Nowadays, an increasing number of women with complex congenital heart disease live to reach childbearing age. Pregnancy, childbirth, and the postpartum period lead to physiological changes that involve an increased risk of decompensation in pregnant women with heart disease.1 While patients who have undergone the Fontan-Kreutzer procedure may have a successful pregnancy, there is a greater risk of cardiovascular events and a higher incidence of fetal and neonatal disorders.2
Here, we present 2 cases of pregnant women palliated with the Fontan-Kreutzer procedure with distinct clinical courses. To our knowledge, these are the only 2 cases in Spain with these characteristics that have ended in a successful pregnancy.
The first is the case of a 24-year-old pregnant woman with a single left ventricle, severe pulmonary stenosis, and L-transposition of the great vessels, who was palliated with a Blalock–Taussig shunt followed by the Fontan-Kreutzer procedure at the age of 4 years. She was asymptomatic during the course of the pregnancy, with normal function of the atriopulmonary connection, normal ventricular function, and mild aortic regurgitation.
In week 32 of pregnancy, she showed an irregular uterine dynamic, and fetal lung maturity was assessed. The dynamic spontaneously resolved after 48hours. In week 36, she reported reduced tolerance to exertion and an occasional sensation of palpitations. A follow-up echocardiogram revealed a slight increase in aortic regurgitation. Given the risk of hemodynamic deterioration and the breech presentation of the fetus, the decision was made to end the pregnancy with an elective cesarean section, using epidural anesthesia with fractional doses. A healthy boy was delivered, weighing 2480 g. The postpartum course was favorable. Now, at the age of 35 years, the patient is in New York Heart Association functional class II and has moderate aortic regurgitation. She received no anticoagulation during her pregnancy and later began antiplatelet therapy with aspirin 100 mg.
The second case is a 31-year-old pregnant woman with a double-inlet left ventricle, L-transposition of the great vessels and severe pulmonary stenosis. She was palliated with the Fontan-Kreutzer procedure at the age of 13 years. Cardiology follow-up revealed normal function of the atriopulmonary connection and normal ventricular function. She had been taking antiplatelet therapy with aspirin 100 mg since the age of 24 years. She was asymptomatic until the age of 27 years, when she experienced an initial episode of atrial flutter, requiring electrical cardioversion. She began treatment with amiodarone 200 mg/24 h, and had a relapse of the atrial flutter after 1 year. Ablation was performed (macroreentry around the atriotomy scar), there was alternation between nodal/sinus rhythm, and the antiarrhythmic treatment was withdrawn after 3 months.
During the pregnancy, the antiplatelet therapy was replaced by enoxaparin 1 mg/kg/12 h. By week 28, she had experienced 5 episodes of atrial flutter requiring electrical cardioversion and attempts to control her heart rate with bisoprolol and amiodarone, which were ineffective due to recurrences and bradycardia. Further echocardiograms showed no changes compared with those performed before the pregnancy. At week 29, she had a premature spontaneous normal birth, with no complications. A healthy boy was born, weighing 1,400 g. Postpartum monitoring revealed sinus bradycardia with significant sinus pauses, and implantation of a VVIR epicardial pacemaker was indicated. She was discharged with acenocoumarol.
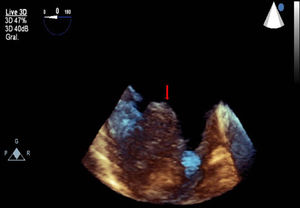
In the routine follow-up 6 months after delivery, a right intra-atrial thrombus was detected (Figure), which resolved without any incidents after switching the anticoagulation prescription to enoxaparin 1 mg/kg/12 h+aspirin 100 mg. She later required 2 further ablations at the age of 36 and 38 years (cavotricuspid isthmus and lateral wall of the right atrium). She experienced no other cardiovascular events during the clinical course. At the age of 39 years, the pacemaker was replaced with a dual-chamber endocavity model with a ventricular lead in the coronary sinus. Currently, at the age of 40 years, she has mild-to-moderate dysfunction of the single ventricle and is in functional class II. She is under treatment with acenocoumarol, bisoprolol, sildenafil, and spironolactone.
The Fontan-Kreutzer procedure and its modifications have improved survival in patients with single ventricle defects who reach childbearing age. The combination of hypoxemia before palliation and subsequent chronic venous congestion can affect ovarian function.3 The most common obstetric complications are premature rupture of membranes, intrauterine growth retardation, and premature birth, and there is an increased risk of neonatal death and miscarriage. Arrhythmias,3 most commonly supraventricular arrhythmias, often complicate pregnancies, particularly in patients with atriopulmonary anastomosis.
The changes that occur during pregnancy are particularly unfavorable in women palliated with the Fontan-Kreutzer procedure, as it can alter the delicate and paradoxical balance between the high central venous pressure and the low pulmonary pressures. The ability to increase cardiac output is limited, leading to poor tolerance to atrial arrhythmias. Patients who have undergone the Fontan-Kreutzer procedure have a high thromboembolic risk, mainly in the atriopulmonary connection. Anticoagulation therapy with low–molecular-weight heparin should therefore be considered during pregnancy and in the peripartum period for this subgroup of patients, with monitoring of anti-Xa and platelet concentrations.4,5
While specific patients may have a successful pregnancy, they should be considered as moderate-to-high risk (World Health Organization classes III and IV).6
The delivery of choice is vaginal delivery with shortening of the second stage of labor, unless there is significant worsening of ventricular function or obstetric issues. The anesthetic technique of choice is epidural with fractional doses, to minimize the repercussion on cardiac output. Close patient monitoring is recommended for at least 72hours after delivery, as well as encouragement of early movement.
Preconception counseling is essential and should begin in adolescence. If the woman becomes pregnant, she will require close multidisciplinary specialist monitoring to detect and treat any complications.