Optical coherence tomography (OCT) is an intracoronary diagnostic technique of particular interest for characterization of the atheromatous plaque and assessment of the outcome of stenting by percutaneous coronary intervention. We present a case of stent thrombosis in which OCT provided very useful information for arriving at the diagnosis, understanding the thrombotic mechanism, deciding on the most appropriate therapeutic strategy, and guiding percutaneous coronary intervention.
The patient was a 65-year-old man, referred for primary angioplasty due to inferolateral acute myocardial infarction with onset 3h earlier. He had completely discontinued double antiplatelet therapy 1 week earlier. Eight months earlier, he had experienced a non-Q-wave acute myocardial infarction for which 2 overlapping drug-eluting stents were placed in the second obtuse marginal branch. Another drug-eluting stents was placed in the ostium of the first obtuse marginal branch with adjustment by simultaneous balloon deployment in the proximal circumflex artery (Figs. 1A and B). The only finding in the coronary angiography performed during inferolateral stent thrombosis elevation was the presence of a small filling defect in the proximal circumflex artery (Fig. 1C). OCT confirmed the presence of a thrombus in the proximal end of the stent in the first obtuse marginal branch. Moreover, this stent protruded into the lumen of the circumflex artery itself. Several stent struts lacked neointimal coating and there was a thrombus adhered to its surface. The technique also showed that, on advancing towards the distal segments of the second obtuse marginal branch, our guide had crossed through this stent's cells (Fig. 2A). We therefore advanced a second guidewire and it was confirmed that this time, it had gone beyond the stent (Fig. 2B), and so stent crushing could be performed (Fig. 1D). After administering an intracoronary abciximab bolus, we placed another drug-eluting stents in the proximal circumflex artery and inflated a kissing balloon at the circumflex artery and the first obtuse marginal branch (Figs. 1E and F).
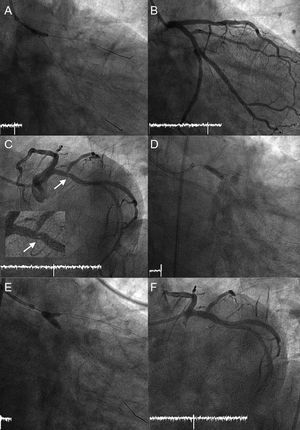
A: Stent (2.25×8mm) placed in the ostium of the first obtuse marginal branch, facilitated by simultaneous deployment of a low-pressure angioplasty balloon in the proximal circumflex artery. B: Final angiographic outcome of the first intervention. C: Small filling defect in the circumflex artery (arrow) with TIMI 3 distal flow in all branches. D: Crushing of the proximal end of the stent of the first obtuse marginal branch with the angioplasty balloon. The stent was protruding into the circumflex artery. E: Kissing balloon after stenting of the proximal circumflex artery. F: Final angiographic outcome of the second intervention.
Optical coherence tomography. A: Initial withdrawal; it can be seen that our angioplasty guidewire and the optical coherence tomography probe have passed through the stent placed in the ostium of the first obtuse marginal branch, given that this stent protrudes into the circumflex lumen. In A1, the red thrombus (+) distal to the stent can be observed. Note that this type of thrombus produces a posterior shadow that hinders both assessment of the arterial wall and evaluation of potential underlying mechanical problems (for example, malapposition). In A2, thrombus (+) adhered to the stent struts. In A3, angioplasty guidewire and optical coherence tomography probe inside the stent, which also has thrombotic remains adhered to its struts. B: New withdrawal after advancing a second guidewire. In B1, second angioplasty guidewire and optical coherence tomography probe outside the stent; the first guidewire can also be seen being introduced into the stent lumen (arrow). C: Final withdrawal. In C1, ostium of the first obtuse marginal branch; in C2, 3 layers of stent (*) in the wall of the circumflex artery after stent crushing and kissing-balloon. OM1, first obtuse marginal.
As seen in our case, the angiographic appearance of stent thrombosis is sometimes subtle and may go unnoticed. In the face of clinical suspicion, intracoronary diagnostic techniques are of great help for confirming or ruling out diagnosis and contributing to an understanding of its causal mechanism. Thus, OCT is extremely useful in view of its high sensitivity for identifying the thrombus and stent-related factors (lack of endothelialization, infraexpansion, malapposition, neoatherosclerosis, etc.) that may be implicated in thrombosis.1,2 Identification of the thrombus and stent-related factors is essential when deciding on therapeutic strategy, which may range from manual extraction only of the thrombus or intensification of antithrombotic treatment to balloon dilatation, with or without the need for repeat stenting.3 In our patient, in addition to discontinuation of antiplatelet therapy, we discovered the presence of a determinant mechanical factor: a small-diameter partially endothelialized stent that protruded into a larger diameter vessel. This finding was essential when making the decision to perform stent crushing.
Recently, it has been shown that OCT could be of use in percutaneous coronary intervention in bifurcation lesions, particularly when recrossing the angioplasty guidewire through the struts, as angiography and intravascular ultrasound may be of more limited value in this situation.4 As we show, an exact knowledge of the position of the guidewire relative to the previously placed stents may be of additional value, as it allows the desired bifurcation technique to be performed and avoids suboptimal angiographic outcomes with an increased risk of future adverse events.
Although there is a lack of solid studies that demonstrate the clinical benefits of OCT-guided percutaneous coronary intervention, we believe that this case illustrates that OCT may be of use in some situations, such as treatment of stent thrombosis or bifurcation lesions.