Transcatheter mitral valve replacement (TMVR) is a therapeutic option for patients with prosthesis dysfunction and high surgical risk.1 Prosthetic valve thrombosis is a known complication of valve replacement, but there are few published reports of thrombosis of a mitral valve-in-valve prosthesis and the treatment of this condition.2–4
We present the case of a 66-year-old woman who was brought to the emergency department of our hospital in cardiogenic shock. She had a history of rheumatic valvular disease, requiring several surgical procedures: open commissurotomy in 1970; replacement of the aortic and mitral valves with metal prostheses plus a tricuspid annuloplasty in 1999; and replacement of the aortic and mitral prostheses in 2008, this time using biological prostheses. In 2016 (2 months before the current admission), and because of her high surgical risk (pulmonary hypertension, right ventricular dysfunction, and severely incompetent tricuspid annuloplasty), transcatheter implantation of an Edwards SAPIEN 3 valve-in-valve was carried out to treat mitral prosthesis dysfunction with severe regurgitation.
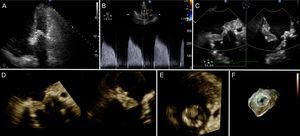
Upon arrival at our hospital, the patient was in cardiogenic shock, and treatment was initiated with vasoactive and diuretic agents, and noninvasive mechanical ventilation. On transthoracic echocardiography (TTE), the mitral prosthesis showed high pressure gradients and there was evidence of severe pulmonary hypertension with significant ventricular interdependence, causing a decrease in the left ventricular ejection fraction (Figure 1A and Figure 1B). On invasive monitoring with Swan-Ganz catheterization, pulmonary arterial pressure was 104/33/57mmHg, wedge pressure 45 mmHg, and central venous pressure 32 cmH2O. Transesophageal echocardiography (TEE), performed to investigate suspected mitral thrombosis, showed a thrombus within the prosthetic valve causing a severe obstruction (Figure 1C-F). The patient admitted that she had stopped taking anticoagulant therapy.
Echocardiographic study on admittance. A: TTE apical 4-chamber view shows right ventricular dilatation and increased ventricular interdependence, with septal displacement to the left. B: Continuous Doppler through the prosthetic mitral valve shows elevated pressure gradients. C: X-plane TEE imaging of the thrombotic mitral prosthesis. D and E: 3-dimensional TEE reconstruction enables en-face visualization of the mitral prosthesis thrombosis. F: 3-dimensional TEE view of the TMVR showing a thrombus at the anterior aspect of the valve restricting leaflet movement. TEE, transesophageal echocardiography; TMVR, transcatheter mitral valve replacement; TTE, transthoracic echocardiography.
Considering her high surgical risk, the multidisciplinary team decided to initiate fibrinolytic therapy. The regimen used was a 10-mg bolus dose of recombinant tissue plasminogen activator, followed by continuous infusion of 90mg of this drug for 90minutes, and subsequent infusion of sodium heparin as adjuvant therapy.5
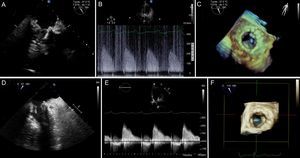
At 48hours, the patient showed clinical improvement, but continued to rely on hemodynamic support. A new TEE confirmed persistence of the thrombus obstructing the mitral prosthesis (Figure 2A-C). In the light of these findings, it was decided to repeat fibrinolytic therapy, which led to normalization of the valvular gradients and enabled discontinuation of the vasoactive support 48 hours later. A new TEE depicted significant regression of the thrombus (Figure 2C-E). As a complication of the fibrinolytic therapy, the patient experienced hematemesis that required red blood cell transfusion. Oral anticoagulation therapy was restarted following hospital discharge, and 3 months later, the patient was in functional class II/IV.
A-C: Images following the first administration of antifibrinolytic therapy. A: TEE shows a persistent thrombus in the valve-in-valve prosthesis. B: Mean pressure gradients are elevated. C: 3-dimensional TEE view depicts reduced valvular opening. D-F: Images following the second administration of fibrinolytic therapy show disappearance of the thrombus (D), a normal mean pressure gradient in the prosthesis (E), and normal leaflet opening on 3-dimensional TEE (F). TEE, transesophageal echocardiography.
Fibrinolysis is a alternative therapy for thrombosis of prosthetic cardiac valves in patients with high or prohibitive surgical risk,5 but there is no experience with this therapy for thrombosis of prostheses implanted percutaneously. To our knowledge, this is the first reported case of thrombotic dysfunction of a mitral valve-in-valve prosthesis treated with fibrinolysis. Although urgent surgery is recommended in hemodynamically unstable patients with left-sided prosthetic valve thrombosis,5 our patient's high surgical risk prompted us to choose fibrinolytic therapy. Furthermore, we decided to repeat fibrinolysis, accepting the increased risk of hemorrhage, based on the patient's clinical situation. There is some experience yielding favorable results with readministration of recombinant tissue plasminogen activator in patients with thrombotic mitral valve prosthesis dysfunction, when the first administration was unsuccessful.6
In most previously published cases of TMVR thrombosis, the patients were clinically stable and were treated conservatively using anticoagulant therapy.2,3 One patient underwent urgent surgery.4 Nonetheless, many patients who receive this type of valvular replacement are at very high surgical risk, and in these patients, fibrinolytic therapy may be a reasonable option.
.