Keywords
INTRODUCTION
Sustained monomorphic ventricular tachycardia (SMVT) in patients with a previous myocardial infarction (MI) is usually characterized by a wide QRS complex. Patients have occasionally been reported to have SMVT and a QRS complex <0.14 s.1,2 This "pseudonarrowing" of the QRS complex has been attributed to both a septal location of the circuit and an early penetration of the His-Purkinje system, with a later rapid activation of the rest of the ventricular myocardium.2 However, the characteristics of this type of tachycardia have not yet been studied systematically and the results of radiofrequency ablation (RFA) have not been previously analyzed. The aim of this study was to determine the incidence of SMVT with a QRS <140 ms (narrow SMVT: N-SMVT) and analyze its clinical and electrophysiological characteristics, as well as the results of RFA.
METHODS
This retrospective study included 135 patients with a prior MI before admission to our center in whom at least one SMVT was induced during the electrophysiological study. We examined the incidence, clinical and electrophysiological characteristics and the results of RFA in the patients in whom at least one N-SMVT was induced.
The anti-arrhythmic medication was suspended five half-lives before the study. The duration of the QRS complex was measured in the electrocardiogram lead recording the greatest width for which the start and end of the QRS were clearly evident, determined by two independent observers, with a recording speed of 100 mm/s. In the event that the clinical SMVT was able to be induced again, this constituted the sole end point of the RFA. In patients in whom its induction was not possible, only the "non-clinical" SMVT that was induced most frequently, with a cycle length (CL) >240 ms and hemodynamically tolerated, was considerd.
Identification of the slow conduction zone of the circuit was made by initial approximation to the suspected region with the search for fragmented potentials of low amplitude and appearance, coinciding with or later than the most delayed portions of the QRS complex in sinus rhythm. Once the SMVT was induced, the criteria used were: recording of the mid-diastolic potentials, entrainment with concealed fusion, postentrainment return cycle not more than 30 ms greater than the cycle length of the SMVT and electrogram-QRS interval during the SMVT the same as the spike-QRS interval during entrainment.3,4
The radiofrequency applications were done by a catheter with a 4 mm distal electrode in those catheter positions in which at least two of the previously mentioned mapping criteria were fulfilled.
The impossibility of later reinduction of the SMVT when RFA had been done was considered to reflect an efficient RFA. An automatic defibrillator was implanted in the patients with an ejection fraction (EF) <35% whose RFA was done after publication of the MADIT study.5
Statistical Analysis
The data are expressed as the mean (standard deviation) or the median (interquartile range), depending on the type of distribution. The interobserver variability was analyzed by the intraclass correlation coefficient.
RESULTS
Of the 135 patients included in the study, eight (5.9%) had SMVT with QRS <140 ms. The main clinical characteristics of these patients are shown in Table 1.
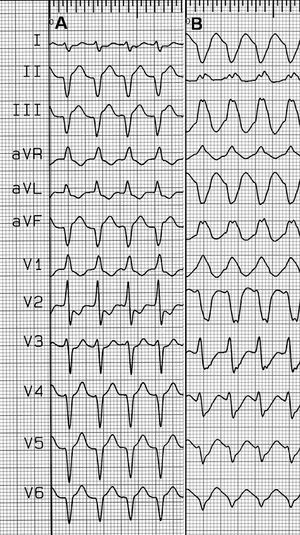
One single N-SMVT morphology was induced in all eight patients. The mean number of SMVT induced per patient was 3.8 (1.5). In four of these, the SMVT induced was similar to the clinical SMVT. No induced SMVT with a wide QRS complex (W-SMVT) had a similar morphology to its respective N-SMVT. However, in three patients, the W-SMVT induced showed a bundle branch block image concordant with the N-SMVT, as did five of the six morphologies induced in another two patients (Figure). All the N-SMVT and 92% of the W-SMVT were induced from the apex of the right ventricle. The interobserver variability of the duration of the QRS complexes of the N-SMVT had a correlation coefficient (R) of 0.77. The main electrophysiological characteristics of these patients are shown in Table 2.
Figure. Twelve lead electrocardiographic tracings at 25 mm/s of 2 ventricular tachycardias (VT) induced in the same patient A: narrow QRS complex VT. B: wide QRS complex VT
The intrachamber mapping showed a SMVT origin in the left ventricle in all the patients. The entrainment of the N-SMVT from the apex of the right ventricle showed return cycles 70 ms greater than the cycle length. The characteristics of the mapping and the RFA are given in Table 3. After the efficient RFA, in three patients it was impossible to reinduce any of the SMVT, whereas in two patients just poorly tolerated SMVT were inducible, with a CL <240 ms.
One of the two patients in whom RFA was not done had a mechanical septal block of the N-SMVT during the mapping, which was impossible to reinduce later. No exhaustive mapping was performed in the other patients due to the state of the patient and the long procedure time. For this reason no areas were found that fulfilled at least two criteria for RFA and treatment was started with amiodarone (Table 3).
DISCUSSION
The incidence of SMVT with a QRS complex <140 ms in patients with a prior MI was 5.9%. Although their presentation is uncommon, N-SMVT must nevertheless be considered in the differential diagnosis with supraventricular tachycardia with aberrant conduction.
Miller et al2 reported an incidence of 12% N-SMVT (¾0.14 s) in a series of patients with SMVT. This greater incidence as compared with our study might be explained by the inclusion in their series of idiopathic SMVT, which, because they originate near the divisions of the left branch, usually present a narrow QRS complex, as well as having considered a cut-off point that was "lower than or equal to" rather than just "lower than" 0.14 ms, as was the case in our study. Additionally, Hayes et al6 described an incidence of N-SMVT (¾0.11 s) of 4.7%. Unlike these results, in our study no N-SMVT was induced with a QRS duration <0.11 s. Although the methodology used for measurement was not reported in their series, the differences with our study could be attributed to the greater precision of the digital measurements used nowadays.
As already mentioned, a short QRS complex duration is attributed to a circuit exit of the N-SMVT in the proximity of the interventricular septum. Although the spatial localization of the slow conduction zone was not confirmed by RFA in all the patients, the septum was the most common site of this zone of the circuit in the cases with an efficient RFA (80%), as well as probably in the cases with mechanical block during the procedure. Although the data support this hypothesis, the results should be confirmed in larger series of patients.
Bogun et al described the presence of a shared isthmus in some 40% of post-MI SMVT.7 The main feature of this shared tissue is that the same slow conduction zone may be a vital component in sustaining different SMVT, which would permit the concurrence of different morphologies of induced SMVT. In our study, the inability to reinduce mappable SMVT (CL >240 ms) after an efficient RFA in all the patients indicates that, as an expression of different ventricular exits, the same patient may have not only SMVT with a different morphology but also SMVT with a different QRS complex duration or cycle length.
Finally, the success rate of the RFA in patients with N-SMVT was comparable with the results of other series on SMVT RFA and prior MI.8,9 Nevertheless, due to the limited number of patients with N-SMVT, these results should be confirmed in larger series of patients.
Correspondence Dr. J.L. Merino.
Unidad de Arritmias y Electrofisiología.
Paseo de la Castellana, 261. 28046 Madrid. España.
E-mail: jlmerino@secardiologia.es
Received April 25, 2006.
Accepted for publication November 2, 2006.