The rate of maternal mortality during pregnancy is very low in Spain.1 However, it can be as high as 1% for women with cardiovascular disease, that is, 100 times greater than in the healthy population.2
In the future, an increase in the number of pregnant women with heart disease is expected to increase as more women with congenital heart disease reach adulthood and the age of pregnancy increases. Thus, a higher number of pregnant women will have comorbidities and a risk of having heart disease. This new scenario requires all clinical cardiologists to be familiar with the initial management of pregnant woman with heart disease.
In an attempt to unify knowledge and facilitate decision making, new clinical guidelines have been published.3 These propose that appropriate counselling of women with heart disease should begin prior to pregnancy and, in the event of pregnancy, high-risk women should be referred at an early stage to specialized centers. For this, the World Health Organization (WHO) has proposed a classification to stratify the risk of maternal complications (WHO I, no increased risk of maternal mortality or mild increase in morbidity; WHO II, small increased risk of mortality or moderate increase in risk of morbidity; WHO III, significantly increased risk of mortality or severe morbidity; WHO IV, extremely high risk of mortality—pregnancy contraindicated).
The objective of this study was to present the experience in our center in the management of pregnancy in patients with structural heart disease. We used a retrospective registry covering 1998 to 2014. From 2007, pregnancy was managed in a multidisciplinary team. A specific protocol is in place for management of pulmonary arterial hypertension (PAH).4
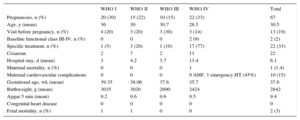
Patients were classified according to the new risk scale. The following were analyzed: heart disease, visit prior to pregnancy, functional class, anticoagulants and medication specific for heart disease, type of birth and morbidity and mortality during pregnancy, birth, and postpartum (6 months). For the baby, the gestational age, weight, Apgar test, presence of congenital heart disease, and perinatal mortality were assessed (Table).
Outcomes According to Risk Group
| WHO I | WHO II | WHO III | WHO IV | Total | |
|---|---|---|---|---|---|
| Pregnancies, n (%) | 20 (30) | 15 (22) | 10 (15) | 22 (33) | 67 |
| Age, y (mean) | 36 | 30 | 30.7 | 28.5 | 30.5 |
| Visit before pregnancy, n (%) | 4 (20) | 3 (20) | 3 (30) | 3 (14) | 13 (19) |
| Baseline functional class III-IV, n (%) | 0 | 0 | 0 | 2 (9) | 2 (2) |
| Specific treatment, n (%) | 1 (5) | 3 (20) | 1 (10) | 17 (77) | 22 (33) |
| Cesarean | 2 | 7 | 2 | 11 | 22 |
| Hospital stay, d (mean) | 3 | 4.2 | 3.7 | 13.4 | 6.1 |
| Maternal mortality, n (%) | 0 | 0 | 0 | 1 | 1 (1.4) |
| Maternal cardiovascular complications | 0 | 0 | 0 | 9 AHF. 1 emergency HT (45%) | 10 (15) |
| Gestational age, wk (mean) | 39.35 | 38.06 | 37.6 | 35.7 | 37.6 |
| Birthweight, g (mean) | 3035 | 3020 | 2890 | 2424 | 2842 |
| Apgar 5 min (mean) | 9.2 | 9.6 | 9.6 | 9.5 | 9.4 |
| Congenital heart disease | 0 | 0 | 0 | 0 | 0 |
| Fetal mortality, n (%) | 1 | 1 | 0 | 0 | 2 (3) |
AHF, acute heart failure; HT, heart transplant; WHO, World Health Organization. Unless otherwise indicated, the data are expressed as no. (%) or n.
Sixty-seven pregnancies in 62 women were included in the study (8 multiparous). The mean age of the women was 30.5 years (range, 16-42 years).
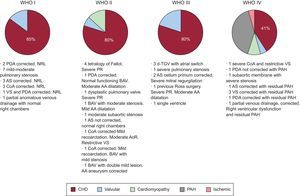
The main diseases were congenital heart disease (69%), PAH (13%), and valve disease (10%). A high percentage of mothers had PAH because our hospital is a reference center for this condition (Figure). Counselling prior to pregnancy was only given in 19% of the patients. This is mainly because our hospital takes patients referred from other centers during pregnancy. Pregnancy did not lead to birth in 5 women. Three of these had miscarriages. The other 2 women, in the WHO IV risk group, had an abortion in the first trimester. It is important that the cardiologist who attends women with congenital heart disease provides reproductive counselling and refers complex cases to reproductive health units.
Etiology according to risk group. AA, ascending aorta; AoR, aortic regurgitation; AS, atrial shunt; BAV, bicuspid aortic valve; CHD, congenital heart disease; CoA, coarctation of the aorta; d-TGV, d-transposition of the great vessels; NRL, no residual lesions; PDA, patent ductus arteriosus; PR, pulmonary regurgitation; VS, ventricular shunt.
With regards anticoagulation, 19% of the pregnant women (2 with mechanical prosthesis and 1 with complex congenital heart disease) were receiving low molecular weight heparin 1mg/kg every 12hours as anticoagulant therapy, with monitoring of anti-Xa factor. No complications were reported during pregnancy or birth.
The high rate of Cesarean deliveries in the WHO IV risk group (50%) can be attributed to a special protocol for patients with PAH that included scheduled procedures at week 36.3
The maternal mortality (1.4%) was slightly higher than that reported in the European registry (1%),2 although the percentage of patients in the WHO IV risk group IV higher in our series (33% versus 4%), largely because of the high proportion of patients with PAH. Complications and mortality are directly related to risk group.5 Manso et al6 reported mortality of 25% among high-risk patients.
The only death was a patient with severe idiopathic PAH of 1 year in functional class II, who died during an abortion at week 8 after syncope followed by bradycardia and cardiac arrest. No clear trigger was identified.
Seven of the patients in the WHO IV risk group had heart failure in the postpartum period and 1 required an emergency heart transplant. The condition of a patient with PAH worsened and she died 1 year after birth. There was one case of peripartum cardiomyopathy with an unsatisfactory outcome (the patient was placed on the waiting list for heart transplantation). One patient with severe mitral valve stenosis and moderate regurgitation, who was ineligible for valvuloplasty, underwent valve replacement after Cesarean delivery. The remaining patients did not have any relevant cardiovascular complications. Fetal mortality (3%) was due to obstetric complications (umbilical cord knot and placental abruption). There were no neonatal deaths.
We can conclude that all women with heart disease of a childbearing age should receive appropriate counselling prior to pregnancy and they should be discouraged from becoming pregnant in cases of high risk. Even so, most of the patients with heart disease, following appropriate recommendations and attended in specialized centers with multidisciplinary teams, can give birth safely.
FundingThe study was funded by the Instituto de Salud Carlos III, Ministry of Economics and Competitiveness, through the Cardiovascular Research Network.