Keywords
INTRODUCTION
For the fifth consecutive year, the Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias is publishing the Spanish Catheter Ablation Registry for ablation procedures done in 2005. The registry includes data from most of the catheterization laboratories in Spain.
METHODS
Data were collected either retrospectively by filling out of a form sent to all catheterization laboratories or prospectively through use of a common database. This method was similar to that used for previous registries.1-4
Ten substrates were analyzed, as in previous registries: atrioventricular nodal reentry tachycardia (AVNRT), accessory pathways (AP), atrioventricular node (AVN), focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia related to postmyocardial infarction scarring (VT-AMI), and ventricular tachycardia associated with heart disease and not related to postmyocardial infarction scarring (VT-NAMI). The variables analyzed for each substrate were number of patients and procedures performed, number of successful procedures, type of catheter used for ablation, type of complications, and periprocedural deaths. In addition, some substrate specific variables were analyzed such as AP location, FAT and MAT location, type of IVT, and type of VT-NAMI.
As in previous registries, the acute outcome (success or failure) was assessed; we did not analyze the subsequent course and so we have no data on recurrence. Complications were counted during the period in hospital after the procedure. Nevertheless, significant complications reported during the days after discharge from hospital were also considered.
In the ablation procedures for AF and VT-AMI, acute success or failure could not be fully assessed due to the type of information collected in the forms of the registry. The type of approach or the aims in the two substrates may vary according to catheterization laboratory. Thus, AF ablation may be treated by isolating pulmonary vein or by circumferential ablation with or without ablation lines in the mitral annulus and/or the posterior left atrial wall, or by electrogram-guided ablation.5,6
Ablation of VT-AMI can be done by mapping during VT or in the underlying rhythm of the patient, with the aim of reducing potentials or of block of slow isthmus conduction detected with an intracardiac nonfluoroscopic intracardiac navigation system.7,8 This all suggests that the criterion for acute success or failure may vary from laboratory to laboratory, and so the current registry will not discuss this variable and these data will not be included in the overall assessments.
The percentage of successful outcomes will therefore be calculated using 5504 procedures as the denominator, but the percentage of complications will be calculated with respect to all the ablation procedures.
Statistical Analysis
Quantitative variables are expressed as mean (SD). Qualitative variables and proportions were analyzed with the χ² test and Fisher test when necessary. Quantitative variables were analyzed with the Student t test. The percentages of successful procedures and procedures with complications were calculated with respect to the number of procedures. P values less than .05 were considered statistically significant. The statistical analysis was performed with the statistical software SPSS 12.0.
Data on human resources are presented only for centers with public funding because these variables in private hospitals could be attributed to factors beyond the scope of this registry. The epidemiological variables correspond to 1345 patients with a single ablation procedure during 2005 in the hospitals that provided prospective data (n=11). None of these centers treated pediatric patients.
RESULTS
In total, 47 centers responded, representing an increase in the number of centers with respect to previous registries.1-4 The characteristics of the participating centers are shown in Table 1 and the distribution of these centers throughout Spain is presented in the list of registry participants. Only 1 hospital treated exclusively pediatric patients. One center started its activity on December 14, 2005, and provided data from 5 ablation procedures only, and so the results of the ablation procedures for this center were excluded from the analysis.
Retrospective data was provided by 76.6% (n=36) of the centers.
Epidemiological Variables (Table 2)
The youngest patient group corresponded to those who underwent AP ablation (39 [16] years), whereas those who required AVN ablation were the oldest (69 [9] years). Atrioventricular nodal reentry tachycardia ablation was done primarily in women (71%), whereas AF ablation was much more common in men (90%).
In total, 19% of the patients suffered some kind of heart disease, 11 out of every 100 patients had left ventricular systolic dysfunction, and 1 out of every 100 had an implantable cardioverter defibrillator (ICD). These characteristics were reported more often in patients who underwent VT ablation.
Infrastructure and Resources
The information on the resources of catheterization laboratories in the hospitals of the registry are shown in Table 3. Most laboratories (66%, n=31) had at least 1 nonfluoroscopic intracardiac navigation system, 8 laboratories had 2 nonfluoroscopic intracardiac navigation systems and 2 had 3. The distribution of types of device was as follows: 16 centers had CARTO® systems, 12 had LOCALISA® systems, 9 had NavX® systems and 4 had RPM® systems. In addition, 8 laboratories offered intracardiac echocardiography.
Human resources in the publicly funded hospitals are listed in Table 4. Two or more staff physicians worked full-time in the catheterization laboratory in 69% of the centers (29/42). Sixteen centers (38%) also had student doctors.
Overall Results
The total number of ablation procedures undertaken by the 46 centers was 6157 (excluding the center that did only 5 ablation procedures), which corresponds to 133 (85) procedures per center (median, 129; range, 13-489).
Figure 1 shows the distribution of the number of procedures per laboratory.
Figure 1. Number of catheterization laboratories in the Spanish Registry classified by number of catheter ablation procedures in 2005.
The overall percentage of successful procedures was 92.7% (5104/5504 procedures). The mean number of successful procedures per center was 93% (8%) (median, 93%; range, 84-100). The overall percentage of major complications was 1.05% (n=65) and the mortality rate was 0.03% (2 patients). The data are similar to previous years.1-4 Two patients died during 2005, one after CTI ablation and the other after VT-AMI ablation. The first patient died after a massive cerebrovascular accident (CVA). Detailed information on the second is not available.
Results by Substrate
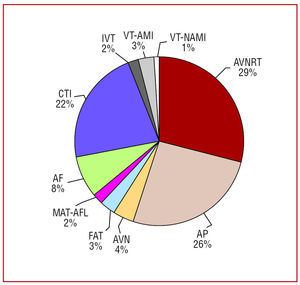
The substrate most frequently ablated (as in previous registries) was AVNRT, followed by AP and CTI (Figure 2). An increase in AF ablation, which now accounts for 8% of all procedures (Figure 3), can be seen compared to previous registries. Table 5 shows the distribution of substrates by center after exclusion of the center that only did 5 procedures and the pediatric hospital. The following substrates were ablated: AVNRT (8%), AP (86%), and focal atrial tachycardia (FAT) (6%).
Figure 2. Relative frequency of different substrates treated by catheter ablation in Spain in 2005. AF: atrial fibrillation; CTI: cavotricuspid isthmus; AVN: atrioventricular node; FAT: focal atrial tachycardia; MAT-AFL: macroreentrant atrial tachycardia/atypical atrial flutter; AVNRT: atrioventricular nodal reentry tachycardia; IVT: idiopathic ventricular tachycardia; VT-AMI: ventricular tachycardia related to postmyocardial infarction scarring; VT-NAMI: ventricular tachycardia not related to postmyocardial infarction scarring; AP: accessory pathways.
Figure 3. Relative frequence of different substrates treated since 2001. AF: atrial fibrillation; CTI: cavotricuspid isthmus; AT: atrial tachycardia; AVNRT: atrioventricular nodal reentry tachycardia; VT: ventricular tachycardia; AVN: atrioventricular node; AP: accessory pathways; AT: atrial tachycardia.
The mean number of different substrates treated in the same center (excluding the pediatric center and the center that did only 5 procedures) was 7.9 (1.8) (median, 8; range, 4-10). Eleven centers (24%) treated all types of substrate analyzed. All centers did AVNRT, AP and CTI ablation (Figure 4). The other substrates were not treated in all centers. Due to the nature of the study, we do not have sufficient information to analyze the variables that might influence why a catheterization laboratory treats or does not treat a given substrate.
Figure 4. Number of catheterization laboratories included in the Spanish registry that treat the indicated substrates. CTI: cavotricuspid isthmus; AF: atrial fibrillation; AVN: atrioventricular node; FAT: focal atrial tachycardia; MAT: macroreentrant atrial tachycardia; AVNRT: atrioventricular nodal reentry tachycardia; VT-AMI: ventricular tachycardia related to postmyocardial infarction scarring; VT-AMI: ventricular tachycardia not related to postmyocardial infarction scarring; AP: accessory pathways.
Figure 5. Percentage of successful catheter ablation procedures by substrate since 2002. CTI: cavotricuspid isthmus; AVN: atrioventricular node; AT: atrial tachycardia; AVNRT: atrioventricular nodal reentry tachycardia; AP: accessory pathways.
Figure 6. Percentage of major complications in catheter ablation procedures by substrate since 2002. AF: atrial fibrillation; CTI: cavotricuspid isthmus; AVN: atrioventricular node; FAT: focal atrial tachycardia; AVNRT: atrioventricular nodal reentry tachycardia; VT: ventricular tachycardia; AP: accessory pathways.
The mean success and complication rates are presented by substrate in Tables 6 and 7. The outcomes were similar to those reported in previous years.
Atrioventricular Nodal Reentry Tachycardia
All centers treated AVNRT at least once. A total of 1792 ablation procedures were undertaken (39 [25] per center; range, 3-148). The number of successful procedures was 1759 (98.1%). A total of 8 major complications occurred (0.4%), with atrioventricular (AV) block occurring in 5 cases (4 were permanent and required a pacemaker and 1 was transient). No deaths were reported. A standard catheter (that is a radiofrequency catheter with a 4-mm tip) was not used in 22 procedures. The nonstandard catheters used were 2 8-mm catheters, 1 irrigated tip catheter, and 19 cryoablation catheters were.
Accessory Pathways
A total of 1591 AP ablation procedures were performed (34 [19] per center; range, 2-99). Success was achieved in 1455 procedures (91.4%) and major complications occurred in 20 (1.2%). As in previous registries, arterial c omplications were the most common type of complication (0.95%). In 4 cases, significant pericardial effusion occurred, and in 3 cases, AV block was reported that did not require permanent pacemaker implantation. In 128 procedures, a standard catheter was not used (26 8-mm catheters, 75 irrigated tip catheters, and 27 cryoablation catheters). The most common site for AP ablation was the left free wall (53%). The success rate varied according to site, thus, the success rate was 93% for AP ablation of the left free wall, 92% for ablation of the right free wall, 87% for inferior septal ablation, and 86% for ablation around the His bundle and the superior septum.
Cavotricuspid Isthmus
Only the pediatric center did not perform CTI ablation procedures. Overall, 1378 procedures (30 [19] per center, range 3-81) were done. Success was achieved in 1291 procedures (93.7%) and major complications occurred in 8 (0.6%). One patient died after CVA. Of the 1247 procedures for which information on the type of catheter used is available, 1230 (98.6%) did not use the standard type. Of these nonstandard types, 844 (68.6%) were 8-mm tip catheters, 353 were irrigated tip (28.7%), and 33 were cryoablation catheters (2.7%).
Atrioventricular Node Ablation
Overall, 246 procedures were performed in 39 centers (6 [5] per center; range, 1-25). Success was achieved in 239 procedures (97.1%) and major complications occurred in 2 (0.8%), corresponding to pacemaker malfunction and an undefined complication.
Focal Atrial Tachycardia
Overall, 39 centers treated FAT (189 procedures; 4.5 [3.5] per center; range, 1-20); 149 procedures were successful (78.8%) and 2 major complications were reported--CVA and pericardial effusion. Of the 124 procedures with a nonstandard catheter, 11 used 8-mm tip catheters, 11 used irrigated tip catheters, and 2 used cryoablation catheters. The FAT site was documented in 170 procedures: 151 (89%) in the right atrium and 19 (11%) in the left atrium. The success rate was 81.5% and 68%, respectively.
Macroreentrant Atrial Tachycardia/Atypical Atrial Flutter
A total of 101 procedures treated MAT/atypical atrial flutter out in 23 centers (4.3 [4.3] per center; range, 1-18). Of these, 66 procedures were successful (65.3% centers), and arterial complications were reported in 2. In the 90 procedures with information on the type of catheter, nonstandard catheters were used in 56 (62%). Of these, 30 were irrigated tip and 26 were 8-mm tip. In 86 procedures, information on the location of the tachycardia is available: 41 in the right atrium (48%) and 45 in the left atrium (52%), with a success rate of 73% and 53%, respectively.
Atrial Fibrillation
In total, 480 AF procedures were done in 24 centers (20 [24] per center; median, 13; range, 1-106). Eighteen centers reported the outcome of 352 procedures (73% of the procedures done). Complications occurred in 29% (6%), the most frequent being significant pericardial effusion (n=17), followed by vascular complications (n=6). Two patients suffered CVA (0.4%) and 3 episodes of arterial ischemia were reported. Only one instance of pulmonary vein stenosis occurred. The type of ablation was reported in 427 procedures: 259 were circumferential ablations, 167 corresponded to ostial isolations, and a right atrial ablation was done once. A nonstandard catheter was used in 407 procedures, that is, 95% of the 452 procedures with information on the type of catheter available. Irrigated tip catheters were used in 243 procedures and 8-mm tip catheters in 164.
Idiopathic Ventricular Tachycardia
A total of 149 IVT procedures were carried out in 40 centers (3.5 [2.7] per center; range, 1-13). In total, 138 procedures were analyzed with success reported in 109 of these (79%). No complications were reported. The type of VT was reported in 131 procedures: 79 were located in the right ventricular outflow tract, 23 in the left ventricular outflow tract, 22 were fascicular, and 7 were IVT with some other location. The overall success rates for these types of VT were 71%, 69.5%, and 71%, respectively.
Ventricular Tachycardia Related to Postmyocardial Infarction Scarring
In total, VT-AMI was treated in 173 procedures in 32 centers (4.7 [4.4] per center, range, 1-22). Three major complications were reported (1.7%). One patient died after the ablation procedure. In the 156 procedures with information on the type of approach, 111 corresponded to conventional ablation and 45 to a substrate approach. Of the 158 procedures with information on the type of catheter, 102 (64.5%) used a nonstandard catheter, 80 an 8-mm tip catheter, and 22 an irrigated tip catheter.
Ventricular Tachycardia Not Related to Postmyocardial Infarction Scarring
A total of 67 VT-NAMI procedures were carried out in 23 centers (3 [3.5] per center; range, 1-14). Of the 53 procedures with outcome data available, 36 were successful (68%), and only 1 major complication (1.5%) was reported (AV block). Thirteen ablation procedures were reported in patients with right ventricular arrhythmogenic dysplasia with a success rate of 61.5% (n=8). Success was achieved in the 6 patients with bundle-branch reentrant VT. Success was also achieved in 13 of the 20 patients (65%) with VT and with nonischemic dilated cardiomyopathy. A nonstandard catheter was used in 29 of the 53 procedures reported (55%), 17 with an 8-mm tip and 12 with an irrigated tip.
DISCUSSION
The registry this year has collected data on more procedures (over 6000) and enjoyed stronger participation (47 centers), thus breaking the downward trend in terms of centers and procedures in previous registries (Figure 7).
Figure 7. Number of ablation procedures analyzed and number of centers with data analyzed since 2001.
The techniques used have changed greatly since 2001.1 In the first ablation registry, 11 centers had at least 1 nonfluoroscopic intracardiac navigation system compared to 31 in 2005. In 5 years, the number of centers with intracardiac ultrasound has doubled. Only 1 center performed cryoablation in 2001 compared to 11 in 2005.
However, the number of physicians working full-time in the catheterization laboratories of publicly funded hospitals has remained stable over these last 5 years (1.6 in 2001 and 1.7 in 2005). This contrasts with the progressive increase in the number of ablation procedures per laboratory (106 in 2001 and 133 in 2005) and with an increase in the percentage of laboratories that do ICD implantation (56% in 2001 vs 72% in 2005) and pacemaker implantation. As in previous years, the laboratories with 2 or more full-time physicians carry out more ablation procedures (167 [92] vs 81 [54]; P<.01). In addition, these centers more often have a laboratory dedicated only to these procedures (93% vs 67%, P<.05) and have more nonfluoroscopic intracardiac navigation systems (82% vs 44%, P<.05).
The distribution of substrates differs substantially from previous registries: in 2005 AF ablation accounted for 8% of the ablation procedures compared to 3% in preceding years. A variety of factors might contribute to this difference, such as the greater number of centers that perform this type of ablation (12 in 2004 vs 24 in 2005) and the addition of centers with a larger number of procedures (3 centers with more than 50) although most (n=16) did not do more than 20 AF ablation procedures.
In the 2002 registry, we reported that the "The proportion of VT ablation has stabilized at 6% to 7%, though this figure may rise in coming years due to the more extended use of nonfluoroscopic intracardiac navigation systems and treatment of unmappable VT." Time does not seem to have confirmed our prediction, despite the increased use of nonfluoroscopic intracardiac navigation systems. In 2001, 125 ablation procedures were done for AVNRT, 125 for VT-AMI, and 48 for VT-NAMI (298 in total, 7% of all procedures); in 2005 these numbers were 140, 173, and 67, respectively (380 in total, 6% of all procedures). The number of laboratories that do VT-AMI ablation was 16 in 2001, 32 in 2005 (31 in public hospitals with a mean of 3 procedures per center), which contrasts with the 80 centers (68 of which were public hospitals) that implanted ICD in 2004.9
In these 5 years, we have not observed significant variations in terms of overall success or success according to substrate treated. The substrates that are most frequently treated are those that have a higher success rate. Given the nature of the registry, we have been unable to analyze any of the variables that might affect outcome. Likewise, we have not observed large differences in the percentage of complications. Atrial fibrillation ablation remains the type of ablation with the largest rate of complications (particularly pericardial effusion), probably because of the technique used which requires transseptal puncture and radiofrequency application in the left atrium.
Year after year, mortality has been less than or equal to 1 death for every 1000 patients treated and is almost always associated with substrates that have a higher incidence of structural heart disease and old age (AVN, VT-AMI, CTI ablation).
CONCLUSIONS
In the fifth catheter ablation registry of Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias, we have analyzed more than 6000 ablation procedures thanks to a notably stronger participation of catheterization laboratories in Spain.
The results reflect an increase in the proportion of AF ablation procedures and a stable success rate for most of the substrates treated (>90% for the most frequently treated arrhythmias) with few complications.
On average, fewer than 2 full-time physicians are available in publicly funded catheterization laboratories, even though daily activity is growing (number and complexity of ablation procedures, device implantations, etc).
Catheterization Laboratories By Autonomous Region and Province That Participated in the Spanish National Catheter Ablation Registry in 2005 (Fully Private Hospitals Shown in Italics)
ANDALUSIA. Cádiz: Hospital Puerta del Mar; Granada: Hospital Virgen de las Nieves; Huelva: Hospital Juan Ramón Jiménez; Malaga: Hospital Virgen de la Victoria; Seville: Hospital Virgen de Macarena, Hospital Virgen del Rocío, Hospital Virgen de Valme. ARAGON. Zaragoza: Hospital Lozano Blesa, Hospital Miguel Servet. ASTURIAS. Hospital Central de Asturias. BALEARIC ISLANDS. Hospital Son Dureta. CANARY ISLANDS. Las Palmas de Gran Canaria: Clínica San Roque; Tenerife: Hospital Nuestra Señora de la Candelaria, Hospital Universitario de Canarias. CANTABRIA. Hospital Marqués de Valdecilla. CASTILE-LA MANCHA. Toledo: Hospital Nuestra Señora del Prado, Hospital Virgen de la Salud. CASTILE-LEÓN. León: Hospital de León; Salamanca: Hospital Clínico Universitario; Valladolid: Hospital Clínico Universitario; Hospital Río Hortega. CATALONIA. Barcelona: Hospital de Bellvitge, Hospital del Mar, Hospital Clínico, Hospital Valle de Hebrón, Hospital Santa Cruz y San Pablo, Hospital Germans Trias i Pujol, Hospital San Juan de Dios, Centro Cardiovascular San Jordi. VALENCIA AUTONOMOUS REGION. Alicante: Hospital Universitario de Alicante; Valencia: Hospital General de Valencia. GALICIA. La Coruña: Hospital Clínico de Santiago de Compostela, Hospital Juan Canalejo. MADRID. Clínica Puerta de Hierro, Hospital 12 de Octubre, Fundación Hospital de Alcorcón, Hospital Clínico San Carlos, Hospital Gregorio Marañón, Hospital de Getafe, Hospital Severo Ochoa, Hospital La Paz, Clínica USP San Camilo. MURCIA. Hospital Virgen de la Arrixaca. NAVARRE. Clínica Universitaria de Navarra; Hospital de Navarra. BASQUE COUNTRY. Bilbao: Hospital de Basurto, Hospital de Cruces.
List of Physicians Responsible for the Data from Each Center of the Spanish Catheter Ablation Registry in 2005
Dr. J Alzueta, Dr. M.F. Arcocha, Dr. A. Arenal, Dr. A. Asso, Dr. R. Barba, Dr. N. Basterra, Dr. A. Berruelo, Dr. A. Bodegas, Dr. J. Brugada, Dr. L. Cano, Dr. E. Castellanos, Dr. S. del Castillo, Dr. E. Díaz-Infante, Dr. M.C. Expósito, Dr. M.L. Hidalgo, Dr. I Fernández-Lozano, Dr. A. García-Alberola, Dr. E. García-Morán, Dr. A. Grande, Dr. B. Herreros, Dr. J. Jiménez-Candil, Dr. M. López-Gil, Dr. A. Macías, Dr. J. Martí, Dr. J.G. Martínez, Dr. J.L. Martínez-Sande, Dr. D. Medina, Dr. J.L. Merino, Dr. A. Moya, Dr. V. Palanca, Dr. N. Pachón, Dr. A. Pastor, Dr. L. Pérez-Álvarez, Dr. N. Pérez-Castellano, Dr. A. Pedrote, Dr. G. Rodrigo, Dr. A. Rodríguez, Dr. F.J. Rodríguez Entem, Dr. E. Rodríguez-Font, Dr. R. Romero, Dr. A. Rubio, Dr. X. Sabaté, Dr. L. Tercedor, Dr. A. Vázquez, and Dr. F. Wanguermer.
*A list is presented at the end of the physicians who participated in the 2005 Spanish Catheter Ablation Registry.
Correspondence: Dr. M. Álvarez López.
Unidad de Arritmias. Servicio de Cardiología.
Hospital Universitario Virgen de las Nieves.
Avda. de las Fuerzas Armadas, 2. 18014 Granada. España.
E-mail: malvarez@secardiologia.es