The vascular endothelium is exposed to a hemodynamic stress generated by the blood flow known as the wall shear stress. Wall shear stress is defined as the force per unit area exerted on the vessel wall by the blood flow and it depends on blood viscosity and the blood flow velocity profile. The value of the wall shear stress is expressed in dynes/cm2 and the physiologic values in the venous system range from 1 to 6 dynes/cm2, while in the arteries they are at least 10 to 15 dynes/cm2.
WALL SHEAR STRESS AND ATHEROSCLEROSIS
The appearance and progression of atherosclerotic disease occurs as a function of both genetic predisposition and cardiovascular risk factors, such as smoking, arterial hypertension, diabetes mellitus, and hyperlipidemia. Although the different phases in the progression of atherosclerotic plaques have already been defined, the factors associated with the nature and rate of progression of a given atherosclerotic plaque are still poorly understood. In fact, although atherosclerosis is a disease affecting the vascular system as a whole, it has an uneven distribution with substantial differences in the localization and progression of different plaques. In the carotid artery, for instance, there is a well-known predisposition for atheroma plaques to develop in the outer wall of the vessel at the level of the bifurcation of the common carotid artery,1,2 and in the coronary arteries it has also been shown that there is a preferential progression of plaques in segments with bifurcations, as well as along the inner wall of curves in the coronary arteries.3,4 On the other hand, it is unclear why some plaques remain quiescent for many years, while others progress rapidly. These findings suggests that independently of systemic factors, the presence of local hemodynamic factors such as wall shear stress plays a major role in the generation, progression, and destabilization of atherosclerotic plaques. Various studies have shown that the presence of a normal or increased wall shear stress (≥10-15 dynes/cm²) has a protective effect on the endothelium mediated by inhibition of endothelial proliferation, a local antiinflammatory effect, prevention of apoptosis of endothelial cells, and increased expression and activity of antioxidant enzymes (superoxide dismutase and nitric oxide synthase) in endothelial cells.5 However, reduced wall shear stress, as occurs, for instance, in certain segments of arterial bifurcations, favors oxidation and lipid accumulation in the intima. In fact, an increase in the expression and activity of angiotensin-converting enzyme has been demonstrated in areas with reduced wall shear stress, leading to an increase in the levels of angiotensin II and, consequently, increased oxidative stress.5,6 Likewise, low wall shear stress reduces endothelial production of nitric oxide and antioxidant proteins, and increases the expression of E-selectin and adhesion molecules that favor the recruitment of monocytes and leucocytes to the intima.5,6 In 1969, Caro et al7 demonstrated a correlation between reduced shear stress in the vascular wall and atherosclerosis. Subsequently, numerous studies in coronary, carotid, and aortic vessels have confirmed that the generation and progression of atherosclerotic plaques tends to occur in areas with low wall shear stress.1-4,8,9 Stone et al10 studied the effects of wall shear stress on the progression of atherosclerotic plaques and vascular remodeling in the coronary arteries of 6 patients in whom assessments were made at baseline and 6-month follow-up. In all cases, coronary angiography, intravascular ultrasound, and measurement of coronary blood flow were performed and, using that data, a 3D reconstruction of the artery was generated and the wall shear stress determined. Areas with low wall shear stress (<12.6 dynes/cm²) displayed a significant increase in the thickness of the atherosclerotic plaque and the vessel wall (positive remodeling), areas with physiologic wall shear stress (12.6-26.9 dynes/cm²) did not display significant changes, and areas exposed to a high wall shear stress (≥27 dynes/cm²) displayed positive remodeling of the artery without changes in the atheroma plaque. The importance of that study centers on the fact that it represents the first data in humans to link a dynamic factor such as shear stress in coronary arteries with the subsequent progression of the atherosclerotic plaque and vascular remodeling in the medium term. However, the relationship between wall shear stress and atherosclerotic plaques in the coronary arteries appears to be limited to nonsignificant lesions that, through a phenomenon of positive arterial remodeling, have not yet led to stenosis of the arterial lumen.11 As the atherosclerotic plaque progresses to cause stenosis, the wall shear stress increases, especially in the proximal part of the plaque, at the entrance to the stenotic region. It has been suggested that this increase in the wall shear stress could give rise to a reduction in the fibrous cap of the plaque through a process of apoptosis and, therefore, would favor destabilization and rupture of vulnerable plaques.12 In fact, the areas in which ulceration and rupture of plaques is most common in the coronary and carotid arteries lie proximal to the point of maximum stenosis and coincide with the section of the atherosclerotic plaque subjected to the highest shear stress.12
In the 1990s, the first studies were published in which wall shear stress was measured using magnetic resonance imaging (MRI) and correlated with atherosclerosis in the aorta.8,9 Recently, Wu et al13 succeeded in calculating this hemodynamic parameter in the carotid, femoral, and brachial arteries using MRI. Wentzel et al14 took a step further by using high-resolution MRI to study the interaction between wall shear stress and the progression of atherosclerotic plaques in the descending thoracic aorta. Those authors performed analyses at baseline and 2-year follow-up in 10 dyslipidemic patients treated with simvastatin. Despite the demonstration of a significant reduction in aortic atherosclerotic plaques after 2 years of hypolipidemic treatment, the phenomenon was not dependent upon wall shear stress. That study was the first to evaluate the interaction between atherosclerotic plaque progression and wall shear stress by MRI and is a further demonstration of the potential of the technique for the noninvasive functional and anatomic assessment of atherosclerotic disease.
WALL SHEAR STRESS AND RESTENOSIS FOLLOWING CORONARY STENT IMPLANTATION
Restenosis following implantation of coronary stents is mainly due to a process of neointimal proliferation within and at the edges of the stent. The variables that have been associated with this process include systemic factors, such as diabetes mellitus, and angiographic characteristics such as the length of the stenosis and the diameter of the treated vessel.
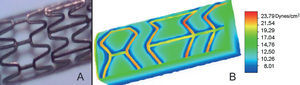
In this issue of Revista Española de Cardiología, Sanmartín et al15 have evaluated the role of a local hemodynamic factor, the wall shear stress, in the extent of neointimal proliferation following stent implantation in the right coronary artery of 7 patients. The methodological complexity of the calculation of wall shear stress makes this study--the fruit of a collaboration between cardiologists and engineers--of particular value, despite the limited number of patients. The calculations of wall shear stress were made using a realistic 3D geometric reconstruction of the artery based on a combination of coronary angiography (2 orthogonal projections following stent implantation) and intravascular ultrasound (automated retrieval of the ultrasound catheter from 4 mm distal to the stent to the aorto-ostial junction). Calculation of the flow conditions was performed using a numerical simulation technique known as the finite volume method. Low wall shear stress was correlated with an increase in neointimal proliferation, with differences in neointimal thickness at 6-month follow-up of up to 20% between the results associated with the highest and lowest values for wall shear stress. This inverse correlation between neointimal proliferation and wall shear stress was observed in both in-stent segments and at the edges of the stent. The results of the study are consistent with those of Wentzel et al,16 who also demonstrated a significant correlation between low wall shear stress and the degree of neointimal proliferation in 14 patients following implantation of self-expanding stents (Wallstent, Schneider AG) in native coronary arteries. It is noteworthy that wall shear stress is not uniform throughout the vascular surface covered by the stent17 and, in fact, is maximal in the stent wires, minimal at the edges of the wires, and intermediate between them (Figure). Carlier et al18 performed an interesting study in animals in which they demonstrated that the variations in in-stent wall shear stress were associated with marked changes in neointimal proliferation. In that study, a device was used that caused a significant increase in the in-stent wall shear stress when positioned inside the stent (antirestenotic diffuser, EP0989830). In the cases in which the antirestenotic diffuser was used, the mean neointimal proliferation was 1.48 mm², significantly less than that observed in stents in which the device was not used (2.36 mm²; P<.01). In addition, that study showed that the reduction of neointimal proliferation was largely due to a reduction of inflammation inside the stent occurring in response to increased wall shear stress. Therefore, alteration of local rheologic factors can have a significant impact on the neointimal response following stent implantation and, consequently, on restenosis. It has also been suggested that certain characteristics of the design and implantation of stents have a significant influence on local hemodynamics and can play a decisive role in the degree of in-stent neointimal proliferation.19 Thus, a reduction in the thickness and number of wires in the stent significantly increases (87% and up to 2.75 times, respectively) the in-stent wall shear stress and would have a protective effect against restenosis. This may partly explain the differences observed in the rates of restenosis between stents with different designs and geometry.20-22 On the other hand, implantation of stents that are oversized in relation to the size of the coronary vessel (stent-vessel ratio ≥1.2) has also been linked to a significant reduction (up to 12 times) in the wall shear stress.19 In agreement with these findings, some clinical studies have revealed a significant correlation between implantation of oversized stents and the incidence of restenosis.23,24 Although it has been suggested that increased arterial damage would be the trigger for an exaggerated intimal response in the case of oversized stents, local hemodynamic changes could also be a factor that favors restenosis in those cases.
Figure.Three-dimensional reconstruction of a stent using a numerical simulation that shows the distribution of in-stent wall shear stress. A: experimental stent (US patent number 6 520 987). B: three-dimensional distribution of the shear stress in the vessel wall and the stent struts. The highest shear stress is seen in the stent wires (>20 dynes/cm2), while the vessel wall at the edges of the wires experiences the lowest shear stress (<10 dynes/cm2). Images obtained in the laboratory of Professor Rosaire Mongrain, Department of Mechanical Engineering, McGill University, Canada.
The use of drug-eluting stents has led to a significant reduction in the incidence of restenosis.25 In the only study in humans that has evaluated the relationship between local hemodynamic factors and neointimal proliferation in drug-eluting stents, Gijsen et al26 reported that the inverse relationship between wall shear stress and neointimal proliferation is maintained in sirolimus-eluting stents, despite the fact that neointimal proliferation is minimal. It remains to be seen whether stent design and implantation technique (both of which influence wall shear stress) have any clinical implications in those cases.
In summary, local hemodynamic factors influence the evolution of atherosclerotic disease and may contribute to explaining the differences in distribution and progression of different atherosclerotic plaques. The presence of a low wall shear stress favors progression of the plaque, while a physiologic shear stress has a protective effect in the vascular endothelium. These local hemodynamic parameters, and in particular, an increase in the wall shear stress, have been suggested to play a role in the generation and destabilization of vulnerable plaques; however, this association still has to be confirmed. Preliminary studies have shown that high-resolution MRI can be used to assess the relationship between the progression of atherosclerotic plaques (in the aorta) and local rheologic factors. This represents a significant step forward for research in this area. Local hemodynamic changes following implantation of coronary stents, and in particular, reduced wall shear stress, contribute to an increase in neointimal proliferation and, therefore, favor restenosis. The design and geometric characteristics of the stent, and the method of implantation influence local rheologic parameters and may play a significant role in the degree of neointimal proliferation and the incidence of restenosis. Finally, despite the minimal neointimal proliferation associated with drug-eluting stents, some preliminary studies indicate that the inverse relationship between wall shear stress and neointimal proliferation is maintained in those cases. Future studies should address the possible clinical implications of these findings in the era of the drug-eluting stent.
Correspondence: Dr. J. Rodés-Cabau.
Quebec Heart Institute. Laval Hospital.
2725, chemin Sainte-Foy. G1V 4G5, Quebec. Canadá.
E-mail: josep.rodes@crhl.ulaval.ca