4.09 (2.10-7.95) | < .001 |
| Baseline HR < 70 bpm | 2.34 (1.49-3.68) | < .001 |
BMI, body mass index; COPD, chronic obstructive pulmonary disease; ESE, exercise stress echocardiography; HR, heart rate; OR, odds ratio.
Our study showed a rate of inconclusive ESE of 29%. In the literature, the rate of inconclusive provocation tests varies widely according to the type of study, the patient profile, and the level of care in which testing occurs. The series of simple ergometry in chest pain units have a rate of inconclusive studies of 22% to 39%.3 Although ergometry includes electrocardiogram-dependent criteria, the main reason for an inconclusive study is not attaining target HR,4 a criterion shared with ESE and one that was also a main reason for inconclusive results in our study. A meta-analysis of ESE or a pharmacologically-based test showed a rate of inconclusive studies of 27%.5
The importance of inconclusive ESE should not be ignored. On the one hand, patients with inconclusive ESE have a higher risk of events than those with negative ESE (2.08% vs 0.77%).5 Furthermore, as was the case in our study, an inconclusive result implies the need for further studies to clarify the cause of symptoms, with the resulting increase in length of hospital stay and costs.3
The present study has important implications for decision-making in clinical practice, as it could help to identify patients with a high probability of inconclusive ESE. It is also the first study on this topic in patients who mostly belonged to the era of ultrasensitive troponin measurements. This makes it more relevant because the characteristics of patients with chest pain undergoing exercise stress tests at an early stage have changed after the introduction of these biomarkers. In view of our findings, we consider that certain measures should be assessed to improve the performance of the diagnostic process in patients with a high probability of inconclusive ESE. Such measures include delaying study of those who take agents with negative chronotropic effects, increasing the use of atropine or contrast-enhanced echocardiography, or selecting another modality of ischemia provocation test or cardiac computed tomography.6