This consensus document on cardiovascular disease in women summarizes the views of a panel of experts organized by the Working Group on Women and Cardiovascular Disease of the Spanish Society of Cardiology (SEC-GT CVD in Women), and the Association of Preventive Cardiology of the SEC (ACP-SEC). The document was developed in collaboration with experts from various Spanish societies and associations: the Spanish Society of Gynecology and Obstetrics (SEGO), the Spanish Society of Endocrinology and Nutrition (SEEN), the Spanish Association for the Study of Menopause (AEEM), the Spanish Association of Pediatrics (AEP), the Spanish Society of Primary Care Physicians (SEMERGEN), the Spanish Society of Family and Community Medicine (semFYC), and the Spanish Association of Midwives (AEM). The document received formal approval from the SEC. This consensus serves as a guide for the clinical community on the diagnostic approach and management of cardiovascular health during the stages or life cycles of women: adolescence, the menopausal transition, postpartum disorders, and other gynecologic conditions. It is based on current evidence and best available practices.
Keywords
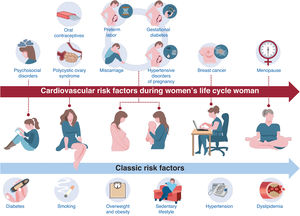
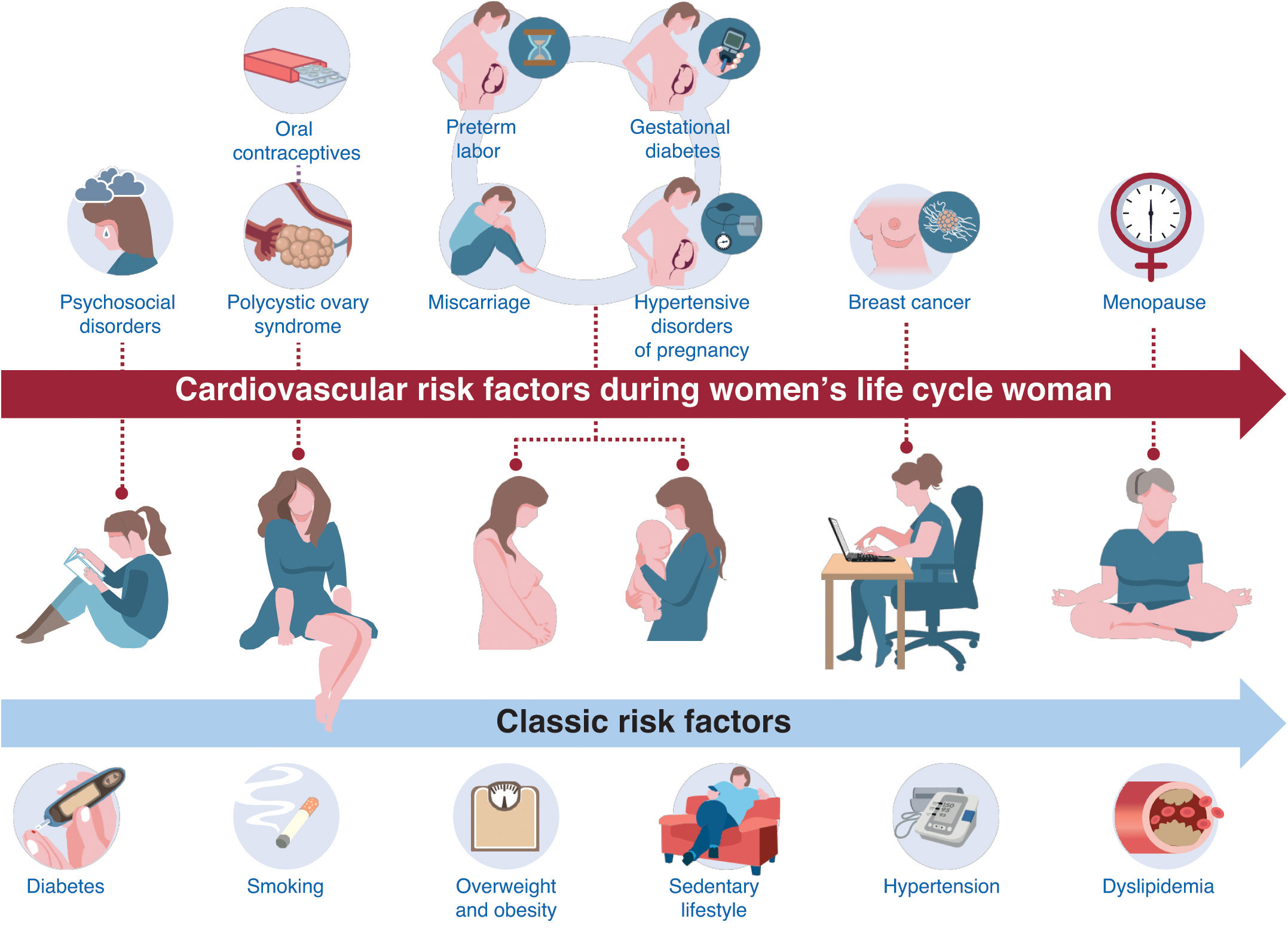
Cardiovascular disease (CVD) is the leading cause of mortality in women, accounting for 35% of total deaths in women in 2019.1 While age-standardized CVD mortality in women has declined globally over the past 30 years,2 a rise in acute myocardial infarction (MI) has been documented among younger women in the last decade.3–5 Early detection and targeted management of both sex-specific and nonsex-specific cardiovascular risk factors (CVRF) in women play an indisputable role in reducing the overall CVD burden in this population.
This multidisciplinary consensus document aims to provide recommendations on the management of primary and secondary cardiovascular prevention in women throughout different life stages based on existing evidence and current best available practices (figure 1). Likewise, this document gathers the opinions of a panel of experts organized by various scientific societies and associations in Spain: the Working Group on Women and Cardiovascular Disease of the Spanish Society of Cardiology (SEC-GT CVD in Women), the Association of Preventive Cardiology of the SEC (ACP-SEC), the Spanish Society of Gynecology and Obstetrics (SEGO), the Spanish Association for the Study of the Menopause (AEEM), the Spanish Society of Endocrinology and Nutrition (SEEN), the Spanish Society of Family and Community Medicine (semFYC), the Spanish Society of Primary Care Physicians (SEMERGEN), the Spanish Association of Pediatrics (AEP), and the Spanish Association of Midwives (AEM).
METHODSAuthors with expertise in CVD prevention in women were selected to contribute to this consensus statement. Participants volunteered to write sections relevant to their knowledge and experience. Writing groups from various associations (SEC, SEC-GT CVD in Women, ACP-SEC, SEGO, AEEM, SEEN, semFYC, SEMERGEN, AEP, and AEM) identified relevant literature and prepared a first draft of the document. The sections were edited based on feedback from all coauthors and discussions within the whole group, and a final version was produced.
The strength of the evidence supporting the recommendations was evaluated and graded scored according to predefined scales, following the European Society of Cardiology (ESC) guidelines:
- -
Level of evidence A: data derived from multiple randomized clinical trials or meta-analyses.
- -
Level of evidence B: data derived from a single randomized clinical trial or large nonrandomized studies.
- -
Level of evidence C: expert consensus and/or small studies, retrospective studies, or registries.
Adolescent girls (10-21 years) have 3 key risk factors to consider: an increase in fat mass and adipose tissue, which is proportionally greater than in boys (25% vs 14%),6 a decline in moderate-vigorous physical activity7 and an increase in cigarette consumption, which is now more frequent than in boys.8 Recommendations for managing of classic CVRF are shown in .
Sex-specific cardiovascular risk factorsPolycystic ovary syndrome, hypogonadotropic hypogonadism, and premature ovarian insufficiency share estrogen deficiency and are significant CVRF. Recent studies estimate that polycystic ovary syndrome affects approximately 8% to 13% of women of reproductive age, making it one of the most common endocrine disorders.9 Women with these hormonal imbalances are more likely to develop metabolic disorders, such as insulin resistance, central obesity, and dyslipidemia, as well as hypertension. Furthermore, estrogen deficiency is associated with chronic low-grade inflammation and endothelial dysfunction, which can increase the incidence of coronary artery disease and cerebrovascular events.9 In the case of endometriosis, elevated estrogen levels may also play a role in increasing cardiovascular risk. Chronic pain and associated symptoms of endometriosis can cause significant psychological stress, increased blood pressure, and changes in heart rate variability, further contributing to cardiovascular risk. To promote optimal cardiovascular health, monitoring and individualized strategies should be implemented. Gonadal hormone replacement therapy (HRT) is recommended in premenopausal women with premature ovarian insufficiency or hypogonadotropic hypogonadism provided no contraindications exist (level of evidence A).9 Transdermal estrogens have shown a more favorable impact on cardiovascular risk biomarkers than oral estrogens.
Transgender peopleThe reasons for consultation in primary care among transgender individuals are similar to those of the general population, including participation in preventive health programs.10 The clinical history should serve the same objectives as in any other patient but must also include specific data, such as the use of HRT and the age of onset, as this carries cardiovascular risk side effects. For instance, trans women have an increased risk of hypertension, dyslipidemia, and venous thromboembolism. In trans men with premature ovarian insufficiency, screening for diabetes is recommended. Consequently, periodic blood pressure monitoring and analytical tests, including lipid and glycemic profiles, is advised. The frequency of these tests should be individualized based on the patient's risk stratification, using tools such as SCORE2.11 SCORE2 is a cardiovascular risk assessment tool used in Europe to predict the 10-year risk of fatal and nonfatal cardiovascular events in individuals aged 40 to 69 years.
Use of assisted reproductive technologyThe use of assisted reproductive technology is associated with increased cardiovascular risk; this is most likely due to the higher prevalence of established cardiovascular risk factors among women with infertility such as advanced maternal age, chronic hypertension, diabetes, obesity, and polycystic ovary syndrome.11
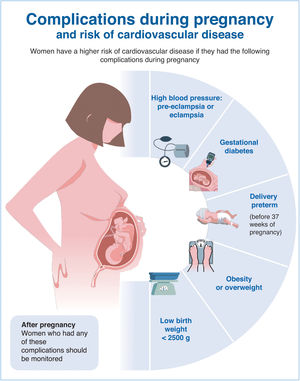
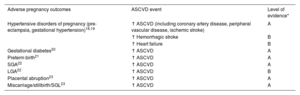
CARDIOVASCULAR RISK FACTORS IN PREGNANCYThe cardiovascular system undergoes significant structural and hemodynamic changes during pregnancy. Furthermore, several metabolic changes increase lipid levels and hypercoagulability.12 In women with prepregnancy cardiometabolic risk factors or genetic or environmental predisposition, the physiological stress of pregnancy may lead to adverse pregnancy outcomes (APOs), such as hypertensive disorders, intrauterine growth restriction, small-for-gestational-age neonates, placental abruption placentae, preterm delivery, and gestational diabetes mellitus (DM).13–16 Women with a history of APOs have an increased long-term risk of CVD (table 1).17–23 However, it remains unclear whether APOs reveal latent CVD risk or act as independent risk factors. Pregestational evaluation is critical for assessing CVRF in women. Early screening at 11-13 weeks aims to identify these risks.24
Adverse pregnancy outcomes and association with mortality and atherosclerotic cardiovascular disease events
| Adverse pregnancy outcomes | ASCVD event | Level of evidence* |
|---|---|---|
| Hypertensive disorders of pregnancy (pre-eclampsia, gestational hypertension)18,19 | ↑ ASCVD (including coronary artery disease, peripheral vascular disease, ischemic stroke) | A |
| ↑ Hemorrhagic stroke | B | |
| ↑ Heart failure | B | |
| Gestational diabetes20 | ↑ ASCVD | A |
| Preterm birth21 | ↑ ASCVD | A |
| SGA22 | ↑ ASCVD | A |
| LGA22 | ↑ ASCVD | B |
| Placental abruption23 | ↑ ASCVD | A |
| Miscarriage/stillbirth/SGL23 | ↑ ASCVD | A |
ASCVD, atherosclerotic cardiovascular disease; LGA, large-for-gestational-age; SGA, small-for-gestational-age; SGL, spontaneous gestational loss.
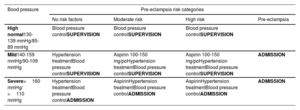
Hypertensive disorders affect nearly 10% of pregnancies worldwide. Hypertension is defined as systolic blood pressure ≥ 140mmHg and/or diastolic blood pressure ≥ 90mmHg. Women with obesity and elevated prepregnancy blood pressure are at higher risk of developing pre-eclampsia or gestational hypertension.16,17 Pre-existing hypertension is identified before pregnancy or during the first 20 weeks of gestation, while new-onset hypertension after 20 weeks is classified as gestational hypertension or pre-eclampsia (table 2).18,19 Biomarkers such as soluble fms-like tyrosine kinase-1 and placental growth factor provide nuanced predictions of pre-eclampsia and APOs, guiding interventions and offering a tailored approach to prenatal care.25 Recommendations for the management and treatment of hypertensive disorders during pregnancy are shown in table 2 and table 3.18,19
Risk definition of hypertensive disorders during pregnancy and clinical management
| Bood pressure | Pre-eclampsia risk categories | |||
|---|---|---|---|---|
| No risk factors | Moderate risk | High risk | Pre-eclampsia | |
| High normal130-139 mmHg/85-89 mmHg | Blood pressure controlSUPERVISION | Blood pressure controlSUPERVISION | Blood pressure controlSUPERVISION | |
| Mild140-159 mmHg/90-109 mmHg | Hypertension treatmentBlood pressure controlSUPERVISION | Aspirin 100-150 mg/poHypertension treatmentBlood pressure controlSUPERVISION | Aspirin 100-150 mg/poHypertension treatmentBlood pressure controlSUPERVISION | ADMISSION |
| Severe>160 mmHg/ >110 mmHg | Hypertension treatmentBlood pressure controlADMISSION | AspirinHypertension treatmentBlood pressure controlADMISSION | AspirinHypertension treatmentBlood pressure controlADMISSION | ADMISSION |
Moderate risk pre-eclampsia (2 risk factors or more): nulliparity, age >40 years, intergenic interval >10 years, body mass index >35 kg/m2, family history of pre-eclampsia, multiple pregnancies.
High risk (at least 1 more risk factor): other hypertensive disorders during previous pregnancies, chronic hypertension, chronic kidney disease, diabetes mellitus, autoimmune diseases (lupus, antiphospholipid syndrome), assisted reproductive therapy in this pregnancy.
Pre-eclampsia (blood pressure ≥ 140/90mmHg and at least 1 more risk factor): proteinuria (protein/creatinine ratio >30 mg/mmoL), creatinine >1mg/dL, elevated aspartate aminotransferase and/or alanine aminotransferase >40 IU/L, neurological complications (stroke, blindness, severe migraine, clonus), platelets <150 000/mL, hemolysis, uteroplacental insufficiency, abnormal umbilical artery Doppler. If the diagnosis is uncertain, determine the following biomarker: sFIt-1/PlGF (placental growth factor) ratio ≥ 85 PlGF <12 pg/mL.
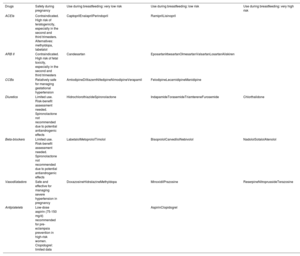
Hypertensive disorders pose significant risks, including severe cardiovascular events for the mother feal death (). In cases of chronic hypertension, angiotensin II receptor blockers and angiotensin-converting enzyme inhibitors should be avoided during pregnancy (table 4). Safe antihypertensive medications during pregnancy include methyldopa, labetalol, and nifedipine. Conversely, statins have traditionally been contraindicated due to potential teratogenic effects,26 although recent studies suggest they may prevent pre-eclampsia.27
Classification and risk categories of antihypertensive and antiplatelet drugs during pregnancy and breastfeeding
| Drugs | Safety during pregnancy | Use during breastfeeding: very low risk | Use during breastfeeding: low risk | Use during breastfeeding: very high risk |
|---|---|---|---|---|
| ACEIs | Contraindicated. High risk of teratogenicity, especially in the second and third trimesters. Alternatives: methyldopa, labetalol | CaptoprilEnalaprilPerindopril | RamiprilLisinopril | |
| ARB II | Contraindicated. High risk of fetal toxicity, especially in the second and third trimesters | Candesartan | EposartanIrbesartanOlmesartanValsartanLosartanAliskiren | |
| CCBs | Relatively safe for managing gestational hypertension | AmlodipineDiltiazemNifedipineNimodipineVerapamil | FelodipineLecarnidipineManidipine | |
| Diuretics | Limited use. Risk-benefit assessment needed. Spironolactone not recommended due to potential antiandrogenic effects | HidrochlorothiazideSpironolactone | IndapamideTorasemideTriamtereneFurosemide | Chlorthalidone |
| Beta-blockers | Limited use. Risk-benefit assessment needed. Spironolactone not recommended due to potential antiandrogenic effects | LabetalolMetoprololTimolol | BisoprololCarvedilolNebivolol | NadololSotalolAtenolol |
| Vasodilatadors | Safe and effective for managing severe hypertension in pregnancy | DoxazosineHidralazineMethyldopa | MinoxidilPrazosine | ReserpineNitroprussideTerazosine |
| Antiplatelets | Low-dose aspirin (75-150 mg/d) recommended for pre-eclampsia prevention in high-risk women. Clopidogrel: limited data | AspirinClopidogrel |
ACEIs, angiotensin-converting enzyme inhibitors; ARB II, angiotensin receptor blockers II; CCBs, calcium channel blockers.
Gestational DM is associated with to maternal and fetal complications, such as pre-eclampsia, cesarean delivery, and macrosomia, leading to birth trauma. Early diagnosis and management during pregnancy, usually between weeks 24 and 28, with diet, physical activity, and insulin, are essential to reduce risks and ensuring healthy outcomes. Multidisciplinary care is recommended for women at risk of developing gestational DM. A team comprising an obstetrician, endocrinologist, diabetes educator, and dietitian can work collaboratively to improve pregnancy outcomes.28
ObesityObesity is the most common medical condition affecting women of reproductive age, with short- and long-term adverse effects on both mothers and children during pregnancy. It increases the risk of infertility, spontaneous miscarriage, congenital anomalies, insulin resistance, glucose intolerance, and fetal overgrowth. At term, obesity is associated with higher risks of cesarean delivery, surgical wound infections, deep vein thrombosis, pulmonary embolism, and breastfeeding difficulties arise. Moreover, maternal overweight and obesity contribute to an estimated 11% of neonatal deaths.29
Spontaneous gestational losses and spontaneous preterm birthIn pregnant women, it is important to differentiate between spontaneous preterm birth and spontaneous abortion. Spontaneous preterm birth occurs between weeks 24 and 37 of gestation, whereas spontaneous abortion usually occurs before 24 weeks. Recurrent pregnancy loss is associated with cardiovascular risk, likely due to the procoagulant and proinflammatory state associated with recurrent miscarriages.30 These conditions increase the cardiovascular risk in women in the long-term (table 1).
FOURTH TRIMESTER: POSTPARTUM FOLLOW-UPThe fourth trimester refers to the period following delivery through the first 12 weeks postpartum.31 This is a vital period for follow-up, given that over 70% of maternal deaths occur postpartum, and nearly 40% occur within the first 6 weeks.32 A fourth trimester visit is recommended to classify and assess cardiovascular risk based on APOs, lifestyle factors, and pre-existing risks. This assessment is performed by the hospital follow-up team. Emerging evidence supports the use of biomarkers and imaging for subclinical CVD screening to identify at-risk postpartum populations and tailor health care interventions.33
However, approximately 40% of women do not attend postpartum visits.31 Telemedicine has the potential to improve postpartum care by reducing some of the barriers, such as transportation and language barriers.
Role of family doctor, midwife, or obstetrician in the follow-up of women who have developed vascular or metabolic complications during pregnancyCare during the fourth trimester should focus on screening and early intervention, particularly among women at increased risk of CVD, metabolic syndrome, chronic kidney disease, and DM.34 Education, risk factor modification, and contraception should be addressed. A coordinated approach involving a midwife, obstetrician and family physician is needed to provide comprehensive postpartum support.35 After delivery, programs should include at least 3 visits during the postpartum period, with several approaches based on the predominant cardiovascular risk (CVR) ().33
Postpartum hypertension is common during the first week after delivery and usually resolves within the first 6 weeks in women with gestational hypertension or pre-eclampsia. However, late postpartum hypertension may also develop up to 6 months after delivery.17 All antihypertensive agents used during pregnancy can also be used during breastfeeding (table 4). However, methyldopa should be used with caution due to the risk of postpartum depression. There is no evidence to support the continued use of aspirin after delivery. Pre-eclampsia with more severe features is associated with a higher likelihood of hypertension. Women are advised to schedule annual visits with their family physician for pregnancy planning, blood pressure monitoring, and cardiovascular risk assessment.
During the postpartum period, women with obesity have higher cardiometabolic risks and an increased likelihood of obesity in future pregnancies. Obesity should be managed aggressively. In women with a history of gestational DM who are overweight, obese, or have prediabetes, treatment with metformin should be considered to prevent type 2 DM. These women should always be reclassified and treated, if necessary, to meet targets outlined in clinical practice guidelines.36 In addition, pediatric health supervision programs provide an excellent opportunity to identify women at risk of CVD related to pregnancy complications (figure 2).36
Currently, there are no specific recommendations for patients with spontaneous gestational losses or spontaneous preterm births, as there are for women with pre-eclampsia. However, certain recommendations should still be followed, including weight management, blood pressure monitoring, maintaining a healthy diet, and regular blood tests to assess lipid profiles.
RISK FACTOR GOALS IN THE CLIMATERIC PERIODThe climacteric period is the transitional period in women's lives between the reproductive and nonreproductive stages, usually beginning about 5 years before menopause. In women, all sex-specific factors, such as gynecological and obstetric history, should be considered, in addition to classic risk factors.37 Although clinical practice guidelines recommend a gender-neutral pharmacological approach to cardiovascular prevention based on risk, without differentiating between men and women,36 therapies indicated for cardiovascular prevention are underused in women.37
Management of the menopause periodNatural menopause typically occurs around the age of 50 years, marking the beginning of approximately one-third of a woman's life without the protective effects of estrogen.38 Menopause occurring before the age of 45 years is classified as early menopause. However, artificial menopause, resulting from surgical oophorectomy or oncological treatments, has a greater impact on women's lives than natural menopause. Estrogens provide protection against CVD and DM. Conversely, menopause and its associated metabolic changes—including central abdominal fat accumulation, obesity, sarcopenia, and dyslipidemia—increase the risk of MI and cerebrovascular events, particularly in cases of early menopause.39
Medical supervision during the menopausal transition and postmenopause is essential to reduce CVD risk and other conditions such as osteoporosis, promoting healthy aging. Current cancer screening recommendations remain unchanged. Recent studies have identified HRT as the most effective intervention for symptom relief and quality of life enhancement.39,40 Natural products have demonstrated lower efficacy in alleviating menopausal symptoms. HRT may decrease CVD and all-cause mortality in women aged <60 years and within 10 years of menopause onset.37,39 Estrogens are recommended as the primary compound for women without a uterus, while combined estrogen-progestin therapy is recommended for those with a uterus to lower the risk of endometrial cancer. Treatment decisions should be individualized. In cases of premature ovarian failure (menopause before the age of 40 years) or early menopause, HRT is strongly recommended to reduce CVD risk, ideally continuing until the average age of natural menopause.41,42 In primary prevention, evidence suggests that HRT may help reduce atherothrombotic events in women aged <60 years or within 10 years of the onset of menopause, provided there are no contraindications.43 However, in patients with high cardiovascular risk or established CVD, HRT is not recommended based on available evidence.44
It is also important to address psychological health during the climacteric and menopause phase, paying particular attention to sexuality. Sexual health concerns are highly prevalent in women with CVD. More than 60% of patients with chronic heart failure (HF) report experiencing sexual problems. The pathophysiological link between sexual dysfunction in women and CVD is less well understood than in men. Factors contributing to sexual problems in women include lubrication difficulties, psychological concerns, symptoms of CVD, and side effects of medication. Currently, there are few medical treatment options. Flibanserin is not suitable for women with CVD. Transdermal testosterone therapy cannot be recommended in women with established CVD due to lack of data.42 However, sexual education may help improve sexual health and overall well-being.
Diet, exercise, and lifestyle factorsThe Mediterranean diet is considered the most effective for cardiovascular prevention.45 A reduction in saturated fat intake is significantly associated with a decrease in cardiovascular events.42 Maintaining a smoke-free lifestyle is strongly recommended, as is managing stress, depression, and anxiety, and establishing healthy sleep and rest patterns. Regular exercise is essential at all stages of life and becomes particularly important during the climacteric phase ().
CLASSIC RISK FACTORS IN WOMENSmokingPreventing and treating smoking in women is a priority. In 2020, the prevalence of smoking among women in high-income countries was 16.1%.46 While smoking rates among men have declined in recent years, this trend has not been observed among women. Smoking in women is associated with an earlier onset of menopause, worsening osteoporosis, higher susceptibility to cancer, worsening of chronic obstructive pulmonary disease and a 25% greater risk of coronary artery disease compared with men. In addition, smoking poses serious risks during pregnancy and breastfeeding.47,48
Women have less initial success with abstinence and a greater negative emotional response. While relapses are similar between men and women, women are more likely to relapse due to emotionally adverse situations than to social events.46 The most effective strategies to achieve and maintain abstinence combine approaches with nicotine replacement therapy and pharmacological treatments. Although the efficacy of most therapies has not been compared between the sexes, research suggests that women may experience lower efficacy with nicotine replacement therapy and a higher efficacy with varenicline.46
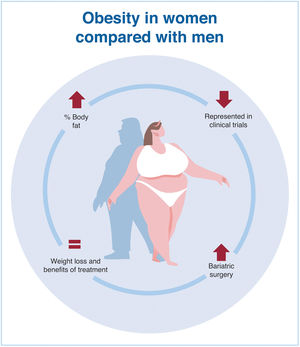
ObesityIn Europe, obesity and overweight are more prevalent among men (63%) than women (54%).49 However, women generally have a higher percentage of body fat than men. Despite these findings, women are still underrepresented in clinical trials of antiobesity drugs, and gender-specific analyses are uncommon. Current evidence suggests that sex-based differences in response to these medications are not substantial enough to warrant different dosing guidelines for men and women.49 Women are more likely than men to undergo bariatric surgery and tend to experience greater improvements in comorbidities as a result50 (figure 3).
HypertensionHigh blood pressure can affect women at every stage of life, with exacerbating factors varying by age. Women have unique risk factors that must be considered in hypertension screening and treatment guidelines, including the use of oral contraceptives, pregnancy, assisted reproductive technologies, and menopause.51 There are notable sex-based differences in hypertension management. Women are more frequently treated with diuretics, while men are more commonly prescribed angiotensin-converting enzyme inhibitors and angiotensin II receptor antagonists. This difference may partly explain why women, particularly older women, have poorer blood pressure control.52 Other factors, such as the use of pain and antidepressive medications (especially in older women) may also influence these disparities.52
DiabetesChronic hyperglycemia promotes inflammation, endothelial dysfunction, oxidative stress, and increased platelet activation, counteracting the protective effects of estrogen.53 The coronary vessels of women with type 2 DM have a smaller diameter and more complex lesons.54 Women with type 2 DM and established CVD are at very high or extreme cardiovascular risk.55 Recent advances in glucose-lowering therapies, such as glucagon-like peptide-1 receptor agonists (GLP-1ra) and sodium-glucose cotransporter 2 inhibitors, have demonstrated CV protective effects. Notably, GLP-1ra have been shown to offer more CV protection in women.56 The use of therapies with proven CV benefits is recommended, together with intensive control of all cardiovascular risk factors.
LipidsWomen have a more atherogenic lipid profile from childhood to early adulthood and from middle to old age. Transition periods in women, such as the menstrual cycle, pregnancy, breastfeeding, and menopause influence lipid levels. Women with polycystic ovary syndrome have low high-density lipoprotein cholesterol levels, high triglyceride levels, and increased low-density lipoprotein cholesterol (LDL-C) levels. Contraceptive treatments combining progesterone can increase triglyceride levels, as can oral HRT.57 During pregnancy, a physiological rise in of LDL-C and triglyceride levels is observed. In women with familial hypercholesterolemia, pregnancy has a compounding effect, leading to further LDL-C accumulation.
The ESC guidelines on the use of lipid-lowering medications, based on their cardioprotective effect, are similar for women and men.58 Dietary supplements, such as purified red yeast rice, may be considered for individuals with high cholesterol who are not candidates for statin therapy. However, the long-term safety of regular consumption of these products has not been fully demonstrated and adverse effects similar to those observed with statins have also been reported.58 Muscle-related adverse effects are more common in women, even though some studies found no sex differences, and this is a common reason for discontinuation58. Despite this, alternative statins, adjusted dosages, or side effect management strategies should be attempted to avoid discontinuation. In cases of statin intolerance, adjunctive therapies such as ezetimibe, bempedoic acid or proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors should be considered. Recently, the US Food and Drug Administration has not found sufficient evidence to contraindicate statin use during pregnancy. Therefore, statins, bile acid sequestrants, or apheresis may be considered in pregnant women with familial hypercholesterolemia or established CVD.59 However, PCSK9 inhibitors and ezetimibe are not recommended during pregnancy due to insufficient clinical data. Bempedoic acid is strongly contraindicated during pregnancy and women using it should be advised to use contraception. Lifestyle modifications, including dietary changes, are recommended for all individuals with lipid disorders and should also be considered a cornerstone of lipid management during pregnancy.
OTHER RISK FACTORS IN WOMENAutoimmune diseaseWomen are more likely to have autoimmune diseases such as systemic lupus erythematosus, rheumatoid arthritis, and inflammatory bowel diseases, which are risk factors for the development of CVD. Furthermore, during pregnancy, women with systemic lupus erythematosus are at heightened risk for cardiovascular complications including pre-eclampsia and stroke.11 Women with one of above conditions require narrow control and treatment of CVRF.
Breast cancerCVD and breast cancer have several overlapping risk factors, such as obesity and smoking. Furthermore, the risk of heart failure and myocardial ischemia is higher in breast cancer survivors. Survivors could develop latent cardiac effects secondary to the cancer treatment, which can include chemotherapy, radiotherapy, and targeted therapy.11
Psychosocial factorsPsychosocial stress is associated, in a dose-response pattern, with the development and progression of ASCVD, independently of conventional risk factors and sex. However, anxiety and depression are more frequent in women, and the later is twice common in women compared to men and should be treated and screened in patients with atherosclerotic cardiovascular disease.11
SECONDARY PREVENTION IN WOMENSecondary prevention of coronary artery disease in womenDespite women being at higher risk for secondary cardiovascular events compared to men, they remain underrepresented in trials of coronary heart disease (CHD), especially within the first 5 years.60 However, available evidence suggests that women benefit similarly from existing secondary prevention pharmacological treatments.61,62 Nonetheless, women are less likely to receive appropriate guideline-recommended medical treatments and have worse outcomes.63 For instance, women are less frequently prescribed statins, aspirin, or potent P2Y12 inhibitors (5%-10% less than men),63 even though the safety of potent P2Y12 inhibitors appears to be similar in both sexes.64
Women also have lower rates of controlled hypertension and diabetes and are less likely to be referred to appropriate cardiac rehabilitation (CR) programs.65 Furthermore, they often report more adverse medication effects than men, which can lead either patients or their clinicians to stop the medications or reduce dosages.62 The adverse-effect profiles of cardiovascular medications for women are variable and may be influenced by factors such as gastrointestinal absorption, body composition, metabolic rate, and kidney excretion. When a reduced dosage is used due to side effects, clinicians should consider gradually increasing the dose to the maximum tolerated level to maximize the treatment benefits.
Management of contraceptives in women with heart disease and use of antiplatelet therapy in menstruating womenIt is essential that women with heart disease of childbearing age use safe and effective contraceptives and that they minimize excessive blood loss associated with anticoagulants and antiplatelet medications.66 Contraceptives consisting solely of progesterone, such as the progesterone minipill, progesterone-coated intrauterine devices and progesterone implants, are recommended in these patients.67 The insertion of the implant requires only local anesthesia, whereas the insertion of a progestogen-impregnated intrauterine device should consider the use of sedation if the risk of a vagal reaction is high.66,67
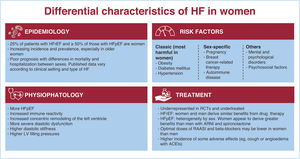
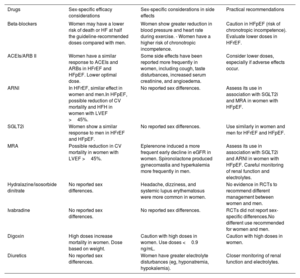
Secondary prevention of heart failure in womenHF is a prevalent condition in women,68 especially those with preserved ejection fraction (HFpEF) (table 5).68–71 Some CVRFs, such as obesity, hypertension, and DM, are more prevalent in women with HFpEF than in men. Figure 4 shows differences between the sexes related to epidemiology, pathophysiology, CVRFs, and response to treatment.70
Sex-specific efficacy and adverse effect considerations in heart failure drugs
| Drugs | Sex-specific efficacy considerations | Sex-specific considerations in side effects | Practical recommendations |
|---|---|---|---|
| Beta-blockers | Women may have a lower risk of death or HF at half the guideline-recommended doses compared with men. | Women show greater reduction in blood pressure and heart rate during exercise. - Women have a higher risk of chronotropic incompetence. | Caution in HFpEF (risk of chronotropic incompetence). Evaluate lower doses in HFrEF. |
| ACEIs/ARB II | Women have a similar response to ACEIs and ARBs in HFrEF and HFpEF. Lower optimal dose. | Some side effects have been reported more frequently in women, including cough, taste disturbances, increased serum creatinine, and angioedema. | Consider lower doses, especially if adverse effects occur. |
| ARNI | In HFrEF, similar effect in women and men.In HFpEF, possible reduction of CV mortality and HFH in women with LVEF >45%. | No reported sex differences. | Assess its use in association with SGLT2i and MRA in women with HFpEF. |
| SGLT2i | Women show a similar response to men in HFrEF and HFpEF. | No reported sex differences. | Use similarly in women and men for HFrEF and HFpEF. |
| MRA | Possible reduction in CV mortality in women with LVEF >45%. | Eplerenone induced a more frequent early decline in eGFR in women. Spironolactone produced gynecomastia and hyperkalemia more frequently in men. | Assess its use in association with SGLT2i and ARNI in women with HFpEF. Careful monitoring of renal function and electrolytes. |
| Hydralazine/isosorbide dinitrate | No reported sex differences. | Headache, dizziness, and systemic lupus erythematosus were more common in women. | No evidence in RCTs to recommend different management between women and men. |
| Ivabradine | No reported sex differences. | No reported sex differences. | RCTs did not report sex-specific differences.No different use recommended for women and men. |
| Digoxin | High doses increase mortality in women. Dose based on weight. | Caution with high doses in women. Use doses <0.9 ng/mL. | Caution with high doses in women. |
| Diuretics | No reported sex differences. | Women have greater electrolyte disturbances (eg, hyponatremia, hypokalemia). | Closer monitoring of renal function and electrolytes. |
ACEIs, angiotensin-converting enzyme inhibitors; ARB II, angiotensin receptor blockers II; ARNI, angiotensin receptor/neprilysin inhibitor; CV, cardiovascular; HF, heart failure; HFrEF, heart failure with reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonists; RCTs, randomized controlled trials; SGLT2i, sodium-glucose cotransporter 2 inhibitors.
Differential characteristics of heart failure in women. ACEIs, angiotensin-converting enzyme inhibitors; ARNI, angiotensin receptor neprilysin inhibitor, HF, heart failure; HFpEF, heart failure with preserved ejection fraction, HFrEF, heart failure with reduced ejection fraction, LV, left ventricular; RAASI, renin-angiotensin-aldosterone system inhibitor; RCTs, randomized controlled trials.
Current guidelines recommend similar therapeutic approaches for both men and women, although women are underrepresented in clinical trials.71 However, sex differences may influence women's response to pharmacological treatment (table 5). In this regard, some adverse effects might be more common in women.69 In addition, women with HF with reduced ejection fraction are less likely to receive cardiac devices, such as cardiac resynchronization therapy and implantable cardiac defibrillators than men, even though these devices have been shown to be more effective in women (table 5).72 More clinical trials involving women are needed to enhance our understanding and offer personalized management.
Cardiac rehabilitation in womenParticipation in CR programs is associated with reduced total mortality, with a more pronounced effect in women compared with men.73 In a study of 20 895 patients after MI, exercise-based CR participation was related to lowered total mortality, which was more pronounced in women than in men.74 This gender difference could be explained by a higher treatment potential in women, as women have higher mortality than men.74
Although coronary heart disease is the main indication for CR in Spain, the benefits of CR have been reported for several cardiac conditions, including HF, which is particularly prevalent in women, especially HF with preserved ejection fraction (HFpEF). However, most of the evidence on CR has focused on HF with reduced ejection fraction, although several randomized trials demonstrate the potential benefits of CR in HFpEF74 Despite these benefits, women are less likely than men to participate in CR.73
The greatest barriers among nonenrolled women who were referred to CR included a lack of awareness about CR, not being contacted by program managers, cost, and finding exercise tiring or painful.74–76 Among enrolled women, the greatest barriers to adherence to sessions were distance, transportation, and family responsibilities.65
In addition, in HF patients, these barriers are compounded by the fact that female patients tend to be older, have more comorbidities, have less social support, and have lower functional capacity than men. Most of the most effective solutions to improve CR in women are in figure 5.
Closing the gapsAddressing the gaps in cardiovascular prevention in women requires a multifaceted approach, targeting the following key areas:
- -
Raising awareness through public education and training of health professionals.
- -
Promoting sex-specific research by increasing women's inclusion in trials and sex-specific data analysis.
- -
Improving screening and diagnosis with sex-specific risk assessments and expand screening guidelines.
- -
Tailoring prevention strategies with lifestyle modifications and pharmacological interventions.
- -
Enhancing access to care, addressing disparities, and integrating multidisciplinary teams.
- -
Focusing on secondary prevention with rehabilitation programs and patient education.
- -
Promoting policy initiatives that prioritize women's cardiovascular health.
No funding was provided for this document.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENone of the authors used artificial intelligence to draft this document.
AUTHORS’ CONTRIBUTIONSA. Sambola conceived and designed the document, chose the coordinators, and distributed the different sections. A. Sambola merged and edited the different versions of the consensus document. and coordinated the secondary prevention in women section with the following authors: A. Pijuan, C. Ortiz-Cortés and R. Campuzano. A. Sambola is the author of lipids in women and secondary prevention in ischemic heart disease. R. Campuzano, A. Castro and M. Goya acted as the coordinators of the remaining main sections. R. Campuzano coordinated the section on risk factor goals in the climacteric period with the authors P. Coronado, R. Fernández-Olmo, V. Pallarés-Carratalá, M.A. María-Tablado, C. Timoteo, R.M. Plata, and B. Viejo-Hernández. R. Campuzano is the main author of cardiac rehabilitation as well as the obesity section. A. Castro coordinated the section on cardiovascular risk factors in fertile age women and the fourth trimester with the following authors: R.M. Sánchez-Hernández, B. Viejo-Hernández, M.A. María-Tablado, V. Pallarés-Carratalá and R. Fernández-Olmo, M. Goya, X. Ortolà, C. Timoteo, M.A. María-Tablado, V. Pallarés-Carratalá, and R.M. Plata, respectively. M. Goya coordinated the section on cardiovascular risk factors in pregnancy and the fourth trimester with the following authors: M.A. María-Tablado, A. Castro, B. Viejo-Hernández, V. Pallarés-Carratalá. M. Goya wrote the sections on the importance of preconception counselling, spontaneous gestational losses, and spontaneous preterm delivery. The various edited and final versions of the document have been reviewed and validated by all authors.
CONFLICTS OF INTERESTA. Sambola reports receiving advisory board fees from Novartis, as well as speaker, meeting, and travel support fees from Boehringer, Daiichi-Sankyo, and AstraZeneca; all are unrelated to the submitted manuscript. A. Castro discloses receiving fees from Novo Nordisk, Novartis, and Lilly. R.M. Sánchez-Hernández reports advisory board fees from Ultragenyx. The remaining authors declare no conflicts of interest.