Currently, individuals older than 75 years are the largest and fastest-growing population group in developed countries, including Spain.1 In this advanced age population group, cardiovascular disease remains the leading cause of death.2 In addition to this significant mortality, this disease is often accompanied by functional and/or cognitive decline and, therefore, increased dependence.3,4
Calculating cardiovascular risk (CVR) establishes the probability of having a cardiovascular event within a determined period, generally 10 years. Specifically, a cardiovascular event is taken to mean an event due to ischemic heart disease or cerebrovascular disease. Calculating CVR is interesting from a clinical perspective because it allows a more efficient assessment of which treatments should be started for primary prevention. Currently, there is clear scientific evidence on the aims and benefits of treating CVR factors in the young-old, but the evidence wanes for patients older than 75 years1,3 and is almost nonexistent for the very old. The traditional CVR factors and markers of increased probability of cardiovascular disease include hyperlipidemia, diabetes, hypertension, smoking, genetic inheritance, obesity, and sedentary lifestyle, among the most widely recognized. In the very old, some of these risk factors have a less clear association or even behave paradoxically.3 Many more risk factors continue to emerge, such as C-reactive protein, high-density lipoprotein cholesterol, homocysteine, uric acid, renal failure, vitamin D, stress, heart rate, and socioeconomic level.1,5,6 Most of these risk factors are extrapolated from a young population with no evidence for an older population. While all these individual factors have been associated with worse health outcomes, a more global assessment, using the various risk scoring systems,5–10 is considered a better approach.
Global assessment of CVR using multifactorial models predicts individual risk more accurately; however, such CVR estimation using currently available scales is of little use in older patients. The most widely used CVR scoring systems are based on the probability of having a coronary event (Framingham) or on cardiovascular mortality (SCORE [Systematic Coronary Risk Evaluation]) at 10 years. These scales have not been calibrated for people older than 75 years (Framingham) and 65 years (SCORE).3 It has been reported that the Framingham score overestimates the risk of coronary disease in populations with a low incidence, such as Spain, and has little prognostic capability in older people, especially in women7 and in the very old.5 Due to these shortcomings, the REGICOR scale was developed. The REGICOR scale consists of the Framingham tables calibrated and validated for the Spanish population up to the age of 65 years.8 In Spain, there are no population cohorts large enough to accurately predict CVR. Recently, therefore, a new cardiovascular risk equation, ERICE, was developed, using information from the individual concurrent risk of participants in various cohorts. This included 472 patients older than 80 years; thus, the recommendations can be extended to patients in this age group.9 The English-speaking world also uses the adapted Sheffield tables, which use extrapolated data from younger patients: in virtually all cases, the healthy life years gained in those older than 90 years are deemed insufficient to justify antihypertensive and lipid-lowering therapy.10 This is a particularly important point, as due to the low number of years of potential life in very old patients, they would not benefit from pharmacological interventions that require long periods to be effective.
In addition to measuring CVR, better information is needed on the importance of prevention. Currently, vascular age is a useful concept for conveying information on CVR factors to patients and thus for improving treatment adherence. The vascular age of a patient with CVR factors is defined as the age of an individual of the same sex and with the same absolute risk, but with controlled CVR factors.11 It would probably be difficult to apply the usefulness of this method to very old patients, although raising awareness of the significance of CVR factors is also important in this group.12
In CVR assessment in elderly patients, it seems important to incorporate other concepts, such as life expectancy, which is a highly relevant marker for this population. An association has been reported between high systolic blood pressure and increased mortality risk in adults who have a good walking speed, although this association is less clear in slower-walking adults.13 Therefore, the authors of the study recommend that walking speed be incorporated as a prognostic tool to identify those patients at risk of developing adverse effects of hypertension.13 Likewise, it seems appropriate to extend the concept of an incorporated frailty assessment14,15 to the application of CVR tables in elderly patients, using scoring scales or equivalents such as walking speed or the Short Physical Performance Battery. An increased presence of CVR factors has been reported in frail and prefrail patients,16 and frailty has been associated with increased risk for a number of cardiovascular factors (including obesity, high-density lipoprotein cholesterol, hypertension, and heart rate) in older people; these associations are independent of the presence of diagnosed cardiovascular disease.17 In a study of 1567 participants aged between 65 and 90 years, which used the modified Fried criteria, the results suggested that prefrailty is associated with an increased risk of developing new cardiovascular disease, and that slow walking speed is the best prognostic factor of future cardiovascular events.18 However, it is worth considering that, in these frail patients at risk of developing physical disability and/or cognitive impairment disability, if we look for it, there will probably be a high prevalence of subclinical or undiagnosed disease, such as myocardial damage seen on echocardiography, or cerebral infarction on diagnostic imaging.14 Therefore, patients with subclinical damage and coexistent frailty could be directly considered as candidates for secondary prevention without the need to apply CVR tables; this is particularly evident when the disease is in a target organ. However, it is important to clarify that frailty cannot be considered a cardiovascular disease equivalent per se, because it is not always the cardiovascular system that is the most affected in frail patients. Nor is there evidence based on clinical trials regarding the potential benefits of treating frail older people with subclinical cardiovascular disease as if it were secondary prevention.
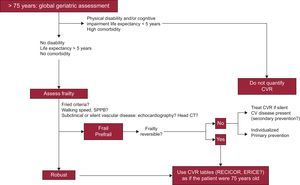
In individuals older than 75 years, then, it seems evident that the geriatric assessment of physical disability and/or cognitive impairment (especially for the basic activities of daily living) should take into account not only significant comorbidities and life expectancy > 5 years, but also a frailty assessment, to be more complete. This is especially important for the identification of robust individuals, whose CVR assessment would be similar to that recommended for the age group younger than 75 years (according to the tables that include patients in this age group: REGICOR, and perhaps in the future, ERICE).
In frail and prefrail patients, clinicians should also take into account the potential reversibility of frailty, especially with changes in physical activity and diet. If a patient is found to be frail, investigation should be considered, where possible, to exclude the presence of cardiovascular disease (silent or otherwise); if present, this situation could be regarded as one of secondary prevention. In the group of patients with purely primary prevention, it is very important to make an individualized decision and to be more vigilant in general, and in particular regarding potential drug side effects, especially from statins and aspirin.19,20 In addition, it should be borne in mind that decisions will often be based on recommendations from studies conducted in younger population groups,21 so the patient's opinion is essential. This proposed approach is presented as an algorithm in the Figure; however, before it is put into practice, more research is required in this field. Among the most important clinical questions that have yet to be resolved are: What is the best way to assess the presence of frailty? Should a diagnostic imaging study be performed in all very old patients to rule out underlying cardiovascular disease? Are pharmacological interventions effective in very old patients? Do the potential benefits outweigh the medication burden in polymedicated patients? What should be done in very old age groups (nonagenarians and centenarians), most of whom have some type of existing cardiac disease?22 It is clear that studies are needed to answer these and other questions, to help reach an agreement on more specific recommendations.
In conclusion, although CVR equations can be helpful, they should never be a replacement for clinical judgement in decision-making. Currently, most of the tables are limited to a few risk factors (age, sex, systolic blood pressure, cholesterol, and smoking) and are not useful in very old patients for the clear identification of which individuals will or will not have a fatal cardiovascular event in the future. In our opinion, adding frailty assessment23 to the concepts of disability, life expectancy, and comorbidity can help give meaning to risk quantification of cardiovascular disease primary prevention in older patients. In patients older than 75 years that are considered “robust” after a frailty assessment, it may be appropriate to equate their chronological age to a biological age of 75 years or similar. The recommendations of the CVR scales for that age group can then be followed, in the hope that future studies confirm the efficacy of such interventions against CVR factors in these patients. In frail patients, when primary prevention is implemented without the use of CVR tables, it should be individualized, with high alertness for potential adverse effects.
CONFLICTS OF INTERESTNone declared.
We would like to thank all those who have helped in reviewing this editorial for their contributions, which helped us to form these reflections, even if their opinions did not coincide completely with all of the above (Juan José Baztán, Nicolás Martínez-Velilla, Joan Espaulella, José María Mostaza, Carmen Suárez, Miguel Camafort, Fernando Rodríguez-Artalejo, Marta Fanlo, Abelardo Montero, and David Chivite).