Idiopathic fascicular ventricular tachycardia (VT) of the left ventricle is a rare type of VT. Unlike idiopathic right ventricular outflow tract VT, which usually occurs as either nonsustained or sustained monomorphic VT, idiopathic fascicular left VT usually occurs as sustained monomorphic VT. In Spain, idiopathic fascicular left VT ablation procedures comprise less than 10% of all idiopathic VT ablation procedures.1 Idiopathic fascicular left VT is commonly seen in verapamil-sensitive patients without structural heart disease. The mechanism of this tachycardia is reentry within the left-sided specialized conduction system. The most common form of these tachycardias affects the posterior fascicle and is therefore known as posterior fascicular VT.2 This form exhibits right bundle branch block morphology and superior axis. The forms that affect the anterior fascicle (anterior fascicular VT) and exhibit right bundle branch block morphology and right axis are less common. A very rare form affects a third, or septal, fascicle. This form is known as upper septal fascicular VT and has a narrow QRS morphology that is sometimes identical to that during sinus rhythm. In other cases, it exhibits incomplete right bundle branch block morphology and normal or right axis.3–5
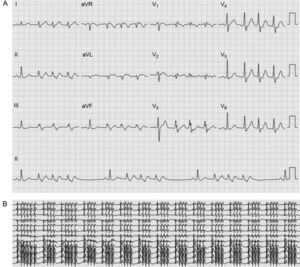
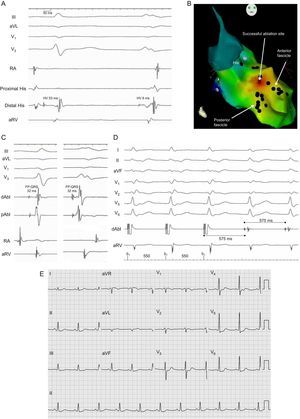
We report the case of a 48-year-old male smoker who was admitted for several days for recurrent palpitations in the neck associated with mild general discomfort. An initial electrocardiogram and telemetry on admission documented sinus rhythm alternating with continuous repetitive 3- to 5-beat bursts of tachycardia at 110 bpm with a QRS complex characteristic of incomplete right bundle branch block morphology without a shift of axis (Figure 1). There was no evidence of structural heart disease. Treatment was started with verapamil (80 mg/8 h), which reduced the number of bursts of tachycardia and the heart rate at which they occurred (100 bpm). However, the drug was discontinued after 2 days due to symptomatic hypotension and an electrophysiologic study was performed without drugs. A His-ventricular interval of 53ms in sinus rhythm was observed, with a constant His-ventricular-atrial sequence and a His-ventricular interval of 8ms during the repetitive nonsustained tachycardia complex (Figure 2A). The CARTO® 3 system was used to guide an irrigated-tip ablation catheter into the left ventricle using an atrial transseptal approach. Ventricular activation mapping of the Purkinje potentials recorded at QRS onset was performed, with visualization of the anterior and posterior fascicles of the left bundle branch (Figure 2B). At a site adjacent to the branching point of the anterior and posterior fascicles, the interval between the fascicular potential and QRS onset was virtually identical during sinus rhythm and tachycardia (32 ms) (Figure 2C), suggesting that this part of the conduction system was involved in the tachycardia.4 Furthermore, during activation mapping of this site, the tachycardia changed from repetitive nonsustained tachycardia to sustained tachycardia with occasional interruptions; the sustained tachycardia was reinduced by ventricular pacing. At this point in the procedure, it was possible to entrain the tachycardia. A difference was obtained between the post-pacing interval and tachycardia cycle length (0 ms), with an interval between the peak pacing level and the QRS onset equal to the interval between the fascicular potential and QRS onset. Nevertheless, there was a certain degree of fusion, which may have been due to capture from the adjacent ventricle (Figure 2D). The findings suggested that there was a reentry mechanism and that the ablation catheter was positioned at the site of the tachycardia circuit. Three radiofrequency ablations were performed at this site (Figure 2B) during sinus rhythm (up to 40W, 15 mL/h irrigation). Following this procedure, the tachycardia could not be reinduced, stable sinus rhythm without bursts of VT was maintained, and baseline QRS morphology remained unchanged (Figure 2E). After a follow-up of 3 months without drugs, the patient was asymptomatic without new episodes of tachycardia.
A: Intracavity recording and electrocardiographic leads of 1 (left) sinus beat and 1 tachycardia beat (right); B: Right anterior oblique view of the electroanatomic reconstruction and activation map of the fascicular potential created with the CARTO® 3 system; C: Intracavity recordings of the ablation catheter at the correct site during 1 sinus beat (left) and 1 tachycardia beat (right); D: Detail of tachycardia entrainment from the successful ablation site; E: 12-lead electrocardiogram after tachycardia ablation. dAbl, distal ablation; pAbl, proximal ablation; RA, right atrium; aRV, apex of the right ventricle; HV, His-ventricular; FP, fascicular potential.
Upper septal idiopathic fascicular VT is very rare. This tachycardia uses portions of the posterior fascicle as the anterograde limb (which can be considered as an orthodromic form of posterior fascicular VT5) and the septal fascicle as the retrograde limb, with simultaneous passive activation of the right bundle branch and anterior fascicle, which accounts for the relatively narrow QRS that can be very similar to baseline QRS. This form of tachycardia is often associated with a history of ablation of a typical posterior fascicular VT,2,3,5 although our patient had not undergone this procedure. To our knowledge, this case is unique in the literature, given the electrocardiographic presentation of repetitive nonsustained tachycardia.