To the Editor,
We report the case of a 69-year-old man who was admitted to the emergency room for upper left quadrant pain, unproductive cough, and fever. In his medical history, the only remark of interest was that he was a smoker.
In the preceding week, he had consulted for a dry cough and a mild breathless sensation. In view of suspected bronchitis, he had started treatment with ß2-adrenergic inhalers. In the preceding days, he had also reported pain in the left upper quadrant and asthenia. On the day he attended the emergency room, he had maximum fever of 38°C and increased dyspnea.
In the emergency room, a good general state of health was reported, with blood pressure of 115/69mmHg and a body temperature of 37.7°C. The patient was eupneic with a heart rate of 110 bpm. Cardiac auscultation revealed arrhythmia, without murmurs; there was hypoventilation in the left inferior lobe along with some crackling mainly in the right lobe. The left rib cage was painful to palpation, which also revealed bilateral pretibial foveal edemas. The rest of the physical examination was normal.
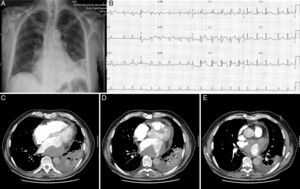
Chest X-ray revealed an anterior condensation in the left lower lobe, with an air bronchogram sign and an indistinct left costophrenic angle (Figure 1A). The electrocardiogram showed atrial fibrillation with ventricular response at 120 bpm. Complete right bundle branch block and ST elevation was reported, with concave up form in leads V2 to V5 (Figure 1B).
Figure 1. A: Posteroanterior chest X-ray: condensation in the left lower lobe. B: Electrocardiogram; atrial fibrillation and ST elevation in leads V2-V5. C-E: Computed tomography of the chest; condensation in the left lower lobe and left pleural effusion.
The laboratory workup highlighted only mild leukocytosis (10 100 × 109/L). The remaining hematological parameters and the complete biochemistry profile were normal.
With suspected left lower lobe pneumonia, treatment with amoxicillin-clavulanic acid was started and the patient was admitted to the respiratory medicine department. Once the patient was admitted, a computed tomography of the chest was performed. Pulmonary thromboembolism was ruled out and a condensation in the left lower lobe was confirmed, and left pleural effusion detected (Figure 1C-E). An echocardiogram was then requested.
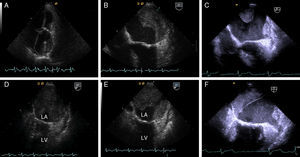
The transthoracic echocardiogram showed a normal-sized left ventricle with normal systolic function, a severely dilated left atrium with an image compatible with a thrombus adhered to the posterior and lateral wall (Figure 2A). The mitral valve showed characteristic signs of being rheumatic, with very predominant severe stenosis. The aortic valve showed signs of sclerosis. The tricuspid valve, which was morphologically normal, showed mild regurgitation. The systolic pulmonary artery pressure was estimated to be 58mmHg. These findings were confirmed by transesophageal echocardiography (Figure 2B, D, and E).
Figure 2. A: Transthoracic echocardiography; highly dilated left atrium, with adhered thrombus. B, D, and E: Transesophageal echocardiography; thrombus in the left atrium. C and F: Follow-up transesophageal echocardiography. LA indicates left atrium, LV, left ventricle.
Thoracocentesis was performed to study the pleural effusion; the pleural fluid obtained was characteristic of transudate, and so an infectious, inflammatory, or tumoral origin was ruled out. Anticoagulation was started with low molecular weight heparin and the patient was transferred to the cardiology department. He received β-blockers; ventricular response was controlled, the symptoms disappeared, and he remained without fever and in a good general state throughout the rest of his stay in hospital.
The follow-up electrocardiograms did not show any significant changes with respect to admission, and the condensation and left pleural effusion disappeared in the chest X-ray.
The patient was reassessed taking into account his clinical course and the outcomes of the complementary tests. This led us to conclude that the left pleural effusion was associated with pulmonary venous hypertension (resulting from severe mitral stenosis of rheumatic origin) and the hindered drainage of the inferior left pulmonary vein due to the presence of a large atrial thrombus. The patient was discharged with treatment with coumadin and low-dose bisoprolol/hydrochlorothiazide.
One month after discharge from hospital, a second echocardiographic follow-up was performed. This showed a notable decrease in the thrombus which no longer blocked the outlet of the pulmonary veins (Figure 2C and F). In the follow-up electrocardiogram, the right bundle branch block and ST elevation in leads V2-V6 remained.
The finding of a large mass in the chamber required a differential diagnosis between a thrombus and a tumor. The presence of valve disease and previously undetected atrial fibrillation, along with the echogenic characteristics of the mass, suggested that the origin was more likely thrombotic. The decrease in size after anticoagulation confirmed this hypothesis.
Although the initial clinical signs and symptoms and radiologic imaging were suggestive of pneumonia, this diagnosis became increasingly untenable given the clinical and radiology course, the response to treatment, and the transudate characteristics of the pleural effusion. Localized pulmonary edema has been described,1 although it is not very common. Unilateral cardiogenic pulmonary edema often leads to an erroneous initial diagnosis, as it is usually confused with pneumonia, and this can causes delays in initiating appropriate therapy.2
Causes of unilateral cardiogenic pulmonary effusion can vary. They can be the result of vascular or bronchial obstruction, congenital heart diseases,3 or severe mitral regurgitation.4
The persistence in the electrocardiogram of a subepicardial lesion brought into question the initial suspected diagnosis of possibly compromised pericardium resulting from proximity to the lesion, and it was classed as a normal variation given that previous electrocardiograms were not available for comparison.
Corresponding author: miryammpascual@gmail.com