The role of N-terminal pro-B-type natriuretic peptide (NT-proBNP) in the risk prediction of patients with systemic right ventricles (sRV) is not well defined. The aim of this study was to analyze the prognostic value of NT-proBNP in patients with an sRV.
MethodsThe prognostic value of NT-proBNP was assessed in 98 patients from the SERVE trial. We used an adjusted Cox proportional hazards model, survival analysis, and c-statistics. The composite primary outcome was the occurrence of clinically relevant arrhythmia, heart failure, or death. Correlations between baseline NT-proBNP values and biventricular volumes and function were assessed by adjusted linear regression models.
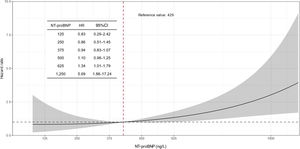
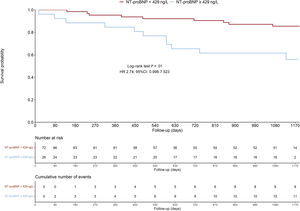
ResultsThe median age [interquartile range] at baseline was 39 [32-48] years and 32% were women. The median NT-proBNP was 238 [137-429] ng/L. Baseline NT-proBNP concentrations were significantly higher among the 20 (20%) patients developing the combined primary outcome compared with those who did not (816 [194-1094] vs 205 [122-357]; P=.003). In patients with NT-proBNP concentrations> 75th percentile (> 429 ng/L), we found an exponential increase in the sex- and age-adjusted hazard ratio for the primary outcome. The prognostic value of NT-proBNP was comparable to right ventricular ejection fraction and peak oxygen uptake on exercise testing (c-statistic: 0.71, 0.72, and 0.71, respectively).
ConclusionsIn patients with sRVs, NT-proBNP concentrations correlate with sRV volumes and function and may serve as a simple tool for predicting adverse outcomes.
Keywords
The population of adults with congenital heart disease and a systemic right ventricle (sRV) with biventricular circulation consists of patients with congenitally corrected transposition of the great arteries (ccTGA) and patients with dextro-transposition of the great arteries (d-TGA) after an atrial switch operation.1,2 Due to its embryological, morphological, and histological characteristics, the right ventricle is at increased risk for failure when exposed to systemic pressures. Thus, in adults with sRVs, ventricular dilatation and dysfunction are common, and there is a strong association between sRV dysfunction and cardiac complications (eg, arrhythmias and heart failure) and premature death.3–5
Natriuretic peptides such as B-type natriuretic peptide (BNP) and N-terminal pro–B-type natriuretic peptide (NT-proBNP) are quantitative markers of hemodynamic cardiac stress and heart failure (HF) that have gained increasing importance in the diagnosis of left ventricular dysfunction and HF among patients with acquired cardiovascular diseases.6,7 Moreover, the prognostic role of these biomarkers among patients with normal biventricular physiology is well-established.8–10 Pilot studies have suggested that NT-proBNP may also play an important role in risk prediction among patients with congenital heart disease (CHD).11,12 However, most of these studies included mixed cohorts of patients with CHD11,12 or focused solely on those with d-TGA after an atrial switch operation.13
The SERVE trial is a multicenter, double-blind, randomized, placebo-controlled clinical trial aiming to assess the effects of tadalafil on sRV size and function, exercise capacity, and neurohormonal activation over time.14,15 The present study is a substudy of the SERVE trial. We aimed to assess the determinants and the prognostic value of NT-proBNP in patients with an sRV from the SERVE trial.
METHODSEthics approvalThis study used data from the SERVE trial. The responsible investigator at each site ensured that approval from an appropriately constituted Competent Ethics Committee was sought for the clinical study. All changes in the research activity (including the case of planned or premature study end), all unanticipated problems involving risks to humans and the final report were reported to the ethics committee.
The study was carried out in accordance with the protocol and with the principles outlined in the current version of the Declaration of Helsinki. The ethics committee and regulatory authorities received annual safety and interim reports and were informed about study stop/end in agreement with local requirements.
Study populationThe study population consisted of participants from the SERVE trial with valid baseline NT-proBNP values. The detailed methodology of the study has already been published.14,15 In short, the SERVE trial is a double-blind, randomized, placebo-controlled, multicenter trial comparing placebo vs tadalafil in a 1:1 ratio. All participants started on tadalafil 20mg or placebo once daily, or both. At baseline, a clinical examination, a 12-lead electrocardiogram, and an echocardiogram were performed. Neurohormonal activation, detailed cardiac anatomy, biventricular volumes, and function, as well as exercise capacity and cardiopulmonary fitness were assessed by means of blood tests, cardiac magnetic resonance (CMR) or coronary multidetector computed tomography (CMDCT) if CMR was contraindicated, and a cardiopulmonary exercise test, respectively. These examinations were repeated after 1 year and at the end of the study follow-up 3 years later. For the purpose of this analysis, data on 98 patients with no missing NT-proBNP values at baseline from a total of 100 were analyzed.
Assessment of neurohumoral activationConcentrations of NT-proBNP (ng/L) were analyzed in a core lab with expertise in biomarker analysis: the Cardiovascular Research Institute Basel (CRIB) in Basel, Switzerland. An electrochemiluminescence immunoassay (Elecsys, Roche Diagnostics, Switzerland) was used. Specific patient sets with plastic tubes and barcodes corresponding to the individual patient numbers and time points in the study were used. Samples were collected locally, followed by centrifugation, aliquoting, and initial storage at−80°C at the participating centers. Routine sample collection at the local study sites and refrigerated transportation to the dedicated biobank at the CRIB were provided by the core lab. The data obtained from the analysis were then centrally entered into the electronic database of the SERVE trial.
Primary and secondary outcomes of the current studyThe combined primary outcome of the current study (from now on also referred to as cardiac complications) was defined as the occurrence of either clinically relevant arrhythmias (requiring hospitalization and/or therapeutic intervention), hospitalization for HF, or all-cause death.
Secondary outcomes investigated the pathophysiological determinants of NT-proBNP in patients with an sRV by assessing the correlations of this biomarker with baseline biventricular end-diastolic and end-systolic volumes, stroke volumes, and ejection fraction assessed by CMR/CMDCT.
Statistical analysisContinuous variables are presented as medians (interquartile range [IQR]), and categorical variables as counts (percentages). Baseline characteristics were stratified by NT-proBNP quartiles and compared using the Kruskal-Wallis test for continuous variables and the chi-square or Fisher exact test for categorical variables, as appropriate. Confidence intervals were computed as recommended.16
Friedman 2-way ANOVA was used for the comparison of dependent samples. Multivariable linear regression models (age-, sex-, and creatinine-adjusted) were fitted for each baseline CMR/CMDCT variable related to biventricular volumes and function. To avoid dichotomizing continuous variables and imposing linearity, continuous variables were modeled using restricted cubic splines. Three spline knots were placed at 0.1, 0.5, and 0.9 percentiles of each variable marginal distribution, following Harrell's recommendations.17 Linear regression assumptions were checked using diagnostic plots. Consequently, the dependent variable (NT-proBNP) in each model was log-transformed to satisfy the assumption of homoscedasticity. To avoid dichotomizing our main variable of interest (NT-proBNP), another Cox proportional hazards model corrected for age and sex was fitted. NT-proBNP was then modeled with a restricted cubic spline function (3 knots) to take possible nonlinearity into consideration and to treat the main variable of our study continuously. Because NT-proBNP was modeled with a restricted cubic spline, we expressed its hazard ratio (HR) using the 75th percentile of our NT-proBNP values (429 ng/L) as the reference value. We calculated the HR of several levels of NT-proBNP compared with this specific reference value. The proportional hazard assumption was tested by means of the Schoenfeld residuals. The assumption was not violated (overall P=.73; figure 1 of the supplementary data). In addition, to investigate the association of clinically relevant parameters with the occurrence of the primary outcome, an age- and sex-corrected Cox proportional hazards model was fitted for each of the following variables: New York Heart Association (NYHA) functional class> I, NT-proBNP, predicted peak oxygen uptake (predicted peak VO2 [%]), and right ventricular ejection fraction (RVEF), as %. To test the added value of NT-proBNP on top of RVEF and peak VO2, a sequential modeling approach starting with RVEF, adding peak VO2, and ending with NT-proBNP was performed. Due to the limited sample size, we were unable to adjust the base model for more prior information.
Survival analysis for the occurrence of the combined primary outcome of patients with NT-proBNP values lower vs higher than the cutoff value (> 429ng/L) was assessed using the Kaplan-Meier estimator. If a patient experienced multiple events, event-free survival time was calculated from the date of inclusion until the occurrence of the first event. The statistical significance for the difference between groups was assessed by means of the log-rank test. The individual prognostic accuracy of NT-proBNP and those of other established markers for predicting the primary outcome was assessed by means of the concordance statistic (c-statistic). To compare the prognostic value of NT-proBNP, we built a model adjusted for age and sex and compared the c-statistic with adjusted models for RVEF and predicted peak VO2.
All hypothesis testing was 2-tailed, and P values <.05 were considered statistically significant. There was 1 missing value for the variable “predicted peak VO2 (%)”. This patient was excluded from the corresponding analysis. Data analysis was performed in R, version 4.1.3 (R Foundation for Statistical Computing, Austria).
RESULTSBaseline characteristics stratified by NT-proBNP quartiles are depicted in table 1. The median age at baseline was 39 [32-48] years and 32% of the patients were female. There was no significant difference in NT-proBNP concentrations between men and women (220 [125-426] vs 259 [154-456]; P=.504). The median [IQR] of NT-proBNP was 238 [137-429] ng/L. Older patients had higher NT-proBNP concentrations. In 24 patients (24%), the NT-proBNP concentration was above the chosen cutoff value of> 429 ng/L (fourth quartile). Eighty-two (84%) patients were in functional NYHA class I and had lower NT-proBNP levels compared with patients in functional class II or III. The 3 patients with permanent atrial fibrillation/flutter were in the highest NT-proBNP quartile.
Baseline characteristics of the study population
| Variable [IQR] | OverallNT-proBNP | Quartile 1[56-136] | Quartile 2[137-237.5] | Quartile 3[237.6-429] | Quartile 4[430-5778] | P |
|---|---|---|---|---|---|---|
| No. | 98 | 25 | 24 | 25 | 24 | |
| Age, y | 39 [32,48] | 32 [30-40] | 36 [31-38] | 41 [37-49] | 52 [41-54] | <.001 |
| Female sex | 31 (32) | 7 (28) | 7 (29) | 9 (36) | 8 (33) | .946 |
| Treatment with tadalafil | 50 (51.0) | 15 (60.0) | 9 (37.5) | 12 (48.0) | 14 (58.3) | .379 |
| Weight, kg | 78.5 [70-86] | 80 [72-88] | 75 [70-86] | 75 [63-85] | 82 [72-85] | .573 |
| BMI | 25.5 [23-28] | 26 [25-28] | 24 [22.0-26] | 26 [23-28] | 27 [25-28] | .143 |
| PM/ICD implantation | 20 (20) | 2 (8) | 4 (17) | 7 (28) | 7 (29) | .189 |
| Cardiac anatomy | .149 | |||||
| ccTGA | 25 (26) | 7 (28) | 3 (13) | 6 (24) | 9 (38) | |
| d-TGA and Mustard | 21 (21) | 3 (12) | 4 (17) | 9 (36) | 5 (21) | |
| d-TGA and Senning | 52 (53) | 15 (60) | 17 (71) | 10 (40) | 10 (42) | |
| Additional lesion | .334 | |||||
| None | 58 (59) | 15 (60) | 15 (62) | 16 (64) | 12 (50) | |
| VSD | 11 (11) | 3 (12) | 3 (13) | 1 (4) | 4 (17) | |
| Pulmonary stenosis | 8 (8.2) | 4 (16) | 2 (8) | 0 (0) | 2 (8) | |
| VSD and pulmonary stenosis | 10 (10) | 1 (4) | 1 (4) | 3 (12) | 5 (21) | |
| Other | 11 (11) | 2 (8) | 3 (13) | 5 (20) | 1 (4) | |
| NYHA classification | .001 | |||||
| I | 82 (84) | 23 (92) | 23 (96) | 23 (92) | 13 (54) | |
| II | 13 (13) | 1 (4) | 1 (4) | 2 (8) | 9 (38) | |
| III | 3 (3) | 1 (4) | 0 (0) | 0 (0) | 2 (8) | |
| Rhythm (ECG) | .145 | |||||
| Junctional | 12 (12.2) | 1 (4.0) | 2 (8.3) | 6 (24.0) | 3 (12.5) | |
| Sinus rhythm | 66 (67.3) | 21 (84.0) | 19 (79.2) | 13 (52.0) | 13 (54.2) | |
| Atrial flutter | 2 (2.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (8.3) | |
| Atrial fibrillation | 1 (1.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (4.2) | |
| Pacemaker | 15 (15.3) | 2 (8.0) | 3 (12.5) | 5 (20.0) | 5 (20.8) | |
| Other | 2 (2.0) | 1 (4.0) | 0 (0.0) | 1 (4.0) | 0 (0.0) | |
| TR severity | .584 | |||||
| None | 8 (8.8) | 3 (12.5) | 1 (4.5) | 2 (9.5) | 2 (8.3) | |
| Mild | 52 (57.1) | 14 (58.3) | 15 (68.2) | 13 (61.9) | 10 (41.7) | |
| Moderate | 27 (29.7) | 7 (29.2) | 6 (27.3) | 5 (23.8) | 9 (37.5) | |
| Severe | 4 (4.4) | 0 (0.0) | 0 (0.0) | 1 (4.8) | 3 (12.5) | |
| CMR/CMDCTa | ||||||
| Indexed RVESV, mL | 63.9 [51.7-82.9] | 60.2 [49.4-68.9] | 61.9 [49.5-69.1] | 70.1 [53.1-89.5] | 84.5 [55.8-108.6] | .012 |
| Indexed RVEDV, mL | 121.4 [103.6-140.1] | 110.7 [98.4-122.8] | 117.9 [101.0-128.2] | 128.8 [105.6-157.5] | 128.2 [113.6-161.3] | .022 |
| Indexed RVSV, mL | 53.9 [47.7-62.1] | 52.8 [46.9-56.0] | 52.9 [48.5-58.3] | 63.2 [51.8-69.6] | 50.8 [43.6-61.7] | .016 |
| RVEF, % | 45.6 [39.5-50.5] | 46.1 [43.1-50.6] | 47.5 [44.9-50.6] | 46.0 [41.4-52.8] | 35.3 [30.3-46.9] | .001 |
| Indexed LVESV, mL | 26.8 [21.3-38.2] | 25.0 [20.9-33.5] | 28.2 [20.8-33.8] | 31.7 [23.4-41.6] | 30.8 [22.2-39.4] | .377 |
| Indexed LVEDV, mL | 77.5 [62.8-88.5] | 77.6 [62.4-84.7] | 74.4 [64.6-84.5] | 83.9 [72.2-97.8] | 72.2 [62.5-90.7] | .375 |
| Indexed LVSV, mL | 48.1 [41.1-55.5] | 50.2 [43.5-55.8] | 45.8 [40.9-51.5] | 51.9 [43.9-56.9] | 42.5 [38.6-51.6] | .185 |
| LVEF, % | 63.5 [58.4-67.5] | 66.3 [60.2-67.8] | 64.2 [61.0-68.7] | 63.0 [56.1-67.4] | 62.2 [55.4-65.3] | .353 |
| CPETb | ||||||
| Peak VO2, mL/min/kg | 25.3 [19.1-29.2] | 29.1 [21.6-31.3] | 27.0 [22.9-29.8] | 25.1 [19.0-28.9] | 18.3 [14.3-22.8] | <.001 |
| Predicted peak VO2, % | 76.0 [67.0-86.0] | 81.0 [74.0-92.0] | 77.0 [69.8-86.5] | 82.0 [67.8-92.5] | 67.0 [56.0-77.0] | .006 |
| Laboratory parameters | ||||||
| Creatinine, μmol/L | 82 [73-93] | 86 [81-96] | 79 [74-85] | 75 [71-78] | 90 [79-99] | .007 |
| Hs-cTnT, ng/L | 7 [4-11] | 5 [3-7] | 6 [4-9] | 7 [5-9] | 14 [9-17] | <.001 |
BMI, body mass index (in kg/m2); ccTGA, congenitally corrected transposition of the great artery; CMR, cardiac magnetic resonance; d-TGA, dextro-transposition of the great arteries; hs-cTnT, high-sensitivity cardiac troponin T; ECG, electrocardiogram; LVEDV, left ventricular end-diastolic volume; LVEF, left ventricular ejection fraction; NT pro-BNP, N-terminal pro–B-type natriuretic peptide; NYHA, New York Heart Association; RVEDV, right ventricular end-diastolic volume; RVEF, right ventricular ejection fraction; VO2=oxygen uptake.
The data are expressed as median [interquartile range] or No. (%).
There were 24 primary outcome events in 20 (20%) patients. Specifically, there were 2 deaths, 5 hospitalizations due to HF, and 17 clinically relevant arrhythmias (15 supraventricular arrhythmias and 2 ventricular arrhythmias). The occurrence of the combined primary outcome increased significantly within the fourth quartile compared with quartiles 1-3 (for each of quartile 1-3: 3 events (12%), compared with 11 events in quartile 4 (46%); P=.012). Levels of NT-proBNP were significantly higher among patients meeting the combined primary outcome (816 [194-1094] vs 205 [122-357]; P=.003). The median [IQR] of NT-proBNP levels for arrhythmia and HF were 322 [190-1095] and 1202 [928-3980], respectively. The 2 (male) patients who died had NT-proBNP levels of 773 and 932 ng/L, respectively. The occurrence of the primary outcome did not significantly differ among cardiac anatomy groups (6 [24%], 5 [22%], and 9 [17%]; P=.768 for ccTGA, d-TGA after Mustard operation, and d-TGA after Senning operation).
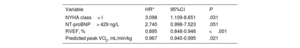
HRs with 95% confidence intervals (95%CI) for other established risk factors for increased risk of cardiovascular events during the 36-month follow-up are shown in table 2. The association between NT-proBNP levels and the risk of 36-month complications (primary outcome) is depicted in figure 1. A significant nonlinear dose-response association is shown. HRs (95%CI in gray) of NT-proBNP compared with the cutoff value of 429 ng/L for the occurrence of the primary outcome are also outlined in figure 1. Event-free survival (median [IQR] follow-up duration=37 [36-37]) was significantly higher in patients with NT-proBNP values below the cutoff value (429 ng/L) when compared with patients above this level (figure 2). The unadjusted c-statistic for NT-proBNP and other established markers for poor prognosis are depicted in table 3. There was no difference in the prognostic performance of NT-proBNP, RVEF, NYHA class> I, and peak VO2 (predicted) for the occurrence of the primary outcome (table 3). When comparing Model I to Model II and Model III (table 4), there was no significant difference in their prognostic value (P=.815 and .935, respectively). The base model with RVEF yielded a c-statistic of 0.69 (95%CI, 0.56-0.82). Incorporating peak VO2 into the model resulted in a c-statistic of 0.7 (95%CI, 0.56-0.84). Finally, the addition of NT-proBNP to the model comprising RVEF and peak VO2 increased the c-statistic to 0.71 (95%CI, 0.57-0.85). These results are depicted in table 5.
Hazard ratios for the occurrence of the primary outcome
| Variable | HR* | 95%CI | P |
|---|---|---|---|
| NYHA class> I | 3.098 | 1.109-8.651 | .031 |
| NT-proBNP> 429 ng/L | 2.740 | 0.998-7.523 | .051 |
| RVEF, % | 0.895 | 0.848-0.946 | <.001 |
| Predicted peak VO2, mL/min/kg | 0.967 | 0.940-0.995 | .021 |
95%CI, 95% confidence interval; HR, hazard ratio; NT pro-BNP, N-terminal pro–B-type natriuretic peptide; NYHA, New York Heart Association; predicted peak VO2, maximal oxygen uptake; RVEF, right ventricular ejection fraction.
NT-proBNP and the occurrence of the primary outcome. This dose-response plot shows the association between NT-proBNP levels at baseline and the risk of complications at 36 months. We calculated age- and sex-adjusted hazard ratios (95%CI) for several levels of NT-proBNP and compared them to our reference value of 429ng/L. 95%CI, 95% confidence interval; HR, hazard ratio; NT pro-BNP, N-terminal pro–B-type natriuretic peptide.
Survival analysis stratified by a NT-proBNP level of 429ng/L. Kaplan-Meier curve showing the occurrence of the combined primary outcome in patients with NT-proBNP values above and below the median. There was a significantly higher occurrence in patients with levels at or above 429ng/L. 95%CI, 95% confidence interval; HR, hazard ratio; NT pro-BNP, N-terminal pro–B-type natriuretic peptide.
Prognostic performance of individual variables
| Variable | c-statistic | 95%CI |
|---|---|---|
| NYHA class> I | 0.64 | 0.53-0.74 |
| NT-proBNP, ng/L | 0.70 | 0.57-0.83 |
| RVEF, % | 0.69 | 0.56-0.82 |
| Predicted peak VO2, mL/min/kg | 0.65 | 0.53-0.77 |
95%CI, 95% confidence interval; NT pro-BNP, N-terminal pro–B-type natriuretic peptide; NYHA, New York Heart Association; peak VO2, maximal predicted oxygen uptake; RVEF, right ventricular ejection fraction.
Prognostic performance of different variables adjusted for age and sex
| Model | c-statistic | 95%CI |
|---|---|---|
| Model INT-proBNP adjusted for age and sex | 0.71 | 0.58-0.83 |
| Model IIRV EF adjusted for age and sex | 0.72 | 0.59-0.84 |
| Model IIIPredicted peak VO2 adjusted for age and sex | 0.71 | 0.59- 0.83 |
95%CI, 95% confidence interval; NYHA, New York Heart Association; peak VO2, maximal predicted oxygen uptake; RVEF, right ventricular ejection fraction.
Added prognostic performance of different variables
| Variables | c-statistic | 95%CI |
|---|---|---|
| RVEF | 0.69 | 0.56-0.82 |
| RVEF + predicted peak VO2 | 0.70 | 0.56-0.84 |
| RVEF + predicted peak VO2 + NT-proBNP | 0.71 | 0.57-0.85 |
95%CI, 95% confidence interval; NYHA, New York Heart Association; peak VO2, maximal predicted oxygen uptake; RVEF, right ventricular ejection fraction.
In a sensitivity analysis assuming linearity for the association between NT-proBNP and the outcome and for the association between NT-proBNP and the magnetic resonance imaging parameters, the results were comparable (figure 2 and 3 of the supplementary data).
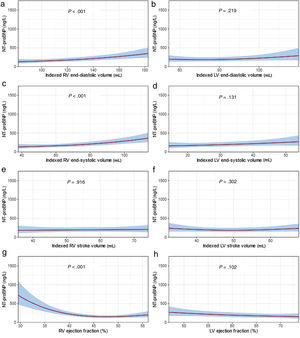
Determinants of NT-proBNP concentrationsMeasurements of biventricular volumes and function are shown in table 1. Systemic RV end-systolic and end-diastolic volumes, ejection fraction and stroke volume were significantly associated with NT-proBNP (P <.03 for all correlations).
A graphic representation of the multivariable linear regression models for the correlation of NT-proBNP levels with CMR- or CDMCT-derived biventricular indexed volumes and function are depicted in figure 3. A statistically significant positive correlation between NT-proBNP levels and right ventricular end-systolic and end-diastolic volume index was observed (coefficient of determination: +0.481; P <.001, and +0.427; P <.001 respectively). There was a statistically significant negative correlation between NT-proBNP levels and RVEF (coefficient of determination: −0.561; P <.001). For the remaining parameters, no statistically significant correlation with NT-proBNP was observed.
Correlation of NT-proBNP levels with variables regarding the right ventricular size and function. Multivariable linear regression models (age-, sex-, and creatinine adjusted) were fitted for baseline biventricular end-diastolic and end-systolic volumes, stroke volumes and ejection fraction assessed by either cardiac magnetic resonance or coronary multidetector computed tomography. There was a significant association between NT-proBNP levels and right ventricular volumes and function. LV, left ventricular; NT pro-BNP, N-terminal pro–B-type natriuretic peptide; RV, right ventricular.
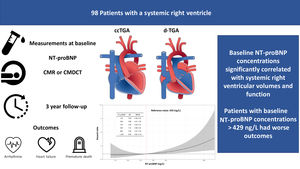
To our knowledge, this is the first prospective study investigating the prognostic value and determinants of NT-proBNP in a well-defined population of patients with an sRV (SERVE trial). Individuals meeting the primary outcome of adverse cardiovascular events (a composite endpoint of death, hospitalization for HF, and/or occurrence of clinically relevant arrhythmia) had significantly higher baseline NT-proBNP levels than those who remained event-free during follow-up. An NT-proBNP level> 429 ng/L seems to be a practical cutoff level indicating an increased risk of adverse events during mid-term follow-up. The prognostic accuracy of NT-proBNP was comparable to that of RVEF and predicted peak VO2. By comparing the prognostic value of NT-proBNP with RVEF and peak VO2 in separate models, the study aimed to assess whether NT-proBNP could offer comparable prognostic performance to magnetic resonance imaging analysis or exercise stress tests, which are more resource-intensive, not widely accessible, and require specialized trained personnel. The similar prognostic performance underscores the potential value of NT-proBNP as a widely accessible prognostic biomarker. While the addition of NT-proBNP on top of RVEF and peak VO2 increased prognostic discrimination, the improvement was modest. However, due to the wide confidence intervals (resulting from the small sample size), it is difficult to draw conclusions from this sequential approach. Higher NT-proBNP levels were associated with higher right ventricular end-systolic and end-diastolic volume index and lower RVEF as measured by CMR or CMDCT. Figure 4 depicts the findings as a central illustration.
Central illustration. Analyzing NT-proBNP in patients with a systemic right ventricle. ccTGA, congenitally corrected transposition of the great arteries; d-TGA, dextro-transposition of the great arteries; 95%CI, 95% confidence interval; CMDCT, coronary multidetector computed tomography; CMR, cardiac magnetic resonance; HR, hazard ratio; NT pro-BNP, N-terminal pro–B-type natriuretic peptide.
Previous studies analyzing the prognostic impact of NT-proBNP were either performed in heterogeneous cohorts of patients with adult congenital heart disease or were retrospective in nature.
Popelovà et al.11 investigated the prognostic value of NT-proBNP in 646 adults with various congenital heart lesions. These authors found a significant correlation between NT-proBNP and all-cause mortality. Of these, 84 patients (13%) had transposition of the great arteries after Mustard or Senning operation and 22 patients (3%) had ccTGA.11 Baggen et al.12 also examined the prognostic value of serial NT-proBNP measurements in 602 ACHD patients, including 65 (11%) patients with d-TGA after atrial switch operation and 20 (3%) patients with ccTGA. They found an association between elevated NT-proBNP measurements and a combined endpoint of death, HF, hospital admission, arrhythmia, thromboembolic event, and cardiac intervention. However, neither study reported lesion-specific outcomes. A retrospective study of 87 patients after atrial switch operation found NT-proBNP to be the most reliable prognostic marker for mortality.18 Another retrospective cohort study of 89 TGA patients with prior atrial switch operation showed that BNP had a high predictive value for distinguishing patients with and without critical cardiac events.13
The strength of our analysis is that measures of neurohormonal activation, ventricular volumes and function derived from CMR and CMDCT, as well as determinants of exercise capacity, were obtained from dedicated core labs, used in the SERVE trial.14,15 While our analysis supports findings from previous studies regarding the prognostic value of NT-proBNP levels, the determined NT-proBNP cutoff> 429 ng/L derived from our data may serve as a clinical risk marker, although this should be confirmed in larger patient cohorts. Additionally, our data strongly support the prognostic importance of NT-proBNP levels, which are comparable to RVEF and peak oxygen uptake on exercise testing, and may therefore help in tailoring the frequency and type of follow-up studies in clinically stable patients.
Clinical relevance of our findingsThe role of NT-proBNP in patients with a systemic left ventricle has been thoroughly investigated, and its importance in the evaluation and management of these patients, for example in the setting of the emergency department, is undisputed.19
While the importance of NT-proBNP in predicting adverse events in ACHD is mentioned in the current guidelines, there is no specific recommendation for patients with an sRV.20 Our study showed that NT-proBNP may help to discriminate patients who are at risk of clinically relevant arrhythmia, HF, or death. Values of NT-proBNP> 429 ng/L may now be seen as a screening tool for closer follow-up or even as a turning point to consider starting HF medication in asymptomatic patients with an sRV. The correlations of NT-proBNP with sRV volumes and function points toward a comparable pathophysiological pathway to that seen in subaortic left ventricles. Furthermore, the prognostic accuracy of NT-proBNP alone was comparable to that of models using RVEF or predicted peak VO2. Thus, this widely available and inexpensive biomarker may be seen as an alternative to other more costly, time-consuming, and less universally available tools.
LimitationsOnly 24 cardiac events occurred during our 3-year follow-up period. Of these, only 2 were deaths. Furthermore, the overall number of patients was low. Given the relatively small sample size of the cohort, the suggested cutpoint for NT-proBNP should be interpreted with caution. Studies with longer follow-ups and a larger number of patients are needed to assess the prognostic value of NT-proBNP with regard to mortality and to validate the cutpoint and assess its extrapolation and robustness. For the same reason, we were only able to adjust for some selected variables, and the effect of other variables on NT-proBNP levels and their prognostic value is still unknown. Additionally, Kaplan-Meier curves should be interpreted with caution due to potential residual confounding.
CONCLUSIONSPatients with higher concentrations of NT-proBNP were at a significantly higher risk of adverse events. The accuracy of NT-proBNP in predicting death, hospitalization for HF, and/or clinically relevant arrhythmia was comparable to that of the RVEF and predicted peak VO2. N-terminal natriuretic peptide significantly correlated with right ventricular volumes and function measured by CMR. NT-proBNP may be a reliable and widely available diagnostic tool for the risk stratification of patients with sRV. Our findings need to be validated with further studies including longer follow-up duration time.
- –
NT-proBNP has gained increasing importance in the diagnosis of left ventricular dysfunction and HF among patients with acquired cardiovascular diseases.
- –
However, there is scarce evidence on the importance of NT-proBNP in risk prediction among patients with CHD and most published studies included mixed cohorts of patients with CHD or focused solely on patients with d-TGA after atrial switch operation.
- –
This study shows that NT-proBNP may help discriminate patients with an sRV who are at risk for clinically relevant arrhythmia, HF, or death.
- –
Values of NT-proBNP> 429 ng/L may now be seen as a screening tool for closer follow-up or even as an indication to consider starting HF medication in asymptomatic patients with an sRV.
- –
The prognostic accuracy of NT-proBNP alone was comparable to that of models using RVEF or predicted peak VO2.
The SERVE trial is funded by the Swiss National Foundations (Schweizerischer Nationalfonds zur Förderung der wissenschaftlichen Forschung, 31IC30_166855).
ETHICAL CONSIDERATIONSThis work was carried out in accordance with the protocol and the principles enunciated in the current version of the Declaration of Helsinki. All patients provided written informed consent. We did not specifically take possible sex/gender biases into consideration, as the effect/level of the biomarker should not be influenced by sex or gender.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence was used in the preparation of this paper.
AUTHORS’ CONTRIBUTIONSAll authors meet the International Committee of Medical Journal Editors criteria for authorship of this article, take responsibility for the integrity of the work as a whole, were involved in drafting and critical review of the manuscript, and approved the final version for submission. All authors agree to be accountable for all aspects of the work and attest to the accuracy and integrity of the work. F. Tran and F.J. Ruperti-Repilado (first authors) contributed equally to the study design, data interpretation, and manuscript preparation. C. Mueller and D. Tobler contributed to the drafting of the manuscript, the conception of the research, and the critical revision of the manuscript. F.J. Ruperti-Repilado, F. Tran, and P. Lopez Ayala contributed to the statistical analysis. M. Freese and K. Wustmann were responsible for biomarker and CMR analysis, respectively. J. Bouchardy, M. Greutmann and M. Schwerzmann contributed to the conception and design of the study. J. Schwitter and C. Mueller were responsible for the core labs of CMR and biomarkers, respectively.
CONFLICTS OF INTERESTJ. Schwitter receives an unrestricted grant of Bayer Healthcare Schweiz AG for the research activities of the Cardiac MR Center of the University Hospital Lausanne (CHUV). C. Mueller reports receiving research support from the Swiss National Science Foundation, the Swiss Heart Foundation, the KTI, the University Hospital Basel, the University of Basel; Abbott, Astra Zeneca, Beckman Coulter, Boehringer Ingelheim, Brahms, Idorsia, LSI Medience Corporation, Novartis, Ortho Diagnostics, Quidel, Roche, Siemens, SpinChip, Singulex, Sphingotec, outside the submitted work, as well as speaker honoraria/consulting honoraria from Abbott, Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, BMS, Idorsia, Novartis, Osler, Roche, SpinChip, and Sanofi, all paid to the institution. The remaining authors report no potential conflicts of interest.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2024.05.006