Keywords
INTRODUCTION
The endothelium is a monolayer of highly specialized cells that secrete various substances involved in maintaining vascular hemostasis.1
The term endothelial dysfunction (ED) refers to any alteration in the physiology of the endothelium which produces a decompensation in its regulatory functions and is considered the leading cause of development and progression of the atherosclerotic process.2 The state of endothelial function may reflect the propensity of an individual to develop clinical atherosclerotic disease.3 It is accepted that ED arises in response to the presence of coronary risk factors,4 especially to abnormal values of circulating lipids associated with the production of free radicals and the reduction in nitric oxide bioavailability.5-7 These risk factors not only cause dysfunction of the large vessels, but also of the coronary and peripheral microcirculation. In other words, ED represents a systemic disorder that affects the vasculature in general.8,9 Alterations in endothelium-dependent vasoreactivity are normally taken as being synonymous with ED.10 When vascular dilatation occurs in response to agents which stimulate the secretion of nitric oxide, this is known as endothelium-dependent flow-mediated vasodilation (FMD), whereas the response to direct vascular smooth muscle relaxants is called non-endothelial dependent vasodilatation.
This alteration in endothelial function is pharmacologically reversible and some studies have demonstrated that hypolipidemic treatment with statins improves ED in hypercholesterolemic patients with and without coronary disease.11-14 In recent years, various non-invasive techniques have been developed for the evaluation of coronary and peripheral endothelial function. Doppler ultrasonography is one of these techniques and basically consist in detecting alterations in arterial vasoreactivity under different physiological and pharmacological stimuli.15,16
The main aim of the present study was to non-invasively evaluate the short-term effect of atorvastatin treatment on the vasodilator response at the peripheral vascular and coronary microcirculation level in patients with dyslipidemia but without clear clinical atherosclerotic disease. The secondary aim was to evaluate the presence of possible predictive factors for a better response to treatment.
PATIENTS AND METHODS
Twenty-one dyslipidemic patients without clinical diagnosis or suspicion of atherosclerotic disease were included. The average age of the patients was 64.9±1 years with women making up 61.9% of the group. The baseline characteristics of the group are presented in Table 1.
Patients were defined as dyslipidemic when they had total cholesterol greater than 250 mg/dL or low-density lipoprotein cholesterol (LDL-C) greater than 160 mg/dL. The patients had not received hypolipidemic treatment in the 3 months prior to inclusion in the study. Patients were diagnosed as hypertensive if they had blood pressure greater than or equal to 140/90 mm Hg or if they had received antihypertensive treatment in the last 3 months. The American Diabetes Association 2002 criteria were used to identify diabetic patients (glycemia after fasting greater than or equal to 126 mg/dL on more than 2 measurements). The subject considered him/herself a smoker if he/she had consumed any quantity of tobacco in the last month.
The presence of atherosclerotic disease was ruled out through careful study of the case history and detailed physical exploration. Patients with doubtful symptomatology that could be related to clinical manifestations of atherosclerosis were excluded.
A baseline echocardiographic study was carried out with the ATL HDI 5000 system (Phillips, USA), which evaluated carotid intima-media thickness (IMT), peripheral endothelial function in the brachial artery and coronary reserve (CR) distal to the left anterior descending artery (LAD). A blood sample was also taken to analyze lipid profile and glycemia. After baseline evaluation, atorvastatin treatment was started at 20 mg/day for 3 months. No other treatment was changed during this period. A final evaluation was done at the end of treatment consisting of an analytical and echocardiographic study. The studies were conducted by the same echocardiographist. The protocol for the baseline and final studies was the same. This comprised a preparation period during which the patient fasted, and had not smoked or received his/her usual medication in the last 12 h. The temperature was kept constant in the room where the study took place. All the patients gave their written consent to participate in the study.
Analytic Study
Once the patient was placed in the dorsal decubitus position, a vein was cannulated and a full blood analysis done which included glycemia and lipid profile. After leaving the patient to rest for 10 min, baseline blood pressure was obtained and the following parameters were measured in the following order.
Measurement of Carotid IMT
Based on the classic studies by Pignoli et al17 and Salonen and Salonen,18 with the patient at rest and in dorsal decubitus position, the right common carotid artery was explored with a scanner using a 12-MHz linear transducer. Once the image was optimized, the bifurcation was located in the internal and external carotid artery and the echocardiograph zoom lens introduced. Carotid IMT was measured between the bifurcation and 1 cm proximal to it. To this end at least 5 points in the segment under study were measured and this was fully repeated on 2 occasions. A mean IMT value was thus obtained for the right common carotid artery. The procedure was repeated in the left carotid artery and the mean carotid value was obtained from the 2 values.
Measurement of Endothelial Function in the Brachial Artery
A protocol similar to the guidelines recently published for that purpose was followed.19 A 12-MHz linear transducer was used. After a 10-min rest period in the dorsal decubitus position, the brachial artery was located between 3 cm and 5 cm above the cubital fossa in the longitudinal plane, with gain and depth optimized and constant. Once an optimal image was acquired, the position was maintained with an external holding device attached to the arm of the patient. Baseline measurement (obtained from the mean of 2 measurements with at least 5 points measured in each of them) of arterial diameter and flow velocity were taken. Subsequently, the forearm was compressed at 300 mm Hg for 4 min. After loosening, reactive hyperemia (i.e. change in the flow speed) was assessed, and 1 min later the new diameter and arterial flow velocity were measured. The percentage change between the diameter after removing compression (D2) and baseline measurement (D1) was called EDV (or FMD)
EDV=([D2-D1]/D1])x100
Ten minutes later, when the artery returned to its baseline condition, 300 µg of nitroglycerin was administered and 4 min later the new dilatation of the artery observed. The percentage change between the diameter after nitroglycerin (D3) and baseline measurement (D1) was denominated endothelium-independent or nitroglycerin-dependent vasodilatation. Thus
EDVnitro=([D2-D1]/D1])x100
Measurement of Coronary Reserve With Dipyridamole
The CR study20 began immediately after the endothelial function study. The nitrites administered during the endothelial function study ensured that the epicardial arteries maintained maximum dilatation throughout the study. As the LAD section is not modified, the velocity quotient obtained can be extrapolated to the flow quotient, thus coming closer to actual CR.
After placing the patient in the left lateral decubitus position, the study commenced by deploying a 5-8 MHz probe using an apical 4-chamber view, such that the apex of both ventricles was visualized and the adipose triangular interventricular sulcus was observed which the LAD passes through. A pulse frequency of 2000 Hz was used, with the color area centered on the interventricular sulcus. The LAD appeared as a small red circular structure visible in diastole. In this view the flow was analyzed with pulsed Doppler ultrasound. We attempted to obtain the best alignment of the Doppler ultrasound with the LAD flow. We did not adjust the values of the pulsed Doppler ultrasound by the angle between the two axes. The pulsed Doppler ultrasound study was done during unforced post-exhalation apnea and peak velocity was recorded. For the CR study, LAD flow was determined in baseline conditions and after infusing 0.84 mg/kg dipyridamole over 6 min. The mean of 3 measurements was used. The quotient between the final and baseline peak diastolic velocity was taken to be the CR in the LAD. In all cases contrast agents were used (SonoVue®-Rovi) to homogenize the results.
The analytical study, IMT and FMD were determined in all patients. The evaluation of CR was not carried out in 6 patients. In 2 cases this was due to associated bronchial disease, in another 2 it was suspended due to symptoms of arterial hypotension and bradycardia after administration of nitrites and dipyridamole infusion, and in the remaining 2 cases the quality of the data/registries was not good enough.
Statistical Analysis
Baseline characteristics are presented as mean and standard deviation for the continuous variables, and as frequency and percentage for the discrete ones. Student's t test was used for paired data to assess the effect of atorvastatin on FMD and CR. Pearson correlations were carried out to study the relationship between continuous variables. Multiple linear regression models were constructed using the increase in CR and FMD as dependent variables. The independent variables in each model were selected from the clinical variables that could affect the FMD or CR (age, diabetes, tobacco use) and the significant variables from the bivariate analysis.
All the analyses were carried out with SPSS 10.0 software. A value of P<.05 was considered statistically significant.
RESULTS
Total cholesterol, LDL-C, and triglyceride levels were significantly reduced (27.1%, 36.5%, and 24.2%, respectively) after treatment with atorvastatin versus baseline, whereas high-density lipoprotein cholesterol (HDL-C) increased slightly (9.6%) (Table 2).
Intima-media thickness was not significantly modified by the end of follow-up (from 0.972 mm to 0.943 mm; P=.41) and good correlation was observed between the baseline and final studies (r=0.79; P=.001).
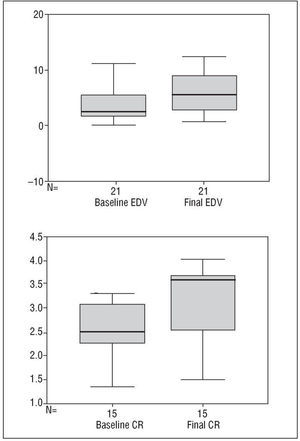
Flow-mediated dilation presented an increase of 43% versus baseline (from 4.3±4.4 to 6.2±3.8) which did not reach statistical significance (P=.07) (Figure). There was no correlation between the baseline and final FMD results (r=0.30; P=.18). Coronary reserve increased by 25% versus baseline at 3-month follow-up (from 2.5±.6 to 3.1±.8; P=.002), indicating good correlation between the 2 studies (r=0.53; P=.04) (Table 2).
Fig. 1. Coronary reserve (CR) and endothelium-dependent vasodilation (EDV) values before and after treatment.
Correlation analysis of baseline and final CR and FMD and their increases yielded the following results: baseline CR and FMD: r=0.11, P=.60; final CR and FMD: r=0.45, P=.09; increases in FMD and CR: r=-0.32, P=.23. A higher baseline FMD did not increase its value whereas it did in those patients with lower FMD. However, CR increased homogeneously, and in the final study the results of both studies tended to correlate.
In the bivariate analysis it was found that the increase in FMD was significantly and negatively correlated with age, baseline IMT and baseline LDL-C, such that the FMD improved more in the younger patients, with smaller IMT and lower baseline LDL-C. Flow-mediated dilation also increased in those with smaller FMD in the initial study. The increase in CR only showed negative correlation with LDL-C at the end of the treatment such that the lower the final LDL-C, the greater the increase in CR (Table 3).
Multiple linear regression showed that clinical variables such as diabetes and tobacco use did not modify the end result. Regarding the increase in FMD, baseline FMD was the only significant variable in the final model (B=-0.64; P=.002). Considering the increase in CR, final LDL-C was the only significant variable in the final model (B=-0.014; P=.002).
DISCUSSION
These results show that after 3 months of treatment with 20 mg/day atorvastatin in dyslipidemic patients without clinical atherosclerosis, in addition to the improvement in lipid profile, there was a significant improvement in CR and also an improvement in FMD, although the latter did not reach statistical significance. As was expected, the IMT value did not show any change after treatment. The fall in percentages of cholesterol and triglycerides, as well as the slight rise in HDL-C, were similar to those described in the literature.21
Intima-media thickness is an atherosclerosis marker and has been associated with the prevalence of cardiovascular disease.22,23 It is known that minimal reductions in IMT obtained with statins are important in cardiovascular prognosis.24 However, our study was not designed to evaluate the effect of statins on IMT. The measurement of IMT was used to non-invasively determine the degree of atherosclerotic disorder in patients.25,26
The evaluation of FMD in the brachial artery provides information on peripheral artery endothelial function,16 which has deteriorated in dyslipidemic patients who have other risk factors27 (an FMD>4.5% is considered to be normal).19 The mean value of the FMD in our series was below this value (4.3±4.4) and, although it increased by 43% after treatment with atorvastatin, it did not reach statistical significance. This increase would probably have been significant if the sample had been larger. The poor correlation between baseline FMD and after 3 months of treatment indicates that not all patients equally respond to treatment.
Hypercholesterolemia affects the vasodilator response to dipyridamole (CR) in high-risk patients with presumably normal epicardial coronary vessels28,29 due to the presence of microvascular abnormalities in the early stages of atherosclerosis.30 Hypercholesterolemia produces inflammation and microvascular dysfunction, and changes the antiinflammatory phenotype into a proinflammatory one.31 Coronary reserve in normal subjects is greater than 3 and drops in patients with epicardial injuries and in those with microvascular damage. A low CR of 2.5 was obtained in our patients. As coronary angiography was not carried out we cannot rule out the presence of epicardial lesions, but the characteristics of our sample suggest that the low value of CR would depend exclusively on microvascular damage. After 3 months of treatment a significant improvement in the evolution of CR was found of 25% versus baseline. The good correlation between the CR baseline values and those obtained after treatment indicate, in contrast to what occurs with FMD, that most patients respond homogeneously to the treatment.
The increase in FMD after 3 months of treatment with atorvastatin was greater in the younger patients, a smaller carotid artery IMT, and lower values of baseline LDL-C, i.e., in those with less baseline atherosclerotic load. It was also greater in patients with smaller baseline FMD, who have more damage to endothelial function. We have described an inverse correlation between the baseline LDL and maximum relaxation due to acetylcholine in the brachial artery of hypercholesterolemic patients.32
The increase in CR is not correlated with age, with IMT or with baseline lipid values. Coronary reserve increases more in those individuals in whom, after treatment, lower final values of LDL are obtained. Similar results were obtained in a study conducted with dyslipidemic patients with normal coronary angiography in whom coronary vessel resistance with intracoronary acetylcholine and intracoronary Doppler ultrasound after 6 months of treatment with pravastatin was evaluated.33 There is also evidence of improvement in the vasodilator response of the epicardial arteries to acetylcholine in relation to the LDL-C value obtained at the end of the treatment.34
The increase in CR was more significant and homogeneous than that of FMD. In order to interpret these different behaviors it would be necessary to take into account the structural differences between the 2 beds. The brachial artery is a main vessel and CR assesses the coronary microvasculature. Although both territories are resistant to atherosclerosis, the brachial artery presents intimal thickening as an adaptive response,35,36 whereas the microcirculation does not present obvious anatomic alterations. Furthermore, despite the association between ED in the brachial artery and the extent of coronary disease,37 some studies have demonstrated that a weak correlation exists between endothelial function of coronary and brachial regions,37,38 and that atherosclerosis would weaken this correlation.38 It has been suggested that there are variations between ED mechanisms in both vascular beds39 and differences in the magnitude of the vasodilator response in the microcirculation and main arteries.40 Finally, the different methods used to assess response to treatment have to be taken into account. At the brachial level, we measure the dilatation in a single artery, whereas when analyzing CR we take into account the increase in flow that is produced when dilating all the microvascular network dependent on the LAD. It is possible that a greater and more homogeneous response is obtained at the coronary level because the microvasculature barely has any structural damage that can limit the vasodilator response. In addition, CR evaluation used to analyze flow increase in the total microvascular network might be more sensitive to the changes than brachial FMD measurement.
In this study an improvement in CR dependent on LDL-C was not proven. This might depend on the simultaneous effects of statins on the vascular wall, taking into account that the microcirculation would be the main target organ of the antiinflammatory properties of statins.41
We emphasize the importance of being able to directly and non-invasively evaluate CR without having to extrapolate the results obtained in the brachial area, as various studies have suggested.
STUDY LIMITATIONS
The lack of coronary angiography made it impossible to confirm the absence of coronary lesions and to compare the measurement of CR with already standardized invasive methods. This was not considered necessary given the non-invasive character of our study.
Unlike FMD and IMT, CR was not determined in all patients. Patients with bronchial disease should be excluded and likewise those with atrioventricular conduction disorders. It is known that in approximately 10% of cases the quality of the data makes it impossible to draw conclusions, even when contrast agents are used. The present study had to be suspended in 2 patients because of hypotension and bradycardia due to the quantity of vasodilators to which they were subject (nitrites plus high-dose dipyridamole). One of the patients recovered following an infusion of saline and the other required atropine.
CONCLUSIONS
Short-term treatment with atorvastatin, in addition to having a beneficial and significant effect on lipid profile, is associated with an improvement in peripheral FMD and CR in the coronary microvasculature. The increase in CR after hypolipidemic treatment is more pronounced and homogeneous than the increase in FMD in the brachial artery and its improvement is related to the levels of cLDL attained at the end of treatment. By contrast, the short-term increase in peripheral FMD is less pronounced and more heterogeneous and improvement depends on factors that indicate less atherosclerotic involvement and more baseline endothelial injury. Note that both estimations can be monitored non-invasively in the echocardiography unit. The behavior of the 2 vascular beds after hypolipidemic treatment indicates that they cannot be considered equivalent, which suggests that caution should be exercised when extrapolating the results from the peripheral study to the coronary microvasculature.
Correspondence: Dr. J.L. Moya Mur.
Laboratorio de Ecocardiografía. Hospital Ramón y Cajal.
Ctra. de Colmenar Viejo, km 9,100. 28034 Madrid. España.
E-mail: jmoya.hrc@salud.madrid.org