Keywords
INTRODUCTION
Permanent right ventricular apex pacing can have undesirable effects1-4 and the outflow tract is not a clear alternative.5
His bundle pacing (HBP) produces physiologic ventricular contraction with no negative effect on ventricular function.6-9
We aim to determine how many patients indicated for permanent cardiac pacing would be candidates for HBP and in how many this is achieved.
METHOD
Selection of Patients
From January to July 2006, patients without cardiomyopathy and proposed for cardiac pacing were considered potential candidates for HBP regardless of block type. Due to pressure of healthcare concerns, we selected 1 in 3 consecutive patients. We obtained informed consent.
To be a candidate for HBP we required: indication for permanent cardiac pacing10; maximum Hisian capture threshold 2.5 V/1 ms; 1:1 His ventricle conduction with minimum 120 s/m; and absence of cardiomyopathy.
Location and Temporary His Bundle Pacing
For location and temporary and definitive HBP, we employed active fixation, low polarization Tendril SDX electrodes (St Jude, Minneapolis), 52 cm long with 1 cm between poles, following a previously published technique.11,12
Additional Electrode and Generators Used
In patients with intraventricular conduction disturbance (IVCD) or complete "infra-Hisian" atrioventricular block (CAVB) (His bundle electrogram with H not followed by V), as well as the His bundle electrode, we implanted a backup device in the right ventricle outflow tract (Figure 1C).
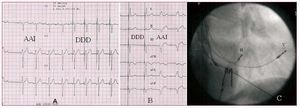
Figure 1. A: type I second-degree supra-Hisian block, treated with DDD pacemakers with His bundle pacing (HBP); pure capture of His. B: first-degree atrioventricular block with left branch block treated with DDD pacemakers for HBP; trunk type behavior; pure capture of His. C: oblique right anterior projection; intraventricular conduction disturbance treated with 3-chamber pacemakers, atrial electrode (A), His (H), and right outflow tract (V).
Depending on specific clinical situations, the pacemakers used were Frontier II 5596 3-chamber (St. Jude Medical, Sylmar, California, US), Kappa 900 dual-chamber (Medtronic, Minneapolis, Minnesota, US), or Insignia I AVT SR single-chamber devices (Guidant Corporation, St. Paul, Minnesota, US) (Figures 1A and B).
RESULTS
We selected 37 patients with conduction disturbances (Table 1) but excluded 6: 3 with CAVB and wide escape in whom we could not record Hisian deflection; and 3 with left branch block (LBB) not corrected by HBP. In the remaining 31 (83.3%) patients, conduction abnormalities were corrected by HBP; 15 (71.4%) had infra-Hisian disturbances (IVCD or CAVB) (Table 2).
The acute HBP threshold was 0.6-9 (3.1 [2.8]) V in 1 ms in the 31 patients; 11 (35.4%) were rejected due to a high threshold. No patient was excluded for 1:1 His-ventricle conduction <120 s/m. Finally, 20 patients met requirements for permanent HBP. In 9 (45%) the electrode could not be fixed. In the other 11 (55%), it was fixed successfully (Table 2) (threshold, 1.5 [0.9] V; impedance, 293 [103] W) and we achieved pure HBP in 6 and fused HBP in 5.
His Bundle Pacing Patterns
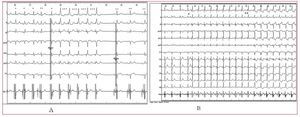
In patients with supra-Hisian block we found 2 QRS patterns. Type 1 presented latency lasting £HV interval and QRS with morphology and repolarization identical to the conduction or escape patterns (Figure 2A). Type 2 lacked latency, QRS morphology and repolarization differed and "prepacing" appeared (Figures 2A and B).
Figure 2. A: QRS marked * are pure capture of His, equal to the other (**); QRS marked *** are fused. B: His pacing with progressive descent in voltage from *; up to ** are fusion complexes. After ** capture of His is lost.
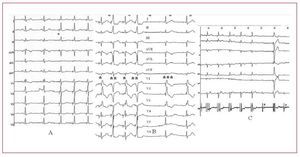
In the so-called "infra-Hisian" IVCD and CAVB we found 3 QRS patterns: A, latency with disappearance of IVCD/CAVB and normalization of QRS (Figures 1B and 3A and C); B, latency and persistence of IVCD (Figure 3B); and C, absence of latency with disappearance of IVCD without normalization of QRS (Figure 3B).
Figure 3. A: right bundle branch block disappearing with His bundle pacing (HBP) in *; trunk type behavior. B: right bundle branch block in ***, persisting with HBP in *; peripheral type behavior; QRS marked with ** are fusion. C: complete "infra-Hisian" atrioventricular block; HBP produces normal QRS; trunk type behavior. H indicates His bundle electrogram.
DISCUSSION
In our series, 83.3% of conduction disturbances requiring permanent cardiac pacing were corrected with HBP. However, permanent HBP was achieved in only 35.5% of possible cases and 55% of attempts.
In patients with supra-Hisian block, the type 1 pattern is due to "pure" HBP and leads to normal QRS because the impulse is conducted via the Purkinje system. Latency reflects the time of conduction from the region of Hisian capture to that of ventricular activation. The type 2 pattern may be explained by simultaneous capture of His and the adjacent myocardium, producing fusion between the 2 sites of activation, which explains the image of "prepaced" QRS and absence of latency.
In IVCD, HBP is known to cause branch block to disappear. However, cases of HBP producing normal QRS in the presence of "infra-Hisian" CAVB (Figure 3C) have not been reported. The theoretical longitudinal disassociation of the His bundle13-16 explains these phenomena: fibers assigned to the right and left branches would be histologically differentiated and isolated in the Hisian trunk. A lesion here can harm them and in the ECG this would appear as complete atrioventricular branch block. Pacing of the region distal to the lesion would normalize QRS.
Thus, "infra-Hisian" IVCD and CAVB could be classified by their location in the (His bundle) trunk and peripheries, depending on whether or not they disappear with HBP. Pattern A would be produced in the presence of trunk IVCD, when Hisian capture is "pure" and distal to the region of block; ventricular depolarization occurs via the Purkinje system, which explains QRS normalization with latency. Pattern B is justified by peripheral IVCD with "pure" HBP, which explains the persistent IVCD with latency. Pattern C would be a "fusion" due to capture of the His and the adjacent myocardium. Right ventricular prepacing would occur, causing loss of latency and the disappearance of right bundle branch block (RBBB), regardless of whether it is located in the trunk or periphery.
In the presence of LBB, pattern C would only occur in trunk location. The QRS would be a fusion of His and myocardium capture. The former would cause ventricular activation to disappear via the Purkinje system, explaining the disappearance of LBB. The latter, right ventricular prepacing, explains the loss of latency and absence of QRS normalization.
On its own, neither "pure" nor "fused" HBP should produce left intraventricular asynchrony and their use is limited due to the high capture threshold that eliminates, given a prior attempt at deployment, more than one third of candidates, or to difficulties in electrode placement, leading to failure in 45% of attempts.
In conclusion, permanent HBP can be considered when definitive cardiac pacing is required. New electrodes that improve capture and stability are needed. Moreover, the uncertain evolution of "infra-Hisian" IVCD and CAVB increases the complexity and cost of HBP.
Correspondence: Dr. R. Barba Pichardo.
A. Sundheim, 30. 1.o C. 21003 Huelva. España.
E-mail: rbphuelva@Yahoo.es
Received August 24, 2007.
Accepted for publication January 17, 2008.