Previous studies have reported that coronary intervention for complex lesions is independently correlated with major bleeding. The SYNTAX score is an angiographic tool used to grade the complexity of coronary artery diseases. The aim of this study was to assess the ability of the SYNTAX score to predict major bleeding following drug-eluting stent implantation.
MethodsWe analyzed 722 patients who underwent drug-eluting stent implantation in an all-comers population between January 2007 and April 2010. The incidence of major bleeding and stent thrombosis was investigated during a 2-year period. Major bleeding was evaluated using the CRUSADE score and Bleeding Academic Research Consortium criteria. Patients were stratified into the following groups according to the SYNTAX trial: low (≤ 22; n=484), intermediate (23–32; n=128), and high (≥ 33; n=110).
ResultsMajor bleeding was observed in 47 patients (6.5%) during the 2-year period, and there were 12 incidents of stent thrombosis (1.7%). Major bleeding rates for patients in the low, intermediate, and high SYNTAX score tertiles were 2.9%, 7.8%, and 20.9%, respectively (P < .0001). The SYNTAX score had an adjusted hazard ratio of 1.81 (95% confidence interval, 1.27-2.57) for 2-year major bleeding. The predictive value of the adjusted area under the receiver operating characteristic curve for major bleeding significantly improved after inclusion of the CRUSADE score (C statistic, 0.890 vs 0.812).
ConclusionsAlthough the SYNTAX score can predict major bleeding risk, the predictive value of the CRUSADE score was higher. These scores may be useful in clinical decision-making on revascularization strategies and on the optimal duration of dual antiplatelet therapy following drug-eluting stent implantation.
Keywords
Major bleeding is one of the most frequent complications of percutaneous coronary intervention (PCI) and antithrombotic therapy.1 In the era of bare-metal stents, the incidence of major bleeding following PCI was as high as 5.4%, which is close to the incidence of major adverse cardiac events, including death, myocardial infarction, and ischemia-driven repeat PCI.2 In recent years, more aggressive antiplatelet regimens and prolonged dual antiplatelet therapy (DAPT) have been used with the objective of reducing the incidence of thrombotic events following PCI. However, these strategies increase the risk of bleeding complications.3–5 Importantly, bleeding complications following PCI have been associated with an increased risk of subsequent adverse outcomes, including myocardial infarction, stroke, and death.6,7 Therefore, the bleeding risk must be balanced against the antithrombotic benefits of such therapies. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) trial was the first to compare coronary artery bypass grafting and drug-eluting stent (DES) implantation in patients with left main and 3-vessel disease. The SYNTAX score (SXscore) is an angiographic tool used to grade the complexity of the coronary artery disease.8 A previous study reported that PCI of complex lesions independently correlates with major bleeding.9 Thus, the aim of this study was to assess the ability of the SXscore to predict major bleeding following DES implantation.
METHODSBetween January 2007 and April 2010, 845 consecutive patients with coronary artery disease underwent DES implantation at Ohashi Hospital. This study enrolled all-comers, including patients with chronic stable coronary artery disease and acute coronary syndrome, reflecting routine clinical practice. Patients with malignancies, increased bleeding risk (stroke within the previous 3 months, active bleeding, recent trauma, or major surgery in the previous month), or contraindications to prolonged DAPT (up to 12 months), and those who were treated with bare-metal stents, balloon angioplasty, or who had prior coronary artery bypass grafting were excluded from the study. In addition, we excluded patients who were not able to be evaluated using the SXscore and the acquired angiogram. A total of 722 patients who underwent DES implantation were analyzed in this study. Clinical and procedural data were prospectively entered into a database and retrospectively analyzed. All patients provided written informed consent.
Stent and Post-procedural ManagementPatients scheduled for PCI were administered acetylsalicylic acid (100mg) and clopidogrel (75mg) daily for at least 3 days before the procedure. In cases of unstable angina or urgent PCI within 48h of admission, a 300mg clopidogrel loading dose was administered before the procedure. For all patients, a bolus injection of heparin (100 IU/kg) was administered after sheath insertion, and was titrated to maintain an activated clotting time of >250s throughout the procedure. Because of the observational nature of this study, the type of DES (sirolimus-, paclitaxel-, zotarolimus-, or everolimus-eluting stents) used was at the surgeon's discretion. After stent implantation, a high-pressure balloon inflation procedure was performed to achieve satisfactory angiographic results with < 25% residual stenosis by visual estimate. All patients received 100mg acetylsalicylic acid and 75mg clopidogrel per day for ≥12 months. Continuation of DAPT and other cardiac medications were prescribed at the physician's discretion.
The SYNTAX Score and Angiographic AnalysisOn the basis of baseline diagnostic angiograms, each coronary lesion producing ≥ 50% diameter stenosis in vessels ≥ 1.5mm was scored separately. Thereafter, these scores were added together to provide the overall SXscore, which was calculated using the algorithm available on the SYNTAX website.10 The SXscores of patients were independently assessed by 2 experienced interventional cardiologists blinded to the clinical data, who had experience in calculating the SXscores of >100 patients before assisting in our study. The κ value for interobserver variability that was used to estimate the SXscores was 0.75, while the κ value for the intraobserver variability was 0.86. If there was disagreement regarding the SXscores, the average of the values from the 2 readers was used as the final value.11
Definitions and Follow-upThe primary endpoint was the incidence of major bleeding within 2 years after PCI. Based on the Bleeding Academic Consortium (BARC) criteria, major bleeding was defined as BARC types 3 or 5. In brief, type 3a bleeding events included overt bleeding plus a decline in hemoglobin (3g/dL to < 5g/dL) and any transfusion with overt bleeding. Type 3b bleeding events included overt bleeding plus a decline in hemoglobin of ≥ 5g/dL, cardiac tamponade, bleeding requiring surgical intervention for control, and bleeding requiring intravenous vasoactive agents. Type 3c bleeding events included intracranial hemorrhage, subcategories confirmed by autopsy, imaging, or lumbar puncture, and intraocular bleeding compromising vision. Type 5a bleeding events included probable fatal bleeding suspected clinically but with no autopsy or imaging confirmation. Type 5b bleeding events included definite fatal bleeding, overt bleeding, and autopsy or imaging confirmation.12 Moreover, bleeding events were evaluated by the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the American College of Cardiology/American Heart Association Guidelines (CRUSADE) bleeding score.13,14 The CRUSADE score was calculated based on baseline patient characteristics (female sex, diabetes, prior vascular disease, heart rate, systolic blood pressure, congestive heart failure, hematocrit value, and estimated creatinine clearance). The secondary endpoint was definite stent thrombosis, which was diagnosed as an acute coronary syndrome with angiographic documentation of either target vessel occlusion or thrombus, within or adjacent to the previously stented segment, applying the BARC definition.15 Cardiac death was considered as any fatal event not attributed to a noncardiac cause. Patients were followed up for ≥ 2 years after implantation.
Statistical AnalysisData are presented as mean (standard deviation) or as percentages. Differences between groups were assessed using unpaired 2-tailed Student t tests for continuous variables and chi-square tests for categorical variables. Survival analysis was performed using the Kaplan–Meier method and differences were assessed using the log rank test. Univariate and multivariate Cox proportional hazards models were used to assess independent correlates of major bleeding and stent thrombosis. All variables in Table 1 were entered into the models. Continuous variables were transformed into binary data with “1” representing the presence of an assumed risk factor and “0” as otherwise. For example, age was dichotomized as elderly or not elderly (> 75 years vs ≤ 75 years) and ejection fraction was dichotomized as low or normal (< 40% vs ≥ 40%). Moreover, to avoid arbitrariness, we used the median value of each continuous factor (body mass index, stent length, lesion length, etc.) as the cutoff point for this division. With regard to the SXscores, CRUSADE scores, heart rate, and glomerular filtration rate, the unit of measurement was designated as 10. Eventually, adjustment was performed to calculate hazard ratios (HRs) and 95% confidence intervals (95%CIs) with only clinically relevant variables that had P values of <.05 in the univariate analysis. Area under the receiver operating characteristic curve analysis was performed to determine the ability of the SXscore and CRUSADE score to distinguish between patients with and without major bleeding. A C statistic value > 0.7 was considered to have acceptable discriminatory capacity. All analyses were performed using the IBM-SPSS statistics version 19 and R package. A P value of < .05 was considered to indicate statistical significance.
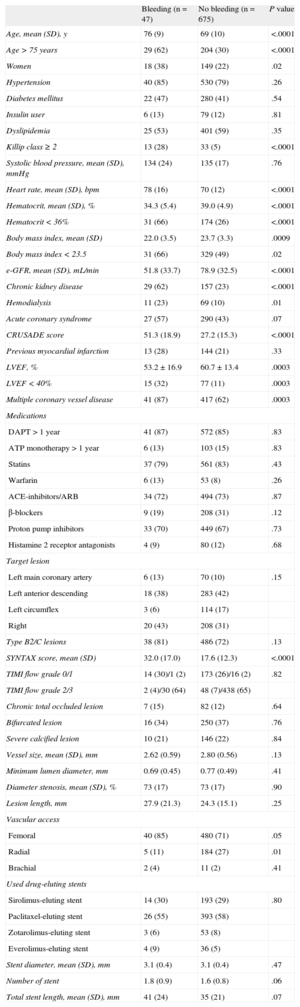
Baseline Patient, Angiographic and Procedural Characteristics With or Without Major Bleeding
| Bleeding (n=47) | No bleeding (n=675) | P value | |
| Age, mean (SD), y | 76 (9) | 69 (10) | <.0001 |
| Age > 75 years | 29 (62) | 204 (30) | <.0001 |
| Women | 18 (38) | 149 (22) | .02 |
| Hypertension | 40 (85) | 530 (79) | .26 |
| Diabetes mellitus | 22 (47) | 280 (41) | .54 |
| Insulin user | 6 (13) | 79 (12) | .81 |
| Dyslipidemia | 25 (53) | 401 (59) | .35 |
| Killip class ≥ 2 | 13 (28) | 33 (5) | <.0001 |
| Systolic blood pressure, mean (SD), mmHg | 134 (24) | 135 (17) | .76 |
| Heart rate, mean (SD), bpm | 78 (16) | 70 (12) | <.0001 |
| Hematocrit, mean (SD), % | 34.3 (5.4) | 39.0 (4.9) | <.0001 |
| Hematocrit < 36% | 31 (66) | 174 (26) | <.0001 |
| Body mass index, mean (SD) | 22.0 (3.5) | 23.7 (3.3) | .0009 |
| Body mass index < 23.5 | 31 (66) | 329 (49) | .02 |
| e-GFR, mean (SD), mL/min | 51.8 (33.7) | 78.9 (32.5) | <.0001 |
| Chronic kidney disease | 29 (62) | 157 (23) | <.0001 |
| Hemodialysis | 11 (23) | 69 (10) | .01 |
| Acute coronary syndrome | 27 (57) | 290 (43) | .07 |
| CRUSADE score | 51.3 (18.9) | 27.2 (15.3) | <.0001 |
| Previous myocardial infarction | 13 (28) | 144 (21) | .33 |
| LVEF, % | 53.2 ± 16.9 | 60.7 ± 13.4 | .0003 |
| LVEF < 40% | 15 (32) | 77 (11) | .0003 |
| Multiple coronary vessel disease | 41 (87) | 417 (62) | .0003 |
| Medications | |||
| DAPT > 1 year | 41 (87) | 572 (85) | .83 |
| ATP monotherapy > 1 year | 6 (13) | 103 (15) | .83 |
| Statins | 37 (79) | 561 (83) | .43 |
| Warfarin | 6 (13) | 53 (8) | .26 |
| ACE-inhibitors/ARB | 34 (72) | 494 (73) | .87 |
| β-blockers | 9 (19) | 208 (31) | .12 |
| Proton pump inhibitors | 33 (70) | 449 (67) | .73 |
| Histamine 2 receptor antagonists | 4 (9) | 80 (12) | .68 |
| Target lesion | |||
| Left main coronary artery | 6 (13) | 70 (10) | .15 |
| Left anterior descending | 18 (38) | 283 (42) | |
| Left circumflex | 3 (6) | 114 (17) | |
| Right | 20 (43) | 208 (31) | |
| Type B2/C lesions | 38 (81) | 486 (72) | .13 |
| SYNTAX score, mean (SD) | 32.0 (17.0) | 17.6 (12.3) | <.0001 |
| TIMI flow grade 0/1 | 14 (30)/1 (2) | 173 (26)/16 (2) | .82 |
| TIMI flow grade 2/3 | 2 (4)/30 (64) | 48 (7)/438 (65) | |
| Chronic total occluded lesion | 7 (15) | 82 (12) | .64 |
| Bifurcated lesion | 16 (34) | 250 (37) | .76 |
| Severe calcified lesion | 10 (21) | 146 (22) | .84 |
| Vessel size, mean (SD), mm | 2.62 (0.59) | 2.80 (0.56) | .13 |
| Minimum lumen diameter, mm | 0.69 (0.45) | 0.77 (0.49) | .41 |
| Diameter stenosis, mean (SD), % | 73 (17) | 73 (17) | .90 |
| Lesion length, mm | 27.9 (21.3) | 24.3 (15.1) | .25 |
| Vascular access | |||
| Femoral | 40 (85) | 480 (71) | .05 |
| Radial | 5 (11) | 184 (27) | .01 |
| Brachial | 2 (4) | 11 (2) | .41 |
| Used drug-eluting stents | |||
| Sirolimus-eluting stent | 14 (30) | 193 (29) | .80 |
| Paclitaxel-eluting stent | 26 (55) | 393 (58) | |
| Zotarolimus-eluting stent | 3 (6) | 53 (8) | |
| Everolimus-eluting stent | 4 (9) | 36 (5) | |
| Stent diameter, mean (SD), mm | 3.1 (0.4) | 3.1 (0.4) | .47 |
| Number of stent | 1.8 (0.9) | 1.6 (0.8) | .06 |
| Total stent length, mean (SD), mm | 41 (24) | 35 (21) | .07 |
ACE, angiotensin-converting enzyme; APT, antiplatelet therapy; ARB, angiotensin receptor blockers; CRUSADE, Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines; DAPT, dual antiplatelet therapy; e-GFR, estimated glomerular filtration rate; LVEF, left ventricular ejection fraction; SD, standard deviation; SYNTAX, SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery; TIMI: Thrombolysis In Myocardial infarction.
Data are expressed as No. (%) or mean (standard deviation).
The mean patient age was 69 years, 23% were female, 42% had diabetes mellitus, and 44% had acute coronary syndromes. Left main coronary disease and chronic total occluded lesions were each reported in 12% of patients. Most cases (87%) were treated with first generation DES. A potential range of the SXscore was 1.0-75.5, with a mean (standard deviation) of 18.5 (13.2) and a median of 15. The median value [interquartile range] of the CRUSADE score was 25 [18–38].
Patient CharacteristicsTable 1 shows the baseline clinical characteristics in the bleeding (n=47) and no bleeding (n=675) groups. The patients in the bleeding group were older, more often women, and were more likely to have a Killip class ≥ 2, multiple coronary vessel disease, and chronic kidney disease than patients in the no bleeding group. Body mass index, hematocrit value, and left ventricular ejection fraction in patients in the bleeding group were significantly lower than those in the no bleeding group. Furthermore, both the SXscores and CRUSADE scores were significantly higher in the bleeding group than in the no bleeding group. With the exception of transradial intervention, there was no significant difference in procedural factors between the groups.
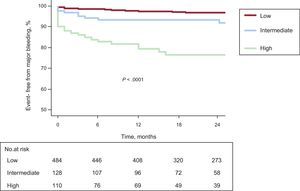
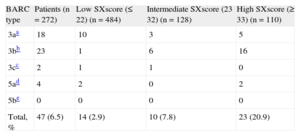
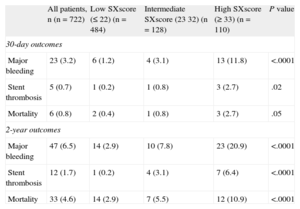
The SYNTAX Score and 2-year Clinical OutcomesComplete clinical follow-up data were available in 93% patients at 1 year and in 81% at 2 years. A total of 613 patients (84.9%) showed prolonged DAPT for up to 2 years following PCI. As shown in Table 2, patients were divided into 3 groups based on the original SYNTAX trial: low (≤ 22; n=484), intermediate (23-32; n=128), and high (≥33; n=110). Major bleeding according to BARC criteria was reported in 47 patients (6.5%; type 3a, n=18; type 3b, n=23; type 3c, n=2; type 5a, n=4; type 5b=0). With regard to the timing of bleeding complications, 23 patients (49%) experienced major bleeding within 30 days of the procedure, and the remaining 24 patients (51%) had major bleeding between 30 days and 2 years (Table 3). With regard to DAPT at the time of major bleeding, all 47 patients with major bleeding were receiving DAPT. On the other hand, stent thrombosis occurred in 12 patients (1.7%) within 2 years; of these, 3 were involved in antiplatelet therapy cessation. The mortality rates were 0.8% at 30 days and 4.6% at 2 years after PCI, respectively (Table 3). Figure 1 shows the survival curves for the patients who were free from major bleeding among the 3 SXscore tertiles. The 2-year incidence of major bleeding was 20.9% (n=23) among patients with high SXscores, 7.8% (n=10) among patients with intermediate SXscores, and 2.9% (n=14) among patients with low SXscores (Table 3). Similarly, stent thrombosis occurred more frequently among patients with high SXscores (6.4%; n=7) than those with intermediate (3.1%; n=4) or low (0.2%; n=1) SXscores (P < .0001). The area under the curve analysis also showed that the SXscore (C statistic = 0.751; 95%CI, 0.674-0.828; P < .0001) and the CRUSADE score (C statistic = 0.835; 95%CI, 0.774-0.897; P < .0001) had an adequate discriminatory capacity to distinguish between patients with and without major bleeding.
Incidence of Major Bleeding According to the Bleeding Academic Research Consortium Definition
| BARC type | Patients (n=272) | Low SXscore (≤ 22) (n=484) | Intermediate SXscore (23 32) (n=128) | High SXscore (≥ 33) (n=110) |
| 3aa | 18 | 10 | 3 | 5 |
| 3bb | 23 | 1 | 6 | 16 |
| 3cc | 2 | 1 | 1 | 0 |
| 5ad | 4 | 2 | 0 | 2 |
| 5be | 0 | 0 | 0 | 0 |
| Total, % | 47 (6.5) | 14 (2.9) | 10 (7.8) | 23 (20.9) |
BARC, Bleeding Academic Research Consortium; SXscore: SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery score.
Overt bleeding plus hemoglobin drop ≥ 5 g/dL, cardiac tamponade, bleeding requiring surgical intervention for control, and bleeding requiring intravenous vasoactive agents.
Clinical Outcomes at 30-day and 2-year Follow-up Among the 3 Groups
| All patients, n (n=722) | Low SXscore (≤ 22) (n=484) | Intermediate SXscore (23 32) (n=128) | High SXscore (≥ 33) (n=110) | P value | |
| 30-day outcomes | |||||
| Major bleeding | 23 (3.2) | 6 (1.2) | 4 (3.1) | 13 (11.8) | <.0001 |
| Stent thrombosis | 5 (0.7) | 1 (0.2) | 1 (0.8) | 3 (2.7) | .02 |
| Mortality | 6 (0.8) | 2 (0.4) | 1 (0.8) | 3 (2.7) | .05 |
| 2-year outcomes | |||||
| Major bleeding | 47 (6.5) | 14 (2.9) | 10 (7.8) | 23 (20.9) | <.0001 |
| Stent thrombosis | 12 (1.7) | 1 (0.2) | 4 (3.1) | 7 (6.4) | <.0001 |
| Mortality | 33 (4.6) | 14 (2.9) | 7 (5.5) | 12 (10.9) | <.0001 |
SXscore: SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery score.
Kaplan-Meier curves depicting the survival from major bleeding according to the SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery scores. Patients were divided into the following groups according to the original SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery trial: low (≤ 22), intermediate (23-32), and high (≥ 33).
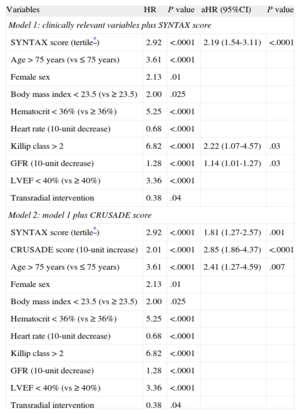
The Cox proportional hazards model was used to identify independent predictors of 2-year major bleeding and stent thrombosis. Baseline variables listed in Table 1 that differed between groups with a P value of < .05 were entered into the model. As shown in Table 4, model 1 with clinically relevant variables and the SXscore identified the SXscore as an independent correlate of 2-year major bleeding (HR = 2.19; 95%CI, 1.54-3.11; P < .0001 for the SXscore tertile). Also, model 2, which was the addition of the CRUSADE score to model 1, demonstrated that both the SXscore and the CRUSADE score were independent predictors of major bleeding.
Two Models of Cox Proportional Hazards Analyses for 2-year Major Bleeding
| Variables | HR | P value | aHR (95%CI) | P value |
| Model 1: clinically relevant variables plus SYNTAX score | ||||
| SYNTAX score (tertile*) | 2.92 | <.0001 | 2.19 (1.54-3.11) | <.0001 |
| Age > 75 years (vs ≤ 75 years) | 3.61 | <.0001 | ||
| Female sex | 2.13 | .01 | ||
| Body mass index < 23.5 (vs ≥ 23.5) | 2.00 | .025 | ||
| Hematocrit < 36% (vs ≥ 36%) | 5.25 | <.0001 | ||
| Heart rate (10-unit decrease) | 0.68 | <.0001 | ||
| Killip class > 2 | 6.82 | <.0001 | 2.22 (1.07-4.57) | .03 |
| GFR (10-unit decrease) | 1.28 | <.0001 | 1.14 (1.01-1.27) | .03 |
| LVEF < 40% (vs ≥ 40%) | 3.36 | <.0001 | ||
| Transradial intervention | 0.38 | .04 | ||
| Model 2: model 1 plus CRUSADE score | ||||
| SYNTAX score (tertile*) | 2.92 | <.0001 | 1.81 (1.27-2.57) | .001 |
| CRUSADE score (10-unit increase) | 2.01 | <.0001 | 2.85 (1.86-4.37) | <.0001 |
| Age > 75 years (vs ≤ 75 years) | 3.61 | <.0001 | 2.41 (1.27-4.59) | .007 |
| Female sex | 2.13 | .01 | ||
| Body mass index < 23.5 (vs ≥ 23.5) | 2.00 | .025 | ||
| Hematocrit < 36% (vs ≥ 36%) | 5.25 | <.0001 | ||
| Heart rate (10-unit decrease) | 0.68 | <.0001 | ||
| Killip class > 2 | 6.82 | <.0001 | ||
| GFR (10-unit decrease) | 1.28 | <.0001 | ||
| LVEF < 40% (vs ≥ 40%) | 3.36 | <.0001 | ||
| Transradial intervention | 0.38 | .04 | ||
95%CI, 95% confidence interval; aHR, adjusted hazard ratio; CRUSADE, Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines; GFR, glomerular filtration rate; HR, hazard ratio; LVEF, left ventricular ejection fraction; SYNTAX, SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery.
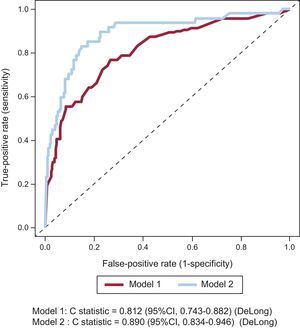
The predictive value of the SXscore and the CRUSADE score with regard to major bleeding was assessed by calculating the adjusted area under the receiver operating characteristic curve in multivariate models 1 and 2. The adjusted areas under the curve of models 1 and 2 demonstrated adequate discriminatory capacities to distinguish between patients with and without major bleeding (model 1: C = 0.812; model 2: C = 0.890) (Figure 2). However, model 2, which added the CRUSADE score, significantly improved the C statistic for predicting major bleeding compared with model 1 (z test=−257, P=.01).
Adjusted receiver operating characteristic curves for predicting 2-year major bleeding by model 1 and model 2. 95%CI, 95% confidence interval. Model 1: clinically relevant variables plus SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery score. Model 2: model 1 plus Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines score.
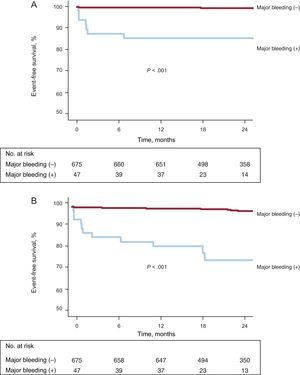
Independent predictors of 2-year stent thrombosis were the SXscore (tertile; HR=4.39; 95%CI, 2.02-9.50; P=.0002) and severe calcified lesion (HR=3.97; 95%CI, 1.26-12.52, P=.02). According to the presence of major bleeding, the event-free survival curves in Figure 3A and 3B indicate that patients with major bleeding had a significantly higher incidence of cardiac death (14.9% vs 1.0%; P<.0001) and of all-cause death (23.4% vs 2.5%) at 2 years.
DISCUSSIONThe present study is the first to evaluate the SXscore as a predictor of major bleeding according to BARC criteria in an all-comers cohort undergoing DES implantation. The following are the major findings of this study: a) the SXscore was significantly associated with an increased risk of 2-year major bleeding following PCI. However, the CRUSADE score had a higher predictive value for major bleeding than the SXscore in our study population. A higher SXscore was an independent predictor of 2-year major bleeding, even after adjustment for clinical variables. As expected, patients with major bleeding were significantly associated with an increased risk of cardiac death and all-cause death at 2 years, b) a higher SXscore was also associated with increased stent thrombosis during 2-year follow-up, although the CRUSADE score failed to predict the development of stent thrombosis.
Bleeding complications following DES implantation remain a challenging issue.1 Concern regarding late adverse thrombotic events, particularly very late stent thrombosis, has prompted the use of extended DAPT and more potent antiplatelet drugs.4 However, aggressive antiplatelet regimens and prolonged DAPT are associated with an increased risk of bleeding complications.5 Therefore, considering the increased bleeding risk, the current antiplatelet regimens must be administered with caution. Bleeding complications may lead to fatal events or at least lead to the discontinuation of antiplatelet therapy, which may increase the risk of thrombotic events. The present study revealed a higher incidence of 2-year mortality in patients with major bleeding. Consistent with our findings, a previous meta-analysis of 4 randomized trials demonstrated that bleeding following PCI had a prognostic impact on mortality within 1 year of the procedure.16
The most widely accepted bleeding score, CRUSADE, was calculated based on baseline patient characteristics and laboratory values, whereas the relationship between bleeding complications and lesion complexity has not been well studied in patients undergoing DES implantation and DAPT.13 The SXscore is a new angiographic tool that can quantify the degree of atherosclerosis in the entire coronary artery tree, including the culprit lesions.10 In the present study, we observed a relationship between higher SXscores and major bleeding risk. Although the reason why a high SXscore was related to an increased major bleeding risk remains unclear, this association may be explained by the longer procedural time and more complicated procedures required in patients with more extensive and complex coronary atherosclerosis, which would be expected to increase the risk of bleeding. In fact, in the present study, approximately half of the bleeding complications were observed within 30 days of the procedure. However, after 30 days, the number of patients with major bleeding gradually increased until 2 years. With regard to this result, the duration of DAPT required to reduce the incidence of bleeding complications after DES implantation is still a matter of debate.
Appropriate Balance of Major Bleeding and Stent Thrombosis Risks Among the 3 GroupsRegarding the risk of thrombotic events such as stent thrombosis and myocardial infarction, registries and observational studies have demonstrated that DAPT is not required beyond 6 months.17,18 The PRODIGY trial also demonstrated that the extended use of DAPT was associated with a higher rate of bleeding events and blood transfusions, without the protective effects of reducing the risk of thrombotic events.19 We observed that the incidence of stent thrombosis was very low among patients with low and intermediate SXscores. Therefore, such low-risk patients should be switched from DAPT to antiplatelet monotherapy, including low-dose acetylsalicylic acid, as soon as possible to avoid bleeding complications. On the other hand, patients with a high SXscore in the present study had significantly higher incidences of both major bleeding and stent thrombosis. In other words, in PCI in patients with a high SXscore, we may still face the unresolvable dilemma of whether to continue DAPT beyond 12 months after PCI.20 Therefore, the SYNTAX trial results along with the present findings suggest that patients with high scores and adequate distal vessel beds may be more appropriate candidates for coronary artery bypass grafts, with the exception of those with a high surgical risk and feasible PCI. Currently, many randomized clinical trials examining the optimal duration of DAPT following DES implantations are ongoing.21–23 To determine whether the duration of DAPT needs to continue beyond 6 or 12 months following PCI, it will be necessary to wait for the results of these trials.
LimitationsThe present study has several limitations. First, it was a single center study with a small sample size. However, to the best of our knowledge, no other studies have evaluated major bleeding following DES implantation using the BARC criteria and SXscores. The results may have been influenced by confounding factors. For example, decisions regarding DAPT duration may have differed among the attending physicians. Notably, in our study, many patients (84.9%) were treated with DAPT for up to 2 years after implantation; this number seems to be high. The reason might have been related to a concern about the development of very late stent thrombosis with first generation DES use. Furthermore, we did not use a glycoprotein IIb/IIIa inhibitor, prasugrel, and bivalirudin. Although 8% of patients in our study were on triple anticoagulation therapy, including warfarin, there was no difference in bleeding complications. Perhaps the expected effect of warfarin was decreased when the patients received DAPT.
CONCLUSIONSThe SXscore had a predictive ability for patients at major bleeding risk in the all-comers population undergoing DES implantation. Also, the CRUSADE score had a higher predictive value for major bleeding than the SXscore. Therefore, these scores may be useful for clinical decision making regarding the optimal DAPT duration following DES.
Furthermore, we observed that a high SXscore was associated with increased risks of major bleeding and stent thrombosis. At present, careful consideration by a heart team is warranted when revascularization strategies such as PCI or bypass surgery are needed in patients with high SXscores. If a revascularization strategy with PCI is performed in a high SXscore subset, DAPT should be administered after careful consideration of the critical balance between the risks of thrombotic events and major bleeding in individual patients.
CONFLICTS OF INTERESTNone declared.