Keywords
INTRODUCTION
Coronary heart disease is one of the main causes of death in both sexes in industrialized countries.1 However, the risk of dying from this disease has decreased in recent years due to a reduction in incidence, the promotion of secondary prevention measures, and the use of new treatments during the acute phase.2-4
Mortality associated with acute myocardial infarction (AMI), both in the acute phase and in the mid and long term, has been examined in many studies. However most have analyzed observed mortality; very few have measured relative survival (RS), a procedure commonly used in oncological studies. RS is used to compare survival in a study cohort with that expected in the background population.5 The techniques used in examining RS are especially useful when cause-specific death information is inaccurate or unavailable because they provide a measure of excess mortality in a group of patients with a certain disease. RS is therefore one of the most adequate procedures for use in the study of long-term survival.6
Gender differences in mortality, presentation and in the type of medical care received have been reported in AMI.7-9 Mortality in the first 28 days following an AMI is usually higher in women,7,8 but controversy exists as to whether this holds for the mid and long term.
Age, sex, cardiovascular risk factors, coronary history, AMI location, complications, treatments received during hospitalization and after hospital discharge, and the type of hospital where treatment is given are among the variables that may influence early or late mortality following an AMI.10-13
The aims of the present study were to analyze 28-day and 5-year survival in men and women arriving alive at a hospital after a first AMI in Guipuzcoa (Spain), and to examine the prognostic factors that may influence such survival.
METHODS
Design
AMI data for Guipuzcoa are recorded in the IBERICA (Investigación, Búsqueda Específica y Registro de Isquemia Coronaria Aguda) population register, a project started in 1997 in which 8 Spanish regions participate. The identification of hospitalized AMI patients, description of variables, and quality controls have previously been reported in detail.14
Study Population
The study subjects were 1677 patients (1228 men and 449 women) resident in Guipuzcoa with a first AMI, admitted to any private or public hospital in the area, and registered in the IBERICA database. This population register included subjects aged 25 to 74 years in 1997 and 1998, but was extended to include people over 75 years of age in 1999-2000. The estimated mean population (aged 25-74) of Guipuzcoa for the period 1996-1997 was 219 516 men and 223 155 women; for the period 1998-1999 (aged 25+) it was 240 712 men and 258 474 women.
All fatal and non-fatal AMI cases and fatal possible AMI cases, classified according to the MONICA study criteria, were included.15 Cases for which the only information source was the death certificate were excluded, as were those who had suffered a prior AMI and non-fatal possible cases (most of which clinically corresponded to angina). The monitoring of cases from the onset of symptoms to day 28 was undertaken via an active search of the hospitals' clinical records. Life status at 5 years was cross checked using National Death Index data (including a manual check), individual health cards and hospital clinical records.
Explanatory Variables
The following variables were taken into account: period of incidence (1997-1998 and 1999-2000), age (collapsed into 3 age groups: <60, 60-69, and >70 years, corresponding approximately to the tertiles of the age distribution), sex, history of angina, coronary risk factors (diabetes, hypercholesterolemia, hypertension, and smoking), AMI characteristics (location, Killip class on admission, left ventricular ejection fraction [LVEF], exercise test results), hospital complications during the acute phase (severe arrhythmia, post-infarction angina, reinfarction, maximum Killip class during hospitalization), treatment employed during hospitalization and at discharge (angiotensin converting enzyme inhibitors [ACEI], antiplatelet therapy, beta-blockers, early revascularization [thrombolysis within 6 hours of the onset of symptoms and primary angioplasty on the day of infarction]), cardiac surgery, and place of treatment (admittance or not to an intensive care unit [ICU]).
Statistical Analysis
Continuous variables are described as means (standard deviations), and discrete variables as absolute and relative frequencies. c2 analysis was used to test the equality of distributions by age and gender, and ANOVA to test the equality of means. The Levene and Kolmogorov-Smirnov tests were used to check for homoscedasticity and the normality of continuous variables.
Observed survival (OS) was estimated for the acute phase (first 28 days), and OS and RS for the late phase (5 years). Deaths occurring in the acute phase were therefore directly related to AMI, with the expected mortality in the general population virtually nil (thus OS and RS are very similar).
The Kaplan-Meier estimator was used to calculate OS and the log-rank test to assess univariate intragroup differences. Relative survival (with 95% confidence intervals) was calculated using the Hakulinen method,16 employing age- and sex-specific life tables for the general population of the area. This expresses the probability of AMI survival after adjustment for competing causes of death, and was estimated as the ratio of the OS to the expected survival of the corresponding general population.5
Mortality and population tables in the 1995-2000 and 2001-2005 periods, stratified by age (single year) and sex, were obtained from the Basque Statistics Institute for Guipuzcoa.17
Data analysis showed a very different behavior of the cardiovascular event in the first 28 days compared to the rest of follow-up (from 29 days to 5 years). Since the usual proportional hazard assumption was violated for the whole of the follow-up period, it was decided to study each period separately. All variables were considered for multivariate analysis, except for treatments received at hospital discharge; these were excluded from analysis of the first 28 days due to the high intrahospital mortality observed.
For the acute phase, a Cox proportional hazards model was used to study the effects on risk of the different covariates considered. The Akaike information criterion (AIC) was used as a covariate exclusion criterion. The models satisfied (P>.150) the proportional hazards hypothesis; this assumption was verified using the test based on Schoenfeld residuals.18
For the period from 29 days to 5 years, a multivariate model was constructed from the generalization for RS of the proportional hazards model proposed by Andersen.19 The test proposed by Stare was used to verify the hazards proportionality hypothesis20 (P>.250). The AIC was again the covariate exclusion criterion used.
All analyses were performed using STATA 10 and R 2.6.2 (Relsur package21) software. Ninety-five percent confidence intervals were calculated for hazard ratios. Significance was set at P<.05.
RESULTS
Explanatory Variables
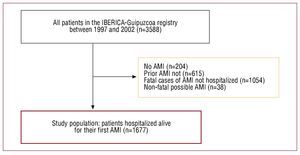
The number of cases included between 1997 and 1998 was 581 (80.7%) men and 139 (19.3%) women; 647 (67.6%) men and 310 (32.4%) women were included in 1999-2000 (Figure 1). The mean age at disease occurrence was significantly higher (P<.01) in women (65.7 [8.98] and 74.43 [12.45] years in the first and second periods, respectively) than in men (58.5 [10.70] and 64.1 [13.33] years, respectively). Table 1 shows the distribution by sex and age group of the baseline characteristics of study patients. Women smoked less in all age groups. From 60 years of age, more women had diabetes and suffered hypertension, and had poorer LVEF and exercise test results. In addition, a greater proportion of diagnostic tests were not performed in women. In the intermediate age group, women more often presented with Killip class III-IV (9.5% vs 17.2%). In the group over 69 years of age, women were admitted less frequently to an ICU (84.0% vs 70.5%), less commonly underwent an early revascularization procedure, and were less often prescribed antiplatelet treatment at discharge. In both sexes, fewer therapeutic resources were used in older than in younger patients. The sex-associated differences that remained significant after adjusting for age were history of diabetes, hypertension and smoking, exercise test results, global contractility, and treatment in an ICU. Significant differences were also seen in terms of hypercholesterolemia and heart surgery (data not shown).
Figure 1. Selection of patients from the Guipuzcoa IBERICA registry. AMI indicates acute myocardial infarction; IBERICA, Investigación, Búsqueda Específica y Registro de Isquemia Coronaria Aguda.
Observed and Relative Survival
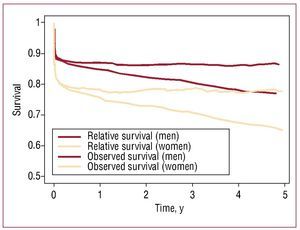
Overall, 229 patients (144 men and 85 women) died within the first 28 days following their AMI; 445 patients (288 men and 157 women) had died at 5 years. Figure 2 shows the overall OS and RS in men and women. During the acute phase of disease, overall OS was higher in men (88.3% vs 81.1%) (Table 2). In the late phase, overall OS and RS was also higher in men (76.5% vs 65% and 86.4 vs 77.6%, respectively). By age group, women under 60 years of age enjoyed greater survival than men at 28 days (P<.05), while in the other 2 groups survival was poorer in women, although with significant differences only for the intermediate age group (P<.05). Men aged 60-69 years and over 69 years of age enjoyed significantly higher long-term RS than women in the same age groups (85.0% vs 77.2% and 74.9 vs 71.4%, respectively). However, when only those patients alive on day 29 were taken into account, differences were seen only for the group under 60 years of age, with a greater risk of death in women (HR, 3.37; 95% CI, 1.29-8.84) (Figure 3). OS and RS at 28 days and 5 years decreased with increasing age in both men and women. Moreover, in all age groups, long-term RS curves showed a high probability of death during the early phase of AMI, followed by a subsequent lower probability of mortality (Figure 3).
Figure 2. Observed and relative survival curves following a first AMI by sex, IBERICA-Guipuzcoa 1997-2000.
Figure 3. Relative survival curves at 5 years (left) and from day 29 to 5 years (right) following a first AMI, by age and gender (IBERICA-Guipuzcoa 1997-2000). Men: red; women: beige.
Multivariate Analysis of Survival in the Acute and Late Phases
Table 3 shows the results of the multivariate analysis by sex, referring to OS in the acute phase of AMI and RS at 5 years, in 1448 patients alive on day 29 after an AMI (1084 men and 364 women).
During the acute phase, variables independently related to a greater risk of death in men included the LVEF, a maximum Killip class during hospitalization of ≥III (HR, 3.01; 95% CI, 1.77-5.14), and the presence of severe arrhythmia (HR, 2.94; 95% CI, 2.02-4.27). Inferior (HR, 0.62; 95% CI, 0.41-0.93) and non-Q wave AMI (HR, 0.41; 95% CI, 0.19-0.86), the use of beta-blockers (HR, 0.36; 95% CI, 0.20-0.65) and ACEI at the hospital (HR, 0.38; 95% CI, 0.25-0.57), and early revascularization (HR, 0.45; 95% CI, 0.28-0.75) were associated with a lower risk of death. In women, the variables associated with a greater risk of death were severe arrhythmia (HR, 3.10; 95% CI, 1.94-4.95) and a maximum Killip class during hospitalization of ≥III (a 3-fold greater risk compared to women with a Killip class With respect to long-term relative survival, an AMI diagnosis during the 1997-1998 period and a Killip class of ≥III on admission were found to be predictive of a greater excess risk of death in men, whereas age over 69 years (HR, 0.42; 95% CI, 0.26-0.69), hypercholesterolemia (HR, 0.56; 95% CI, 0.36-0.87) and use of beta-blockers after hospital discharge were related to a lower excess risk. In women, treatment with ACEI during hospitalization (HR, 1.84; 95% CI, 1.11-3.05) was related to a greater excess risk of death. In contrast, age >69 years (HR, 0.18; 95% CI, 0.07-0.45) and admission to the ICU (HR, 0.45; 95% CI, 0.27-0.76) were associated with a lower excess risk. Men with no exercise test results and women with an AMI of a mixed or non-codable location had poorer prognosis. DISCUSSION Similar to that seen in other studies, in the present registry women experienced a first AMI at an older age, were more likely to suffer diabetes and hypertension and smoked less, compared to men. In addition, they had a more unfavorable initial clinical profile, developed more complications in the acute phase, and from 69 years of age received fewer treatment resources than men.22-24 The interaction between sex and age is clear from the separate models. In the full adjusted models (for acute and long-term follow-up), and after adding the sexage iteration variable, the results were strongly significant (P<.01) (data not shown). While a very extensive literature exists regarding AMI, it is complicated to compare the present results with those of other studies due to the substantial differences in the definition of cases, study populations, research period, baseline characteristics of the patients, and analytical approach. Indeed, differentiated multivariate models for men and women are not common. In the present work, men aged 60 years or older enjoyed greater survival than women of a similar age in both the acute phase and the entire period considered. From 29 days to 5 years, however, sex-based differences were only seen in the younger age group, with a greater RS in men. This effect of sex on survival by age group is similar to that reported by Vaccarino et al.25 in a study in which women under 60 years of age also showed greater long-term mortality. Excess mortality in the acute period has also been reported in women, but if they overcome this phase, their survival is similar to that of men.23 Several factors that might be associated with greater early mortality in women, including the occurrence of an AMI at a later point within each age group, greater comorbidity and clinical complications in the acute phase and treatments less compliant with clinical practice guidelines.7,12,26 The differences found in the older age group between OS and RS at 5 years are due to overall mortality, which is also higher at such ages. In addition, the difference between OS at 28 days and RS at 5 years is lower than the difference seen between the OS in those same periods (1.9% vs 11.8% in men, and 3.5% vs 16.1% in women). This suggests that the estimation of RS affords advantages for long-term analysis, providing a closer-to-reality view of the unique effect of this disease on survival. However, this statistical method has been little used to date for the study of coronary heart disease.5,27 The factors related to OS in the first 28 days and to RS from day 29 to 5 years were not the same in both sexes. This might indicate that AMI is different in men and women, something that has been suggested by several authors.26,28 During the acute phase, the factors independently associated with a lower or higher survival in men were those reported in most studies.10,12,29 In women, factors associated with reduced survival were found, but no variable was identified that related to an improved prognosis. This may be partly due to the relatively low number of women enrolled in the study. As a result, small differences in the variables studied may not have become statistically significant and were therefore not included in the multivariate model. In addition, more men than women participate in clinical trials, and therapeutic indications are therefore mainly based on results obtained in men. However, these differences do not explain why early revascularization has no influence on the survival of women in the acute phase. In the late phase, age is associated with a lower excess risk of death in both sexes. The group over 69 years of age shows the best prognosis, in contrast with the findings of other studies in which OS or mortality have been analyzed.4,30 This might be explained by the higher all-cause mortality in older groups; thus, people who experience an AMI after 69 years of age are at lower risk of dying from this cause than those who suffer an AMI before 60 years of age. A lower excess risk of death related to hypercholesterolemia was seen in men. Although the reasons for this unexpected result remain unclear, it has been described that the treatment received by these patients might be the reason.31,32 The association found between beta-blocker treatment at discharge and long-term survival has been reported in other studies.13,33 The fact that only women showed a lower excess risk of death associated with ICU admission suggests that, since the great majority of men were treated in an ICU, this variable cannot discriminate different risk levels in men, but can in women. The increased risk of death seen in women who were treated with ACEI during their hospital stay is also difficult to explain, particularly when in this same series of patients ACEI treatment was a protective factor in men during the acute phase. A possible explanation might be that women who were treated with ACEI at the hospital had a poorer clinical condition (higher grade of left ventricular dysfunction and a poorer Killip class during hospitalization) than those who were not prescribed ACEI. This increase in the long-term risk of death related to treatment with ACEI during and after hospitalization has been reported in other studies.13,33 Men diagnosed in the first period (1997-1998) had a higher excess risk of death than those diagnosed in the second period (1999-2000), which may be related to improvements in treatment over time, though it is difficult to assume that such improvements only affect men. Early revascularization virtually reached statistical significance in men, with the interval strongly deviated to the left, which appears to indicate that an effect exists. In both sexes, variables associated with poorer survival both in the acute period and in the long term were identified. The greatest risk of death was seen in patients for whom such variables were classified as unknown/not done/other, owing to their poorer baseline clinical condition. Determination of the LVEF and exercise testing are usually performed in patients in a stable clinical condition. Variables classified as unknown, such as the Killip class at admission, were seen in men who died in the first 28 days. One of the main characteristics of the present study is that it uses the RS method with AMI. The analysed data came from a population registry of AMI events in which quality controls are in place,14 thus guaranteeing data reliability and validity. It is therefore unlikely that selection or information bias occurred. The study population consisted of all subjects living in the selected geographic area who met the inclusion criteria and attended a hospital in that area. All potential confounders based on the information from the IBERICA registry were included in the multivariate models. However, other potential confounding variables such as socioeconomic class or statin therapy could not be included because they were not recorded. Therapeutic compliance or potential changes in treatment after hospital discharge were also unknown, as no active follow-up was undertaken. The homogeneous population and the lower sample size of women may have influenced the results obtained. In addition, diagnostic and treatment strategies may have changed from the study period to the present. In the future, further analyses could be performed for a longer time period or for a wider study area, so that a larger number of women with AMI can be studied. CONCLUSIONS Most mortality in patients with an AMI occurs in the acute period of the disease. An interaction between sex and age that influences survival after an AMI was detected. The estimation of RS and differential analysis of prognostic variables in men and women provide an increased understanding of AMI in our area. Different prognostic factors were found in men and women which may be useful for more specific identification of patients at higher risk. However, the small number of women in the present study might have impaired the identification of some of the prognostic factors associated with AMI in this group. These findings highlight the need to include a larger number of women in clinical trials if we are to better understand the treatments most suited to them. ACKNOWLEDGMENTS The authors thank all those involved in the collection of information, particularly to M. Cres Tobalina of the Public Health Department of Alava for providing cases from the Alto Deba area. ABBREVIATIONS Correspondence: Dr. M. Basterretxea. Received August 7, 2009.
ACEI: angiotensin-converting enzyme inhibitor
AMI: acute myocardial infarction
IBERICA: Investigación, Búsqueda Específica y Registro de Isquemia Coronaria Aguda (Acute Ischemic Heart Disease Research, Specialized Literature Search and Registry)
ICU: intensive care unit
LVEF: left ventricular ejection fraction
OS: observed survival
RS: relative survival
Avenida de Navarra, 4. 20013 San Sebastián. Guipúzcoa. Spain.
E-mail: epidem1-san@ej-gv.es
Accepted for publication January 20, 2010