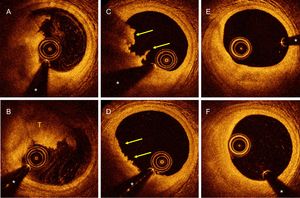
A 34-year-old man, who was a heavy smoker, presented with a 1-hour history of crushing precordial pain and ST-segment elevation in V1 to V3. He was given aspirin and a loading dose of prasugrel. Urgent coronary angiography showed an image of clearance in the proximal left anterior descending artery, visible on different projections, with the other coronary vessels angiographically normal. Optical coherence tomography (OCT) showed (Figure A and B) a large mixed thrombus (T) with a marked posterior shadow, but with no signs of plaque rupture, and a good residual lumen (* indicates guidewire artefact). Since the patient was asymptomatic, the lesion was not angiographically significant, and anterograde flow was normal, it was decided to give abciximab (intracoronary bolus followed by infusion) and thereafter continue anticoagulation with low-molecular weight heparin. At 5 days postinfarct, repeat coronary angiography showed a clear improvement in the image of clearance, and OCT revealed a significant reduction (arrows) in the intraluminal thrombus (Figure C and D) with no signs of plaque rupture. After 3 months of dual antiplatelet therapy, the final coronary angiogram showed a completely normal left anterior descending artery. OCT confirmed an underlying, intact (no ruptures or fissures) fibrous plaque, with no traces of residual thrombus (Figure E and F).
In this patient, OCT allowed confirmation of the diagnosis of fibrous plaque erosion as the pathophysiological substrate of the myocardial infarction, with subsequent stabilization and complete resolution, simply with intensive antiplatelet therapy.