Cardiac toxicity secondary to radiotherapy has an incidence of 10% to 30%. This complication usually develops 5 to 10 years after the administration of the therapy and has been related both to the location of the radiation in the thoracic region and to the dose used (generally over 40Gy). Radiotherapy-induced cardiac toxicity can lead to ischemic heart disease, different degrees of valve involvement, hypertensive heart disease, ventricular dysfunction, or changes in the intrinsic conduction system. The major causal mechanism is the fibrosis developed by the patients, which can first be detected up to 20 to 25 years after therapy was received.1–3
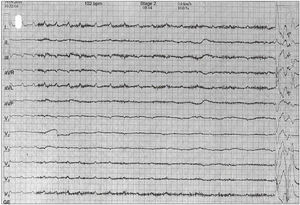
We present the case of a 44-year-old man with no cardiovascular risk factors, who had undergone radiotherapy and chemotherapy 20 years earlier to treat Hodgkin's lymphoma. He attended the emergency department after experiencing 2 episodes of exertional syncope. The initial electrocardiogram revealed complete right bundle branch block, a previously diagnosed condition (Figure 1) for which the patient had undergone cardiac evaluation a few years earlier, including transthoracic echocardiography which revealed left ventricular hypertrophy. During the first 24hours of electrocardiographic monitoring, there were no changes in heart rhythm or arrhythmic events of interest. The transthoracic electrocardiogram revealed severe mitral and aortic valve calcification, with mild aortic stenosis and moderate regurgitation. We also observed a small subvalvular aortic calcification near the anterior mitral leaflet, which did not produce an important resting gradient ().
As the syncope had occurred more than once and had been induced on both occasions by mild exertion, and given the risk associated with the patient's occupation (truck driver), an in-depth study was carried out. The responses to carotid sinus massage and tilt table test were negative. The electrophysiological study revealed an AH interval of 108ms, an HV interval of 65ms, and a supra-Hisian Wenckebach period of 410ms, all within normal limits, whereas the responses to atropine and procainamide were negative. As there was a dynamic obstruction in the left ventricular outflow tract related to the subaortic calcification, exercise echocardiography was performed in an attempt to reproduce the symptoms. In the third minute of the test, the patient developed atrioventricular dissociation with a 12-second pause (Figure 2), followed by a syncopal episode, with subsequent spontaneous recovery. The next day, he underwent implantation of a permanent dual-chamber pacemaker.
The long-term survival associated with Hodgkin's lymphoma due to the good response generally achieved with radiotherapy and chemotherapy, and the high radiation doses administered in the thoracic region 20 years earlier, were important factors in the development of cardiac toxicity over the long-term. We have no information on the chemotherapy regimen received by our patient, as it was administered at another center. The progressive myocardial fibrosis generated by the radiotherapy leads to cardiac manifestations; among these, involvement of the conduction system is one of the least frequent, compared with cardiac valve involvement, ischemic heart disease, or left ventricular systolic dysfunction, which are the most common reasons for patients with this profile to seek medical attention. The follow-up of asymptomatic patients has not been clearly established, but symptoms such as angina or dyspnea should point to radiotherapy as a possible cause in those who have undergone this treatment in the past.
Our patient had been evaluated 5 years prior to hospital admission due to the presence of asymptomatic right bundle branch block. This block is an incidental finding resulting from conduction system involvement and is generally more common than asymptomatic left bundle branch block. A thorough documentation of the syncopal episodes is essential to identify the cause of syncope, given that the results of most of the first-line complementary tests are usually normal. The exertion that precedes the syncopal episode should always guide us and alert us to a cardiac origin. The patient's occupation (truck driver) and the history of radiotherapy led us to carry out an in-depth examination of the differential diagnosis. The tests performed did not show significant changes, but revealed the existence of a subvalvular calcification that could be related to radiotherapy-induced fibrosis. The exercise echocardiogram was performed to rule out a possible dynamic obstruction of the left ventricular outflow tract, suggested by the presence of a subvalvular calcification, and because the patient's clinical signs had appeared after physical exertion.
Improvements in screening and radiotherapy have increased long-term survival in this population, due to both the reduction of the effects on exposed healthy tissue and to the lower radiation dose employed, and prolonged survival translates into longer-term follow-up.
This case highlights 2 important aspects. The first is that the evaluation of syncope involves a thorough case history and, in most patients, the existence of prior physical exertion usually indicates a cardiac origin. The second is the understanding that radiotherapy-induced cardiac toxicity can occur up to 15 to 20 years after treatment administration, normally with doses of more than 40Gy, and that, over a latent period of 25 years, up to 88% of the patients show some symptoms or signs of radiotherapy-related toxicity; these include complete right bundle branch block, as may have been the case in our patient, valve calcification, or undetected left ventricular hypertrophy or left ventricular dysfunction. Thus, it is advisable that patients with symptoms or signs of cardiac involvement undergo long-term follow-up.