To the Editor,
The destabilization of vulnerable atheroma plaques plays a major role in the genesis of acute coronary syndrome (ACS). Apparently, this is not a local reaction of a single atherosclerotic plaque: in the thrombogenic, proinflammatory context of ACS, vulnerability extends to lesions situated at other levels.1
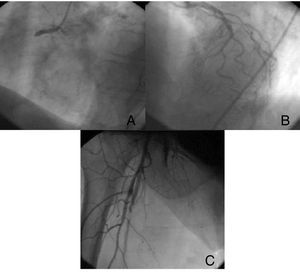
A 69-year-old woman with a past history of high blood pressure, type 2 diabetes mellitus, overweight (body mass index, 28), and tobacco use was referred for urgent percutaneous intervention, indicated for 2h of highly intense central chest pain with electrocardiograph changes compatible with extensive infarction and subepicardial lesion current in the inferior wall and leads V3-V6 (Figure 1). On arrival, the patient was hemodynamically stable and in complete atrioventricular block. She was administered 300mg acetylsalicylic acid (ASA) and 600mg clopidogrel when the intervention began. With the onset of chest pain, the patient simultaneously reported pain in the right lower extremity. Emergency echocardiography showed a left ventricle of normal size and general function, without intracavity thrombus, and right ventricular dysfunction. The patient was moved to the cardiac catheterization laboratory where the right coronary artery was catheterized and an acute thrombotic occlusion found in the proximal segment (Figure 2). She underwent angioplasty and drug-eluting stent implantation after intracoronary administration of abciximab. When the left coronary tree was catheterized, another thrombotic occlusion was found in the left anterior descending artery mid-segment (Figure 2), where simple angioplasty was performed due to the small diameter of the vessel. When catheterization was being completed, the patient reported right lower extremity pain. On examination, we found coldness in the extremity and an absence of distal pulses. Consequently, a contrast injection was administered via the right femoral artery introducer, revealing complete superficial right femoral branch occlusion (Figure 2). We therefore transferred the patient to the vascular surgery theater for urgent embolectomy with a Fogarty catheter.
Figure 1. Electrocardiogram with subepicardial lesion in inferior and anterior leads, and complete atrioventricular block.
Figure 2. Acute occlusion at the level of the proximal right coronary artery (A), anterior descending artery mid-segment (B), and superficial femoral artery (C).
No subsequent complications presented. Following clinical practice guidelines, the patient was administered a maintenance regimen of 100mg ASA and 75mg clopidogrel. Ten days later, platelet aggregation tests were requested. These revealed the patient's resistance to drugs, as her serum arachidonic acid and adenosine diphosphate concentrations were within the normal range (61% and 50%, respectively; normal, 50%-100%). Given the high thrombotic load of her symptoms, we decided to start treatment with 300mg ASA and 10mg prasugrel daily, after a 60mg load, and repeated the aggregation study at 5days. This showed arachidonic acid values were wholly suppressed and adenosine diphosphate had fallen to 26%. The patient progressed favorably, without complications, and at 4 months follow-up presented no new cardiovascular events.
In the literature, the series and cases described1, 2 seem to suggest the most logical strategy when treating ACS with two culprit arteries is complete revascularization in the acute phase. The most frequently described multiple coronary artery occlusions are found in the left anterior descending artery and right coronary artery (≤50% of cases),3 as in the patient described here. The peculiarity of our patient lies in the fact that the acute occlusion extended beyond coronary territory to the superficial femoral artery. Furthermore, we have shown that the patient presented drug resistance to conventional antiaggregation therapy. This resistance may share pathologic mechanisms with greater vulnerability to atherosclerotic plaques. New antiplatelet agents, like prasugrel, may well be more appropriate in these patients, in whom the choice of treatment benefits from a platelet aggregation study.4
Corresponding author: Semdoc@hotmail.com