Keywords
INTRODUCTION
The Spanish Registry of Pacemakers, known as the Banco Nacional de Datos de Marcopasos (BNDM) in Spanish,1 regularly publishes information on the most relevant characteristics of cardiac pacing in Spain and maintains a similar structure in its publications.2-9 The BNDM also submits a summary of the data generated to the European Pacemaker Registry.10,11 The first official report was published in the Revista Española de Cardiología in 1997,2 and presented changes in pacemaker practice since 1994. Even though data collection started in1994, not all information is available in its entirety due to the successive improvements in the software used with the database, the application for extracting information, and the extent of information collected.
Detailed information from 1999 onwards is available on the web site of the Working Group on Cardiac Pacing (www.marcapasossec.org).
The current report presents data corresponding to 2009, with reference only to specific aspects that have changed in the last 10 years in order to improve the clarity of the figures. The report provides information on the quality of pacing and the extent to which it complies with current clinical guidelines in its different indications.12,13
METHODS
The information processed and analyzed is derived from different sections of the European Pacemaker Patient Identification Card (EPPICard). A copy of this card is generated and submitted to the registry. The card is sent from the hospitals where the pacemakers are implanted or from the companies involved, in accordance with the legislation on implantable devices.
Another option is electronic submission or use of the databases of the sites themselves, provided they include at least as much information as that gathered from all fields of the EPPICard and the data privacy guidelines required by the Data Privacy Law are respected. Alternatively, data could be extracted from the dedicated database developed by the Working Group on Cardiac Pacing.8 The aim is to facilitate submission of data, but a substantial improvement has not been observed. Currently, another route is being developed: direct submission via the web, to automate and homogenize the process of data collection in order to extend the reach of the registry.
The data received are checked by graduate nurses, who are regular collaborators with the registry, and processed by a specific program with the collaboration of the IT Department of the Spanish Society of Cardiology.
Given that not all data from all pacemakers used in the year are submitted, the calculation of the number of units used throughout Spain and in each autonomous region is performed with the regular collaboration of the Spanish distribution companies. These companies not only provide this information to the BNDM and but also to the European Confederation of Medicals Suppliers Associations (Eucomed), and small variations are always observed.
The population data for the year are extracted from the report issued and regularly updated by the Spanish Institute of Statistics (INE) (www.ine.es).
Sample Analyzed
A total of 11 939 cards were processed, corresponding to implants or replacement of pacemaker generators submitted by 106 public and private hospitals (Table). This accounts for 35% of all generators, a similar percentage to previous years.
The following results correspond to those from the available sample, which we consider sufficient to provide us with knowledge of many different aspects of cardiac pacing in Spain.
The study made use of all information included on each card. A summary of the data generated is also submitted to the European Pacemaker Registry.10,11
RESULTS
Number of Pacemakers Implanted per Million Inhabitants
In 2009 a total of 34 103 conventional pacemaker generators, including 515 cardiac pacing devices for cardiac resynchronization therapy (CRT) using low-power dual-chamber devices without defibrillation capability (CRT-P), were implanted according to data submitted to the BNDM.
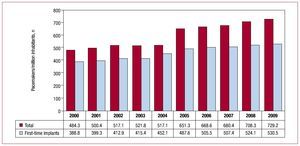
According to the INE, the population census in the reference year was 46 745 000 inhabitants, and so the number of pacemaker generators used was 720.2 per million inhabitants (Figure 1).
Figure 1. Total number of generators per million inhabitants between 2000 and 2009.
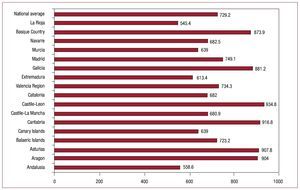
When we analyze the distribution of the units used in the different autonomous regions, we see a notable difference in the number of units implanted per million inhabitants, with a profile very similar to previous years,8,9 and in excess of 900 units in the regions of Castile-Leon, Cantabria, Asturias, and Aragon, and 800 in Galicia and the Basque Country. In general, there were more implants in the autonomous regions in the north of Spain, where the population is more elderly, as has been noted on previous occasions (Figure 2).7-9
Figure 2. Pacemaker generators implanted per million inhabitants by autonomous region and national average in 2009.
Dual-Chamber Pacing
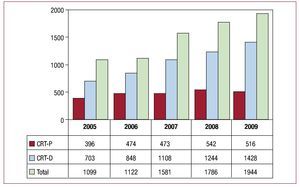
The number of devices used for CRT shows a progressive annual increase and reached 41.5 units/ million inhabitants in 2009. This increase was due to units with capacity for defibrillation. The CRT-P devices, after increasing in 2008, showed a small decrease in 2009 compared to the previous year (Figure 3) (11 units/million inhabitants).
Figure 3. Cardiac resynchronization therapy devices implanted between 2005 and 2009. CRD-D, dual-chamber generator with defibrillation capability; CRD-P, dual-chamber device with pacing only.
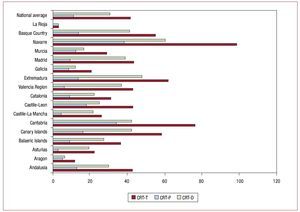
The analysis of generators used for CRT in the autonomous regions revealed significant differences, probably as a result of the greater or lesser dedication of the hospitals to treatment of heart failure with pacing. The region with the greatest number of implants was Navarre, both in terms of devices with CRT-P and with associated implantable cardioverter devices, followed by Cantabria, Extremadura, the Canary Island, and the Basque Country (Figure 4).
Figure 4. Cardiac resynchronization therapy devices per million inhabitants by autonomous communities and national average in 2009. CRT-D, dual-chamber generator with defibrillation capability; CRT-P, dual-chamber device with pacing only; CRT-T, total CRT generators.
Age and Sex
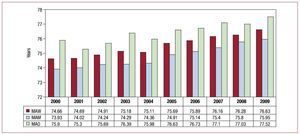
The mean age of the patients requiring a first-time pacemaker implant was 76.6 years in 2009. A progressive increase in the mean age continues to be observed as a result of the longer life expectancy, which is associated with a higher incidence of degenerative diseases responsible for most of the implants. The mean age was 75.9 years in men and 77.5 years in women. This difference of almost 2 years remains similar to that of previous years (Figure 5).2-9
Figure 5. Mean age and sex of patients who received pacemaker implants. Changes between 2000 and 2009. MAM, mean age of men; MAW, mean age of women; MAO, mean age of overall sample.
The mean age of the patients who needed generator replacement was 76.5 years, almost the same as that of the implants.
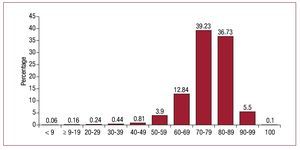
Most implants were performed in patients between 70 and 80 years of age, 39.2% of the total, followed by those aged 80 to 90 years (36.7%) (Figure 6). For replacements, the most common age for the intervention was 80 to 90 years (39.1%) followed by 70 to 80 years (33.2%). Patients over 100 years accounted for 0.1% of pacemaker implants and 0.12% of generator replacements.
Figure 6. Pacemaker implantation by 10-year age intervals in 2009.
The use of generators was greater in men (58%), both for pacemakers (58.4%) and replacements (56.8%), and in all age groups, except for patients aged 90 to 100 years due to the greater longevity of women. This higher incidence of implants in men has been observed ever since the BNDM has collected data.9
Type of Procedure
Implant and Pacemaker Replacement
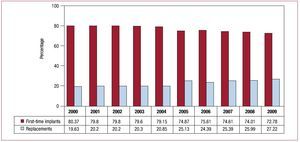
All procedures related to cardiac pacing systems in which a pacemaker was implanted for the first time constitute 72.8% of the total and so a frequency of 530.5 first-time implants per million inhabitants was estimated.
Replacement procedures accounted for 27.2% of all generators used, and so the trend towards an increase in such procedures compared to first-time implants continues (Figure 7). Generator replacements that required implantation of new leads or replacement leads during the procedure accounted for 1.6% of all reported procedures.
Figure 7. Percentage of pacemakers and replacements between 2000 and 2009.
Among the reasons for replacement of the generator, the most frequent (86.6%) was the battery running out at the end of its useful life (early replacement accounted for 0.2% of the procedures, either due to high thresholds or because the battery ran out early). The next most frequent was infection (2.6%), mechanical erosion or protrusion (1.6%), a change in system to improve hemodynamic parameters (0.3%), and a defective generator (0.2%).
Electrode Leads
Most of the leads used for pacing were of the bipolar type (99.8%). Of those implanted in the right atrium and right ventricle (RV), 99.9% were bipolar.
Of the leads used for left ventricular pacing, for CRT, or because of problems of access to the RV (such as presence of a prosthetic tricuspid valve), 55% were bipolar.
The small percentage of monopolar leads (0.2%) corresponded mainly to leads intended for implantation via the coronary sinus (80.7%), implants within the RV (11.5%), and implants within the right atrium (3.8%). The remaining monopolar leads were implanted during heart surgery.
The fixation system used with the leads to stabilize them in the endocardium has changed from passive fixation (using flexible tabs) to active fixation (helix, usually extendable). In 2009, this fixation system was used in 51.5% of the cases (>65% in the atrial position, 45% in the ventricular position) (Figure 8). The possible causes of this trend towards a change of fixation system are the good thresholds obtained with the current active fixation leads (similar to passive fixation), the partial trend away from traditional pacing in the right atrial appendage and apex of the RV to other alternative sites and the easier explantation if necessary, as all leads have the same diameter. The use of the active fixation system is essential for stabilizing the lead when the target implantation area of the electrode is not very trabeculated, as is the case in the Hisian area, the sinus node, and the RV outlet tract.
Figure 8. Active fixation electrodes: percentage of total and of implants in atrial and ventricular chambers between 2000 and 2009.
Implantation of a new lead-electrode of the pacing system accounted for 1.7% of the procedures recorded in 2009. In total, 1.5% were procedures associated with generator replacement, to improve hemodynamics, or elective due to deterioration of the electrical characteristics of the lead or because it was damaged during the surgical procedure. Isolated replacement of the cardiac pacing lead accounted for 0.2% of the procedures performed.The most frequent reasons for changing or explanting the electrode lead were, in descending order, infection or ulceration (50.9%), displacement or sensing problems (15.3%), breakage of the conductor (7.8%), exit block (5.8%), and elective (2%). Symptoms, Etiology, and Electrocardiographic Disorders Leading to Implantation The clinical signs and symptoms before implantation of pacemakers, in descending order of incidence, were syncope (42.2% of cases), dizziness (27.5%), dyspnea or signs of heart failure (14.9%), bradycardia (8.7%), implants in asymptomatic patients or prophylactic implants (3%), chest pain or tachycardia (1%), brain dysfunction (0.9%), and risk of sudden death after return to bradyarrhythmia (0.2%).On analysis of these signs and symptoms prior to implantation, only patients who underwent a replacement (years later), a very similar distribution to that described was observed, reflecting the little change in clinical presentation over the years. The most common etiology in the indication for implantation was, as in previous years, supposed fibrosis of the conduction system (42.6%), followed by unknown etiology (41.1%). Ischemia accounted for 6.5%, followed by cardiomyopathies (3%, with hypertrophic cardiomyopathy accounting for 0.6%) and valve disease (2.8%). The group of iatrogenic or therapeutic effects accounted for 2%; with atrioventricular node ablation accounting for 0.8% (the first year that this percentage is below 1% in the last few years analyzed). The neuromediated causes were less than 1% this year (vasovagal 0.3%, carotid sinus syndrome, 0.6%). The indication was associated with congenital etiology in 0.6%. The most common electrocardiographic disorder in the indication for implantation was atrioventricular conduction disorders, corresponding to 56.1% of cases. Of these, third-degree atrioventricular node block (AVB) was the most common (37.3%), without including AVB in atrial fibrillation. After atrioventricular conduction disorders, the next most common was sick sinus syndrome (SSS), in its different guises, accounting for 21.1% (37.3% if the atrial fibrillation subgroup or atrial flutter [AFib/ AF] with bradycardia was included). Ventricular conduction disorders (VCD) accounted for 5% of all electrocardiographic disorders.
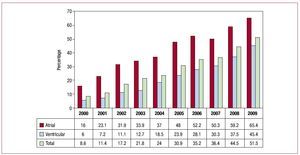
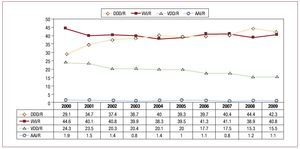
In general, electrocardiographic disorders remained stable despite new indications for pacing in recent years (Figure 9).
Figure 9. Distribution of electrocardiographic abnormalities prior to implantation between 2000 and 2009. AFib/AF+BRAD, atrial fibrillation/atrial flutter with slow ventricular response; AVB, atrioventricular node block; SSS, sick sinus syndrome; VCD, ventricular conduction disorder.
In the analysis of electrocardiographic disorders by sex, of note is a higher incidence of atrioventricular conduction disorders and VCD in men, already apparent in recent years, due to the greater degeneration of the conduction system. The incidence of SSS is similar in both sexes.6-9 This explains the greater number of implants in men.
Pacing Modes
General
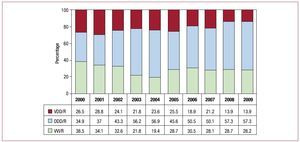
Of all pacemakers implanted in 2009, isolated single-chamber atrial pacing (AAI/R) accounted for only 1.1% of all generators. The limited use of this mode is reflected both in implantation (1.2%) and replacements (1%), was seen in every year analyzed, and did not exceed 2% (Figure 10).
Figure 10. Overall change in all pacing modes between 2000 and 2009.
Single-chamber ventricular pacing (VVI/R) was chosen as the pacing mode in 40.8% of cases, but a certain variation was observed between the first-time implant (42.1%) and replacement generators (37.5%). As in previous reports, the mode was changed from the most recommended one due to electrocardiographic disorders in a high percentage of patients (>20%). Patients in permanent atrial tachyarrhythmia accounted for 20.4% (the same percentage as in 2008: AFib/AF associated with bradycardia, 16.2%; AFib/AF with AVB, 4.2%) and these are the only patients in whom VVI/R mode would be appropriate.10,11 The breakdown of the different electrocardiographic manifestations is described in the following sections, along with factors, such as age, that might affect compliance with the recommendations.
Single-probe sequential pacing (VDD/R) accounts for 15.5% of all units, as in the previous year (Figure 10). There is a trend towards stability, although there is a marked difference in their use in first-time implants (13.4%) compared to replacements (21.3%). This indicates greater use of this pacing mode in previous years, when it accounted for 24% of all generators (Figure 10). Spain is one of the countries where this type of pacing is most used: it is estimated that 5285 units used this mode in 2009.
Dual-lead sequential pacing (DDD/R) was the most widely used, both in general (42.3%) and when analyzing first-time implants (43.1%) and replacements (40%) separately. On comparing the pacing modes with previous years, a slight decrease in DDD/R mode is observed, due to a shift towards units operating in VVI/R mode. No significant changes were observed in the other modes AAI/R and VDD/R (Figure 10).
In pacing for CRT-P, a slight decrease in the number of units was observed (516; 1.5% of the total number of generators), similar to the figure for 2007 (Figure 3). Nevertheless, ventricular resynchronization therapy continues with a notable increase due to the high-power units, as discussed earlier.
There was also the possibility of varying the frequency of pacing by means of 1 or 2 biosensors (accelerometer, tidal breathing, etc) in 84.4% of the cases.
Pacing in Conduction Disorders
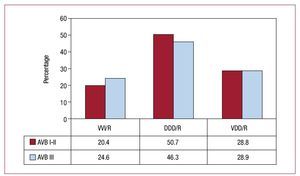
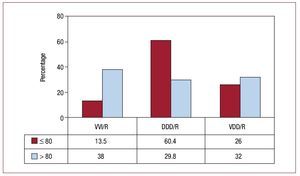
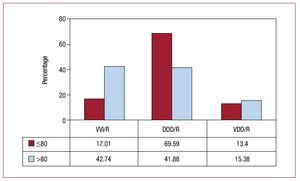
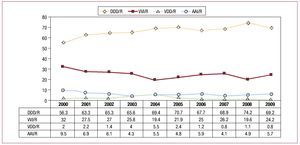
Atrioventricular block. In the study of this group, we excluded, as is the norm, the subgroup of patients who were in permanent atrial tachyarrhythmia (AFib/AF with AVB, corresponding to code C8 of the EppiCard) to correctly assess this type of cardiac pacing in patients who maintain stable sinus rhythm. Pacing in synchrony with the atrium (VDD/R and DDD/R modes) is the most common type (accounting for 76.5% of cases; 47.6% DDD/R and 28.9% VDD/R) (Figure 11). When we compare the pacing mode according to the degree of block, grouped by first and second degree and third degree, we see that synchronous pacing is performed with the atrium in a slightly higher percentage of patients in first- and second-degree AVB (79.5%) than third-degree AVB (75.2%). The variations correspond to the greater or lesser use of the DDD mode, as use of the VDD mode remains the same in both degrees of block, with 28.8% and 28.9%, respectively (Figure 12). The trend towards decreased use of VDD mode, as observed in recent years, could have leveled off after being the most widely used in this type of electrocardiographic disorder (Figure 12). Comparison of atrial-based pacing modes by age group (≥80 years or <80 years) showed that use in the older patients was 61.9% and use in the younger group was 86.4%. This variation is due to a preference for the DDD mode in the youngest patients (60.4%), whereas the percentage of patients with the VDD/R mode was greater in the older age group (32% compared to 26% in the younger age group) (Figure 13). VVI/R pacing continues to be chosen in a high percentage of patients with AVB in sinus rhythm (23.5%) and is as high as 38% in patients aged over 80 years. This was the year in which this pacing mode was least used, among all those analyzed, considering groups of all degrees of AVB, and it was also the least used in the oldest subgroup of patients (Figure 14), despite certain controversy in the choice of mode in elderly patients with AVB in current clinical practice guidelines.12 The use of this single-chamber ventricular pacing mode is somewhat less in the group of patients who retain a certain AV conduction; thus in first- and second-degree AVB the figure was 20.4%, while for third degree AVB, it was 24.6% (Figure 12). The age of the patient continues to be a determining factor in the choice of VVI/R mode, while degree of AVB is of less importance.
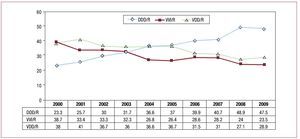
Figure 11. Change in pacing modes in atrioventricular block (excluding patients with permanent atrial tachyarrhythmia, code C8) between 2000 and 2009.
Figure 12. Pacing modes in atrioventricular block (AVB) by first- and second-degree block and third-degree block in 2009.
Figure 13. Pacing modes in atrioventricular block (excluding patients with permanent atrial tachyarrhythmia) for patients aged 80 years or less and those over 80 years in 2009.
Figure 14. Change in VVI/T mode in atrioventricular blocks for patients aged 80 years or less and those over 80 years in 2009.
Ventricular Conduction Disorders. This group is the one whose pacing has remained the most uniform and stable in recent years. In 71.8% of patients, modes are chosen that maintain AV synchrony, a figure practically the same as in the last 3 years, but with a certain change from VDD units to DDD units in 2008. In 2009, there is the same distribution of pacing modes as in 2008, with 13.9% using the VDD mode, the least frequently chosen, and 57.9% using the DDD/R mode. Single-chamber pacing in the VVI/R mode remained stable at 28.2% (Figure 15). Once again, age was the determining factor in choosing which mode to use, such that VVI/R is the most used in older patients (42.7% in patients over 80 years) and DDD (70%) in younger patients. The VDD mode is the least affected by age, as it is used to a similar extent in both age groups—13.4% and 15.3% for younger and older patients, respectively (Figure 16). According to the data available in the registry, the devices used for CRT-P for cardiomyopathy associated with VCDs accounted for 8.9% of all pacemakers implanted for VCDs (13.9% in the subgroup of patients under 80 years and only 1.8% in those over 80).
Figure 15. Pacing modes in ventricular conduction disorders. Changes between 2000 and 2009.
Figure 16. Pacing modes in ventricular conduction disorders for patients aged 80 years or less and those over 80 years.
Pacing in Sick Sinus Syndrome
Study of this group was done in 2 parts, patients with AFib/AF and bradycardia (code E6 of the EppiCard) and patients with other electrocardiographic disorders in SSS (codes E1-E8), which correspond to patients who theoretically are mainly in sinus rhythm. This provides an indication of how appropriate the choice of pacing modes is.12,13
In the subgroup of patients with permanent atrial arrhythmia (AFib/AF), it is expected that all would be paced in VVI/R mode. This was the case in 94.8%. However, 4.7% (similar percentage to other years) are paced in DDD/R mode. This can be explained by an error in coding or, more likely, because the patients are implanted with a pacemaker in atrial tachycardia with the intention of reverting subsequently to sinus rhythm. A constant feature of all years studied is the low percentage of patients paced in VDD/R mode (0.4%), an approach that can only be justified by technical problems with implantation (difficult access, multiple abandoned leads, etc).
The remaining subgroups of SSS, supposedly in stable atrial rhythm, at least partially, underwent atrial-based pacing with capability for atrial pacing and sensing in 75% of the cases (69.3% DDD/R and 5.7% AAI/R), which are the recommended modes for this type of electrocardiographic indication in the clinical practice guidelines.12,13 In 2009, pacing underwent a small decline in the quantity of pacing procedures compared to 2008, the year when the most pacing procedures for this disease were performed.9
Isolated single-chamber pacing, with a percentage of 5.7%, remained in line with other years without any large variations, even after the introduction of units able to switch between AAI/R and DDD/R modes. The AAI/R mode is still underused, perhaps as a result of the uncertainty in the progression to AVB (although the risk without associated VCD is very low), even though it has both potential economic advantages and fewer potential complications, as the ventricle is not paced and there are fewer electrodes than with the DDD/R.
With regard to single-chamber ventricular pacing, there is again, in the current year, a certain increase in VVI/R pacing (24.2%) and the persistence of a low percentage of VDD pacing (0.8%); both are less appropriate due to the greater risk of atrial tachycardia, ventricular dysfunction, risk of pacemaker syndrome due to retrograde conduction, etc (Figure 17).
Figure 17. Pacing modes in sick sinus syndrome (SSS) between 2000 and 2009 (excluding patients with permanent atrial tachycardia, code E6).
In an attempt to assess whether any of the electrocardiographic manifestations in SSS had a greater or lesser influence on the aforementioned compliance with the pacing modes, the type of pacing has been analyzed for each one. It is observed that a substantial number of patients are paced in VVI/R mode, with percentages ranging form 18% to 32% (the latter corresponding to code E5 of the EppiCard, tachycardia-bradycardia syndrome). Subgroups E7 and E8 were not studied as they are poorly represented in SSS (0.9% and 0.3%, respectively) (Figure 18). It is possible that the higher percentage of VVI/R pacing under the E5 code of the EppiCard for SSS is partly due to wrong classification and confusion of tachycardia-bradycardia syndrome (episodes of atrial tachyarrhythmia and sinus bradycardia) with patients with episodes of fast-slow permanent atrial fibrillation, who should be included under the E6 code described earlier. Nevertheless, even excluding these patients, a significant lack of compliance in the selection of the mode can be appreciated in all electrocardiographic manifestations of SSS, and this is something we should try to correct.
Figure 18. Distribution of the percentage of VVI/R pacing according to electrocardiographic code indicated on the card carrier for sick sinus syndrome (SSS) in 2009. E1, not specified; E2, exit block; E3, sinoatrial arrest; E4, bradycardia; E5, bradytachycardia.
If, as in previous years, we assess the possible influence of age on compliance with mode selection, according to the 2 age groups defined by the cut-off of 80 years, as is common practice in the BNDM, a marked difference in the use and selection of DDD and VVI/R modes can be observed. Pacing in DDD/R mode was performed in 77.3% of those under 80 years and 57.4% of those aged over 80 years (Figure 19). Single-chamber pacing was performed in 16.4% and 35.7%, respectively. As can be seen in the pattern of changes over the years, this percentage was highest in 2008 in both age groups (Figure 20). The use of other modes, both AAI/R and the uncommon VDD/R, is similar for both age groups (Figure 17).
Figure 19. Pacing modes in sick sinus syndrome for the two age groups in 2009.
Figiure 20. VVI/R pacing modes in sick sinus syndrome for patients aged 80 years or less and those over 80 years from 2001 to 2009.
Thus, a significant lack of compliance with the recommended modes can be seen, particularly in older patients, as in previous years.6-9
CONCLUSIONS
The 2009 data from the registry show an increase both in the total number of generators used and the number of units per million inhabitants, except for low-power dual-chamber pacing units, whose usage dropped slightly. The percentage of units used for generator replacement accounted for 27.2% of all activity reported to the registry.
There is a significant imbalance between different autonomous regions, both in terms of the number of implants of conventional units per million inhabitants and number of implants for CRT.
The mean age of the patients who receive first-time pacemakers continues to increase slightly due to the greater longevity (76.6 years); in men, the age is approximately 2 years younger than in women. There continues to be more implants in men, due to the higher incidence of conduction disorders in this group. Third-degree AVBs are the most common electrocardiographic disorder (37.3%) leading to implantation.
The fixation system for endocardial leads is shifting towards active fixation; this system now accounts for more than 50% of those used. Bipolar leads were implanted.
VVI/R mode pacing was used in 23% of patients with AVB and 24.2% of those with SSS, with atrial-based pacing modes possible.
The use of single-lead VDD/R mode remained stable over the last 2 years. In AVBs, the most frequent indication for implantation, 29% were paced in this mode.
The age of the patients remains the most decisive factor for the appropriate selection of the pacing mode.
ACKNOWLEDGMENTS
We thank the graduate nurses, Pilar Gómez Pérez and Brígida Martínez Noriega, for their dedication to the maintenance of the registry. We also thank the IT specialist of the Spanish Society of Cardiology, Gonzalo Justes Toha, for his valuable collaboration in analyzing the registry, and all the health professionals of the hospitals that participated directly or indirectly in filling out and submitting the cards of the pacemaker carriers. In addition, we thank the staff of the different pacemaker companies present in Spain (Biotronik, Boston, Medico, Medtronic-Vitatrón, Saint Jude and Sorin Group), for their regular collaboration in the registry, both for submitting cards of pacemaker carriers and for compiling the annual information necessary for calculating the number of units used.
ABBREVIATIONS
AFib/AF: atrial fibrillation/atrial flutter
AVB: atrioventricular block
BNDM: Spanish Registry of Pacemakers
CRT-P: cardiac resynchronization therapy with a pacemaker (without defibrillation)
EPPICard: European Pacemaker Patient Identification Card
INE: Spanish National Institute of Statistics SSS: sick sinus syndrome
VCD: ventricular conduction disorder
Correspondence: R. Coma Samartín. Arturo Soria, 184. 28043 Madrid. Spain.
E-mail: coma@vitanet.nu