To the Editor,
Patent ductus arteriosus (PDA) is found in more than 60% of preterm infants born at a gestational age of less than 28 weeks.1,2
The therapeutic approach to PDA consists of medical treatment with indomethacin or ibuprofen, and surgical ligation or stapling as salvage therapy. Surgery is not free of complications,2-4 with a mortality risk that ranges between 1% and 10%.2,5,6
We present the case of a newborn infant weighing 1700 grams in whom we performed percutaneous closure of PDA.
The infant was born by means of cesarean section in week 29 of gestation and weighed 1380 grams. He required the administration of surfactant, mechanical ventilation and inotropic support from the time of birth. He was found to have a multiple malformation syndrome consisting of duodenal atresia, choanal atresia, type C esophageal atresia, cleft palate, ventricular septal defect (VSD), atrial septal defect (ASD), and PDA.
Esophagoplasty and duodenoplasty were performed when he was 4 days old, with surgical accesses via right lateral thoracotomy and anterior laparotomy. He was given 2 courses of indomethacin, which failed to close the ductus.
He was referred to our center at the age of 19 days in extremely serious condition. He depended on mechanical ventilation, with bronchopulmonary dysplasia and atelectasis in right upper lobe, congestive heart disease and nosocomial sepsis caused by Staphylococcus epidermidis. Echocardiography revealed the presence of a small ostium secundum ASD, a perimembranous VSD measuring 3.5 mm and PDA with a diameter of 3 mm at the pulmonary end. A course of ibuprofen was administered following optimization of the hematocrits and the fluid balance, and persistence of the ductus was verified. Once the high surgical risk had been evaluated, the decision was made to perform percutaneous closure.
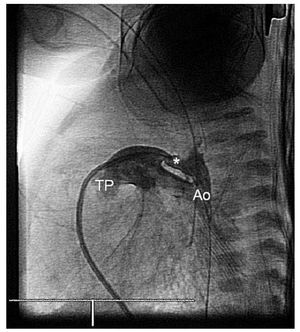
Diagnostic catheterization (Figure 1) was carried out via right femoral vein using a 4-F Terumo® introducer. Heparinization consisted of 100 U/ kg body weight. Oximetries and pressures were recorded through the ductus and the ASD, and revealed a considerable excess in pulmonary flow, basically secondary to the ductus (total Qp/Qs, 6.27; calculated for a VSD and an ASD of 2.78 mm), systemic and pulmonary pressures with normal resistances. We decided on device implantation and reevaluation of a second operation to correct the ASD and VSD.
Figure 1. Angiography in descending aorta showing the morphology of a type E patent ductus arteriosus (PDA) in which the aortic end is larger than the pulmonary end. Ao indicates descending aorta; TP, pulmonary trunk; *PDA.
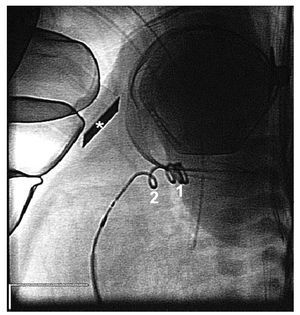
The intervention (Figure 2) involved anterograde access to the ductus (4-F Terumo® vertebral catheter). Arterial access was not established, in an effort to minimize morbidity. The ductus, which was type E, had an aortic diameter of 4 mm, a pulmonary diameter of 2.2 mm and a length of 9 mm. Implantation of a detachable coil (5-PDA 4, Cook®) was carried out. In the final follow-up monitoring of the position of the device, there was no sign of stenosis or residual ductus.
Figure 2. Endoscopic image prior to release. Note transthoracic echocardiographic monitoring (*) and normally positioned device, with 3 coils in the ductal ampulla (1) and 1 on the pulmonary side (2).
Over the following days, there was evidence of improvement in the clinical condition, thus enabling discontinuation of inotropic support and lowering of the respirator settings. At the age of 65 days, the infant developed nosocomial sepsis focalized in intestine, and died despite the administration of antibiotic therapy.
Percutaneous PDA closure was first described more than 40 years ago, and its efficiency and safety have been demonstrated,1,4,6,7 but there are very few reports of its performance in infants weighing less than 2 kg.4,8-10
The rate of failure of medical treatment ranges between 10% and 56%.2,4 Although the current recommendation is to resort to surgical closure of PDA when medical treatment has failed or is contraindicated,1,2 there are warnings about the possible negative impact of surgery on the status of a critically ill preterm infant.2-4 Thus, less invasive techniques have been developed5 and devices for percutaneous closure have been designed.7,8,10
In our opinion, although patient selection is of the utmost importance, we feel that percutaneous closure should be considered as an alternative in the treatment of PDA in the preterm newborn infant.