There are no studies in Spain investigating the outcome of primary percutaneous interventions (PPCIs) for ST-elevation acute coronary syndrome (STEACS) performed out-of-working-hours (OWH) compared with those carried out during working hours (WH).
A retrospective analysis was performed in a cohort of STEACS patients treated by PPCI in our center between 2006 and 2014 (N = 2941). The characteristics of the sample were obtained from the center's electronic database, where patient information is prospectively recorded by the physician performing the procedure. PPCI was established as being OWH when it was performed on weekdays between 3:00 p.m. and 8:00 a.m., on weekends, or on official holidays, whereas WH PPCIs were procedures carried out on weekdays between 8:00 a.m. and 3:00 p.m.
The main event evaluated was death during follow-up. Secondary events were reinfarction, revascularization of the treated vessel, and demonstrated stent thrombosis. The electronic medical records (IANUS software) were exhaustively reviewed to estimate clinical event rates using the Kaplan-Meier method; comparisons were made with the log-rank test. Cox regression analysis was applied to assess the effect of OWH PPCI on mortality adjusted by age, sex, diabetes mellitus, previous acute myocardial infarction, creatinine clearance, hemoglobin, anterior SCACEST, Killip class, left ventricular ejection fraction, multivessel disease, radial access, total ischemia time, and the success of PPCI.
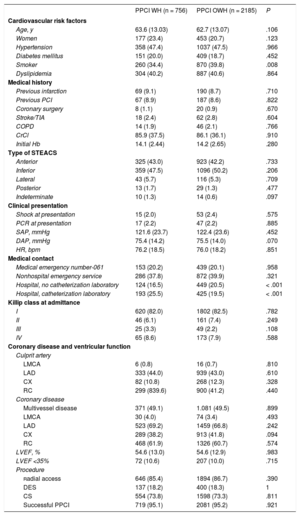
In total, 2185 OWH PPCI (74.3%) were performed. There were no differences between OWH and WH procedures with regard to the patients’ clinical or angiographic characteristics, or procedure-related factors (Table 1). PPCI success rates were similar between the 2 groups (OWH 95.2% and WH 95.1%; P = .921).
Baseline and Procedure-Related Characteristics
| PPCI WH (n = 756) | PPCI OWH (n = 2185) | P | |
|---|---|---|---|
| Cardiovascular risk factors | |||
| Age, y | 63.6 (13.03) | 62.7 (13.07) | .106 |
| Women | 177 (23.4) | 453 (20.7) | .123 |
| Hypertension | 358 (47.4) | 1037 (47.5) | .966 |
| Diabetes mellitus | 151 (20.0) | 409 (18.7) | .452 |
| Smoker | 260 (34.4) | 870 (39.8) | .008 |
| Dyslipidemia | 304 (40.2) | 887 (40.6) | .864 |
| Medical history | |||
| Previous infarction | 69 (9.1) | 190 (8.7) | .710 |
| Previous PCI | 67 (8.9) | 187 (8.6) | .822 |
| Coronary surgery | 8 (1.1) | 20 (0.9) | .670 |
| Stroke/TIA | 18 (2.4) | 62 (2.8) | .604 |
| COPD | 14 (1.9) | 46 (2.1) | .766 |
| CrCl | 85.9 (37.5) | 86.1 (36.1) | .910 |
| Initial Hb | 14.1 (2.44) | 14.2 (2.65) | .280 |
| Type of STEACS | |||
| Anterior | 325 (43.0) | 923 (42.2) | .733 |
| Inferior | 359 (47.5) | 1096 (50.2) | .206 |
| Lateral | 43 (5.7) | 116 (5.3) | .709 |
| Posterior | 13 (1.7) | 29 (1.3) | .477 |
| Indeterminate | 10 (1.3) | 14 (0.6) | .097 |
| Clinical presentation | |||
| Shock at presentation | 15 (2.0) | 53 (2.4) | .575 |
| PCR at presentation | 17 (2.2) | 47 (2.2) | .885 |
| SAP, mmHg | 121.6 (23.7) | 122.4 (23.6) | .452 |
| DAP, mmHg | 75.4 (14.2) | 75.5 (14.0) | .070 |
| HR, bpm | 76.2 (18.5) | 76.0 (18.2) | .851 |
| Medical contact | |||
| Medical emergency number-061 | 153 (20.2) | 439 (20.1) | .958 |
| Nonhospital emergency service | 286 (37.8) | 872 (39.9) | .321 |
| Hospital, no catheterization laboratory | 124 (16.5) | 449 (20.5) | < .001 |
| Hospital, catheterization laboratory | 193 (25.5) | 425 (19.5) | < .001 |
| Killip class at admittance | |||
| I | 620 (82.0) | 1802 (82.5) | .782 |
| II | 46 (6.1) | 161 (7.4) | .249 |
| III | 25 (3.3) | 49 (2.2) | .108 |
| IV | 65 (8.6) | 173 (7.9) | .588 |
| Coronary disease and ventricular function | |||
| Culprit artery | |||
| LMCA | 6 (0.8) | 16 (0.7) | .810 |
| LAD | 333 (44.0) | 939 (43.0) | .610 |
| CX | 82 (10.8) | 268 (12.3) | .328 |
| RC | 299 (839.6) | 900 (41.2) | .440 |
| Coronary disease | |||
| Multivessel disease | 371 (49.1) | 1.081 (49.5) | .899 |
| LMCA | 30 (4.0) | 74 (3.4) | .493 |
| LAD | 523 (69.2) | 1459 (66.8) | .242 |
| CX | 289 (38.2) | 913 (41.8) | .094 |
| RC | 468 (61.9) | 1326 (60.7) | .574 |
| LVEF, % | 54.6 (13.0) | 54.6 (12.9) | .983 |
| LVEF <35% | 72 (10.6) | 207 (10.0) | .715 |
| Procedure | |||
| Radial access | 646 (85.4) | 1894 (86.7) | .390 |
| DES | 137 (18.2) | 400 (18.3) | 1 |
| CS | 554 (73.8) | 1598 (73.3) | .811 |
| Successful PPCI | 719 (95.1) | 2081 (95.2) | .921 |
COPD, chronic obstructive pulmonary disease; CrCl, creatinine clearance; CS, conventional stent; CX, circumflex artery; DAP, diastolic arterial pressure; DES, drug-eluting stent; Hb, hemoglobin; HR, heart rate; LMCA, left main coronary artery; LVEF, left ventricular ejection fraction; LAD, left anterior descending artery; OWH, out-of-working-hours; WH, working hours; PCI, percutaneous coronary intervention; PCR, polymerase chain reaction; PPCI, primary percutaneous coronary intervention; RC, right coronary artery; SAP, systolic arterial pressure; STEACS, ST–segment-elevation acute coronary syndrome; TIA, transient ischemic attack. Unless otherwise indicated, the data are expressed as no. (%).
The first medical contact took place more often in a hospital that was not equipped with a catheterization laboratory in the OWH PPCI group (20.5% vs 16.5%; P < .001). No differences were found in relation to first contacts through 061 (medical emergency number) or emergency services other than hospital emergency rooms.
There were no significant differences between OWH and WH procedures regarding the time interval between symptom onset and the first medical contact (median, 74 vs 71 minutes; P = .793). The time from the first medical contact to artery-opening treatment was significantly longer in OWH PPCI (median, 128 vs 118 minutes; P < .001). The total ischemia time was longer in OWH PPCI, but this difference did not reach statistical significance (median, 221 vs 211 minutes; P = .094).
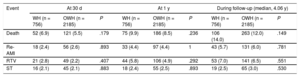
After a lengthy follow-up, (median, 1482 [interquartile range, 675-2289] days), there were no differences in mortality or in the other events studied between OWH and WH PPCI (Table 2). OWH PPCI was not associated with a higher adjusted risk of death during follow-up (hazard ratio, 0.92, 95% confidence interval, 0.71-1.19).
Incidence of Clinical Events
| Event | At 30 d | At 1 y | During follow-up (median, 4.06 y) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| WH (n = 756) | OWH (n = 2185) | P | WH (n = 756) | OWH (n = 2185) | P | WH (n = 756) | OWH (n = 2185) | P | |
| Death | 52 (6.9) | 121 (5.5) | .179 | 75 (9.9) | 186 (8.5) | .236 | 106 (14.0) | 263 (12.0) | .149 |
| Re-AMI | 18 (2.4) | 56 (2.6) | .893 | 33 (4.4) | 97 (4.4) | 1 | 43 (5.7) | 131 (6.0) | .781 |
| RTV | 21 (2.8) | 49 (2.2) | .407 | 44 (5.8) | 106 (4.9) | .292 | 53 (7.0) | 141 (6.5) | .551 |
| ST | 16 (2.1) | 45 (2.1) | .883 | 18 (2.4) | 55 (2.5) | .893 | 19 (2.5) | 65 (3.0) | .530 |
OWH, out-of-working-hours; WH, working hours; n, number of events; Re-AMI, acute myocardial reinfarction; RTV, revascularization of the treated vessel; ST, stent thrombosis. Unless otherwise indicated, the data are expressed as no. (%).
Over the last few years, there has been some controversy regarding the relationship between WH and PPCI-related death. Initial reports described higher mortality rates in OWH procedures,1,2 but this was not seen in more recent studies or in the present series. 3–5 Several explanations have been considered:4 circadian variations in myocardial perfusion, selection bias, and differences in the populations studied or the health care provided. As seen in other studies,2–4 the delays to reperfusion were were longer in OWH than WH PPCI, although the added time yielded a modest absolute value, which could explain why there was no impact of this factor on the clinical outcome. These results should be viewed in the setting of a high-volume hospital providing PPCI within a consolidated regional health care network for STEACS patients6 that offers consistent medical care for infarction in our area, regardless of the time frame. This study has the limitations inherent to a retrospective design based on an unaudited hospital database. In addition, as it did not include patients who were not treated within the publically funded health care system, those who died before PPCI could be performed, and those who could not undergo angioplasty, the series does not necessarily represent the entire population of STEACS patients. Nonetheless, this selection bias is also seen in the other related studies.
Within a network providing care for STEACS patients, OWH PPCI achieves clinical results comparable to those of procedures performed in WH.