To the Editor,
Complications derived from pulmonary artery catheter placement are about 3%-17%,1 from the most frequent and mild (carotid puncture, extrasystoles, etc) to the most severe (pulmonary artery rupture, pulmonary infarction, ventricular fibrillation, atrioventricular block, etc), and rare ones, such as intravascular catheter knotting, located preferentially in the right atrium (RA) or right ventricle (RV),1,2 this last being the most recent severe complication seen in our unit.
It occurred in a 68 year-old patient undergoing an implant of a mitral valve prosthesis due to a double mitral lesion and plasty of the tricuspid due to moderate reflux. Furthermore, in the preoperative ultrasound showed: dilatation of the left atrium, ventricles of normal size and contractility and pulmonary artery systolic pressure of 45 mmHg. After routine monitoring and anaesthesia induction, a high flow tri-lumen Edwards Lifesciences 9 Fr device was inserted in the internal right jugular vein, through which we placed a pulmonary artery 7.5 Fr catheter, guided by intracavitary pressure curves.
We were not able to see the course of the pulmonary artery in spite of introducing the catheter for more than 50 cm. After several collection attempts, we requested that the surgeon guide the catheter, who identified the knot, undid it and placed the catheter correctly. During reanimation we once more ran into the impossibility of following the pulmonary artery curve, added to the difficulty of balloon swelling. In view of the malfunctioning of the pulmonary catheter, we attempted to extract it and found this impossible.
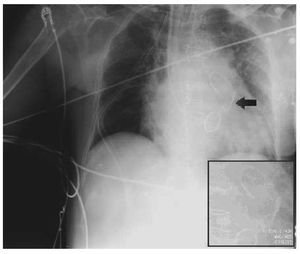
Radiographical identification of the knot in the pulmonary artery catheter in the RV (Figure 1) and persistent simultaneous bleeding through the pericardial drainages obliged us to perform a surgical revision. We performed haemostasis of the bleeding point at the level of the sternotomy and a "tobacco pouch" on the RA to extract the catheter (Figure 2). We found a complex knot (3´1.5cm) with 2 loops at 8 cm from the tip. Intracardial lesion was ruled out by postoperative ultrasound. The patient evolved satisfactorily and was discharged from the intensive care unit reanimation 48 hours later.
Figure 1. Posteroanterior x-ray that shows the knotting of the pulmonary artery catheter in the central area of the square.
Figure 2. Image of the pulmonary artery catheter sticking out of the incision in the right atrium.
Of the multiple factors that predispose to knotting and ravelling, several were present in our case: female, over 60 years of age, blind placement, heating and softening of the catheter (after several attempts), introduction of more than 50 cm, the fact that the balloon did not inflate after reaching the RA and the fact that the pulmonary artery catheter was not replaced after the first knot was detected (excessive handling increased the susceptibility of the catheter to form new knots).3 However, there were no other predisposing factors, such as dilatation of the right cavities or small caliber of the pulmonary artery catheter.
Classical signs made diagnosis possible: impossibility of wedging, resistance to inflation and difficulty to remove the catheter.4 Two reasons led us not to recognize the diagnosis: the fact that we thought the problem of the knot was resolved during surgery and the suspicion that the pulmonary artery catheter had been sutured after an intraoperative rupture of the RV reported in the surgical protocol.
Surgical removal, reserved in most cases for the extraction of large, multiple knots or those that involve cardiac structures, was applied in this case, coinciding with the need for surgical revision due to bleeding.
To prevent pulmonary artery catheter knotting and ravelling the following recommendations must be followed: use of catheters >7 Fr, injection of cold saline through the catheter before its placement to make it more rigid, inflation of the balloon in the RA, use of fluoroscopy or transesophageal ultrasound (TEUS), not to introduce more than 50 cm by the jugular or subclavian route or 70 cm by the femoral route, and not to introduce more than 15-20 cm after obtaining the RV curve.
To conclude, it must be highlighted that pulmonary artery catheter knotting is an infrequent complication,2,5 but that we must think of when we cannot obtain a pulmonary pressure curve, or run into difficulties when mobilising or inflating. We think that direct visualization by means of TEUS3 could help reduce this complications and achieve its early diagnosis, as well as avoiding blind manipulation that damages intracardial structures.