Keywords
INTRODUCTION
Aortic root dilatation in Marfan syndrome (MS) can cause acute dissection, aortic rupture, and aortic regurgitation1 and is a common cause of premature death.1,2 Prophylactic replacement has achieved a substantial improvement in life expectancy.3,4 Most published studies are from Europe and the United States; no series in Latin America have been reported. In the present study, we describe the short-term results (inhospital follow-up) and long-term outcome (complications) of surgery at a tertiary referral center in Argentina.
METHODS
Between July 1992 and December 2006, 54 patients with MS underwent surgery based on criteria subsequently confirmed at Ghent, Belgium.5 The surgery was performed in accordance with routine procedures.6 Surgery performed in a decompensated patient within 24 hours of diagnosis was considered as emergency, surgery performed during hospitalization but after 24 hours as urgent, and surgery undertaken while the patient was stable and asymptomatic as scheduled. The demographic characteristics, in-hospital mortality, late mortality, and need for repeat surgery or interventional treatment on follow-up were analyzed retrospectively. The following events were considered: death, repeat surgery, infective endocarditis, thromboembolism, and major bleeding. Doppler transesophageal echocardiography (TEE), computed tomography (CT), or magnetic resonance imaging was used for the diagnosis. Doppler TEE was performed during surgery, and follow-up was based on TEE and CT. All patients received beta-blockers.
Statistical Analysis
Continuous variables are reported as the mean (SD) or range, and categorical variables, as percentages. The univariate analysis was performed using ANOVA for continuous variables with a normal distribution and the χ2 test for qualitative variables. The Kaplan-Meier method was used to calculate patient survival. The survival rates and 95% confidence intervals (CI) for the different periods are shown.
RESULTS
Mean patient age was 39 years (range, 18-66); 25% were women. Fifteen patients had acute aortic dissection; 6, chronic aortic dissection; and 33, ascending aorta aneurysm. The average (SD) aortic diameter was 66.6 (3) mm. A comparison of the demographic, clinical, and echocardiographic data is presented in Table 1.
The surgery was emergency in 3 (5.6%) patients, urgent in 15 (27.8%), and scheduled in 36 (66.7%); 4 patients had previous aortic surgery. Aortic root replacement used a valved conduit (Bentall de Bono procedure) in 39 patients with a Cabrol modification in an additional 3, valve reimplantation (T. David) in 9, and a homograft in 3. Mitral valve replacement or plasty was performed in 6 patients.
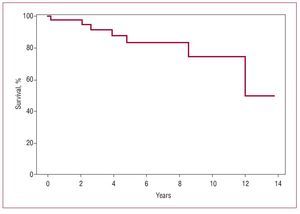
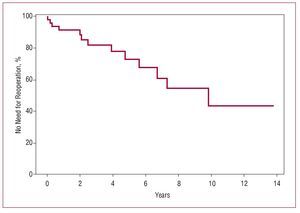
Surgical mortality was 3.7% (2 patients) and was significantly higher in the emergency surgeries compared with elective surgery (33.3% vs 2.8%; P<.001). On follow-up (mean, 4 years [range, 2 months-14 years]), 3 (5.5%) patients were lost, and another 7 died; among them, 4 had type B redissection that had been reoperated and culminated in sepsis (3 from surgery and 1 from catheterization), 2 died of heart failure, and 1 of an unknown cause. Thirteen patients required a second operation, including 9 procedures to treat a distal redissection, 1 heart transplantation, and 3 homograft placement for infective endocarditis. Two patients had a third operation. Survival at 2, 5, and 10 years was 94% (95% CI, 88-100), 83% (95% CI, 70-97), and 75% (95% CI, 55-95), respectively (Figure 1). Reoperation at 2, 5, and 10 years was not necessary in 88% (95% CI, 78-98), 67% (95% CI, 50-85), and 43% (95% CI, 17-70), respectively (Figure 2).
Figure 1. Survival curve of 54 patients with Marfan syndrome operated for complications of the ascending aorta.
Figure 2. No need for reoperation in 54 patients with Marfan syndrome operated for complications of the ascending aorta.
DISCUSSION
Before the advent of prophylactic aortic root surgery, most patients died prematurely; life expectancy with the current treatment is 70 years.3,4 There is a clear association between increased diameter and the risk of dissection and rupture in this condition: the risk of rupture of a 6-cm aneurysm is 4-fold.7 The recommended aortic diameter for prophylactic surgery is 5 cm.7,8 An accelerated increase (>1 cm/y), family history of premature death, or moderate-to-severe aortic regurgitation will require earlier surgery.1 Some authors propose that surgery be done at diameters >3 cm because of the unpredictability of aortic rupture.8 The efficacy, safety, and reproducibility of ascending aorta replacement with valved conduits were initially described by authors from a single institution.9 Later, a report emerged with a series of 675 MS patients operated at 10 surgical centers.10 In that study, 30% presented aortic dissection and 30-day mortality was 1.5% in elective surgery, 2.6% in urgent surgery, and 11.7% in emergency surgery. In 6.7 years of follow-up, there were 114 late deaths, most due to residual aortic dissection or rupture, and arrhythmias, mainly within the first 60 days after surgery. Later, mortality was low and constant: 93.5% of patients were alive at 5 years, 91% at 10 years, and 59% at 20 years. Subsequent experience confirmed these results.11 Similar to the multicenter patient population, 38% of our patients presented aortic dissection. Overall mortality was somewhat higher at 3.7% (elective, 2.8%; emergency, 33%), survival rates were 94% at 2 years, 83% at 5 years, and 75% at 10 years, and there was no need for reoperation in 88%, 67%, and 43%.
Yacoub et al12 described a valve-sparing "remodeling" technique for the aortic valve and David et al,13 "reimplantation" in a tubular Dacron graft. The use of these techniques was restricted to patients with structurally normal aortic valves. David et al14 retrospectively analyzed 220 valve-sparing surgeries (167 with reimplantation and 53 with remodeling), 40% in MS patients, with a follow-up of 5.3 years. There were 3 operative deaths and 13 late deaths. Overall survival at 10 years was 88% and freedom from significant aortic regurgitation was 85% (94% with reimplantation and 75% with remodeling). Reimplantation was used in 9 of our patients, with no surgical mortality or significant mid-term aortic regurgitation. However, there are no reports of long-term follow-up with this technique and the need for reoperation has not been established.15,16
A study of 78 MS patients who underwent surgery was recently conducted. During follow-up (mean, 5.4 years) 4 patients died and 46 "aortic events" (elective surgery or dissection) occurred in 45 patients, with distal aortic involvement in 14 patients (31%).17 Consistent with that series and with others,9-12 25% of our patients required repeat surgeries in the distal aorta. Hence, we believe that all MS patients who have undergone surgery should receive indefinite regular follow-up of the aorta.
We conclude that elective replacement of the ascending aorta with valved conduit is a low-risk, effective, and long-lasting procedure in patients with MS.
Correspondence: Dr. R.R. Favaloro.
ICYCC. Fundación Favaloro.
Avda. Belgrano 1746. (1093) Buenos Aires. Argentina.
E-mail: rrfavaloro@ffavaloro.org
Received May 23, 2007.
Accepted for publication December 11, 2007.