INTRODUCTION
One of the main challenges in percutaneous coronary intervention is to limit the rate of restenosis and the subsequent need for revascularization of the vessel. When multivessel percutaneous revascularization is compared with coronary artery bypass surgery, the need for further revascularization accounts for the most of the difference in the rate of events between the two approaches during follow-up.1 The studies that have been performed so far with drug-eluting stents (paclitaxel and rapamycin) have shown a substantial decrease in restenosis and subsequent need for further revascularization in previously treated lesions.2-7 Nevertheless, these large studies did not include patients who were at higher risk of restenosis with bare metal stents, such as those with total occlusions, in-stent restenosis, very long lesions (>30 mm) or those in vessels less than or equal to 2.5 mm. Studies of small retrospective series of patients with such lesions have been published in which different models of drug-eluting stent were used and in which some very promising results were obtained.8-16
Similarly, no studies have been performed that compare the efficacy and safety of the 2 stents. If there were some difference between the 2 stents, this could be detected more easily in patients with more complex lesions. Thus, in the present study, we compared the clinical course of 2 groups of patient with a similar complex lesion profile treated with paclitaxel-eluting stents (PES) or rapamycin-eluting stents (RES). As a control, we included a third comparable group treated with bare metal stents (comprising our experience with patients treated immediately prior to the introduction of drug-eluting stents).
PATIENTS AND METHODS
We included patients referred to our unit with the clinical indications for coronary angiography who were candidates for percutaneous revascularization and whose lesions (all or at least one) met at least one of the following criteria:
1. In-stent restenosis.
2. Total occlusion however long it has been present.
3. Diffuse lesion (>20 mm).
4. Small vessel lesion (≤2.5 mm).
Treatment periods:
1. From October 2001 to May 2002, the patients were treated with bare metal stents.
2. From June to December 2002, 72% of the lesions that met at least one of the above criteria were treated with RES, Cypher®. The remaining lesions were treated with bare metal stents, whether because RES of the appropriate size were not available or because the lesion profile was more favorable (focal lesions in 2.5 mm vessels or diffuse lesions of 20-25 mm in vessels ≥3 mm). All total occlusions and in-stent restenoses were treated with RES.
3. From April to December 2003, 70% of the lesions that met at least one of the above criteria were treated with PES, Taxus®. The remaining lesions were treated with bare metal stents (on specific occasions) or with RES due to the availability of stents of the appropriate size or because a member of the team used RES more often (for purely logistic reasons).
For each period, the first 100 consecutive cases treated with the corresponding stent were included. The results of the series of patients treated with RES alone have already been published separately in this journal.16
Patients who underwent primary angioplasty and those who were in cardiogenic shock were excluded. Patients with occlusions were only included if stent placement was possible. Whether the stent was implanted directly or not was left to the discretion of the surgeon, though direct placement was not attempted in any of the patients with complete occlusion, those needing a long stent (>23-24 mm) and when vessel calcification or marked bending or twisting was evident. Digital quantitative coronary angiography was done after the procedure.
The femoral approach was used for implantation and, in all cases, vascular closure devices were used. The use of glycoprotein IIb/IIIa inhibitors was left to the discretion of the surgeon. Angiographic success was defined as residual stenosis less than 25% with TIMI flow III. Enzyme measurements were only done in patients in whom there was clinical or electrocardiographic suspicion of necrosis after the percutaneous transluminal coronary angioplasty (PTCA) (procedural complication, ischemia and/or post-PTCA symptoms). All patients received an oral dose of 300 mg of clopidogrel immediately after the procedure, and subsequently a combination of 100 mg of aspirin and 75 mg of clopidogrel for 3 months in the case of RES and 6 months in the case of PES.
Clinical follow-up consisted of a clinical visit 6 to 12 months after the procedure and, an additional telephone call in which the investigator spoke directly with the patient. To compare the clinical course of the 3 consecutive series, we finished follow-up of each group when the last patient had been followed for 6 months. Thus, the length of follow-up was similar in the 3 groups (mean, 8-9 months; range, 6-12 months). Patients were assessed by their corresponding clinical cardiologists, who indicated tests for ischemia or coronary angiography as they saw fit. Events were classified as:
1. Death (cardiac or noncardiac).
2. Q-wave myocardial infarction defined by the appearance of new Q-waves in the electrocardiogram (ECG), whether or not preceded by clinical symptoms, or non-Q-wave myocardial infarction defined as acute coronary syndrome associated with enzymatic elevation (more than twice the upper limit of normal for the creatine kinase MB isozyme [CK-MB]) without subsequent appearance of Q-waves in the ECG.
3. Stent thrombosis defined as angiographic observation of total or partial occlusion of the stent by thrombotic material preceded by acute clinical signs and symptoms with possible ST-segment elevation.
4. Revascularization, which may have been done in the treated lesion (due to in-stent restenosis) or in a new lesion.
Statistical Analysis
Continuous variables were presented as means ±SD. Categorical variables were expressed as percentages. The continuous variables were compared using the Student t test if the distribution was normal and using the Wilcoxon test if the distribution was not normal (according to the normal distribution test of Kolmogorov-Smirnov). Categorical variables were compared with the χ² test or the Fisher exact test, depending on which was appropriate. All variables were compared for the 2 groups of drug-eluting stent and for these groups and the control group. Kaplan-Meier event-free survival curves were obtained for each group and compared by the logrank test. Statistical significance was set at P<.05. The SPSS 11.0 statistical package was used.
RESULTS
The first 100 consecutive patients from each treatment period with the corresponding type of stent were included. From October 2001 to May 2002, 100 patients with 170 lesions were treated with bare metal stents. Of these lesions, 117 (69%) met the selection criteria. From June to December 2002, 100 patients from the RES group were treated with Cypher® stents, corresponding to 154 lesions, of which 109 (71%) met the selection criteria. From April to December 2003, 100 patients from the PES group were treated with Taxus® stents, corresponding to 164 lesions, of which 118 (72%) met the selection criteria. Placement of drug-eluting stents was successful whenever the procedure was attempted.
The clinical characteristics of the 3 groups of patient are shown in Table 1. The only significant differences were seen in the rate of previous surgical bypass operations, which was higher in the RES group than in the group with bare metal stents, and in prior statin treatment. Statin treatment was more widespread in the PES group because statin use has increased over the study period (the PES group were the most recently treated patients). Nevertheless, treatment with statins during follow-up was very similar in both groups.
The angiographic characteristics of the lesions of each group are described in Table 2. In all groups, a similar proportion of lesions met the criteria outlined in the previous section (69% in the group with bare metal stents, 71% the RES group and 72% in the PES group). The distribution of type of lesion was comparable, although a trend toward a lower rate of in-stent restenosis requiring treatment was seen in the PES group. The characteristics of the procedure were likewise very similar, though worthy of mention is the trend toward longer total stent lengths per patient in the drug-eluting stent groups compared to the group with bare metal stents. This difference was significant for comparison of the PES group with the group who received bare metal stents (Table 3). The angiographic success was fully comparable among all 3 groups.
Procedural and in-Hospital Complications
Two non-Q-wave myocardial infarctions occurred in the RES group (2%). One of these was due to an occlusive retrograde dissection after stent placement in the right medial coronary artery and resolved without additional further stenting. The other was due to untreatable occlusion of a small diagonal branch (<2 mm diameter) after stenting of the left anterior descending artery. A transient ischemic attack occurred in 1 66-year-old male hypertensive patient (1%) (Table 4).
In the PES group, a non-Q-wave myocardial infarction due to lack of reperfusion was reported after stenting. Two patients suffered stent thrombosis which presented as ST-segment elevation myocardial infarction. In 1, who received a 2.5/8 mm stent within a stent due to distal restenosis of the left anterior descending artery, thrombosis occurred after 3 hours. In the other, who received a 2.57/32 mm stent implanted in the medial left anterior descending artery, thrombosis occurred 24 hours after the procedure. Neither patient received abciximab during the procedure. In these cases, the distal bed was in poor condition and showed diffuse disease. A second percutaneous coronary intervention was performed with abciximab (thrombus aspiration and balloon dilatation), with a satisfactory outcome.
Two non-Q-wave myocardial infarctions were reported in the group with bare metal stents. These events were related to unresolved occlusion of 2 small diagonal branches (≤2 mm) after treatment of side-branch occlusions.
Clinical Follow-up
All patients in the RES and PES groups and 99% of the patients in the group with bare metal stenting underwent clinical follow-up.
In the RES group, no deaths occurred during 8.5±2 months (range, 6-12 months) of follow-up and 2 patients (2%) had late thromboses, 1 of which led to Q-wave myocardial infarction (Table 4). Thrombosis occurred after 3.5 months in 1 patient with a 2.75/33 mm stent implanted to treat an occlusive and diffuse in-stent proximal restenosis of the left anterior descending artery, with diffuse disease in a distal bed and extensive collateral circulation from the right coronary artery. Competitive flow from this collateral circulation was present even after stenting. The signs and symptoms of thrombosis were unstable angina but without enzymatic elevation due to the aforementioned collateral circulation. The second case occurred 7 months after placement of a 3/33 mm stent in a proximal de novo lesion of the left anterior descending artery, with 50% occlusion at a side branch. The patient with clinical restenosis requiring repeat PCTA had type-1 diabetes and severe, multivessel diffuse coronary artery disease and she had initially received 92 mm of stents in 3 vessels. Coronary angiography, done 5 months after the procedure because of recurrence of symptoms, showed 2 severe in-stent restenotic lesions, 1 in the left anterior descending artery and 1 in the circumflex artery, both of which were focal (<5 mm) and located away from the ends of the stent. During follow-up, 3 revascularization procedures (3%) were performed on a treated lesion, 2 of which corresponded to late thrombosis (Table 4). Another patient underwent angioplasty for a new lesion. At the end of follow-up, only 2 patients (2%) presented symptoms compatible with class II stable angina, but they were not referred for a further angiographic studies because their symptoms could be controlled satisfactorily by medical treatment.
In the PES group, with follow-up lasting 9±2.5 months (range, 6-14 months), 1 patient died of a noncardiac cause (accidental fall). No new stent thrombosis was reported and 2 patients presented non-Q-wave myocardial infarction (2%). One patient (1%) presented clinical restenosis that required percutaneous revascularization and 2 patients (those who had presented non-Q-wave myocardial infarctions) underwent revascularization of new lesions. In 1 of these patients, restenosis of the PES that bordered on angiographic significance (50%) was seen. The lesion was assessed with a pressure guide and a fraction flow reserve (FFR) of 0.85 was obtained, so other severe lesions in another vessel related to the clinical signs and symptoms were treated. At the end of follow-up, 3 patients (3%) had class II stable angina that was controlled with medical treatment and a further 3 had presented 1-2 episodes of brief self-limiting chest pain during the whole follow-up period. The only case of revascularization of a treated lesion corresponded to a patient who had received a 3/24 mm stent in the proximal left anterior descending artery without covering the ostium, which was not affected. After 11 months, a new catheterization procedure was performed for unstable angina and a severe lesion in the ostium of the left anterior descending artery was observed (within 5 mm of the end of the stent).
In the group treated with bare metal stents, with a follow-up of 8±2 months (range, 6-12 months), no deaths were reported and 1 subacute thrombosis occurred (1%), but there were no late thromboses. Two Q-wave myocardial infarctions (2%) and 1 non-Q-wave myocardial infarction (1%) occurred. Revascularization of a treated lesion was undertaken in 15 patients (15%) because of clinical restenosis. Three patients (3%) underwent revascularization of new lesions, and 1 of these required coronary artery bypass graft. At the end of follow-up, 6 patients (6%) presented stable class II angina.
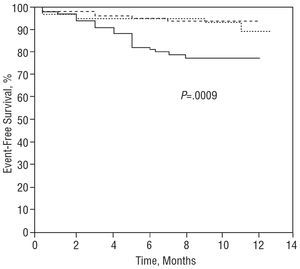
The event-free survival curves (all-cause mortality, infarction, and all revascularizations) are shown in the Figure. The curves for the RES and PES groups were similar and significantly better than the group treated with bare metal stenting. Table 5 shows the rate of repeat interventions due to restenosis by lesion type. Given that the 2 groups had different rates of statin treatment prior to the procedure, that is, those treated with bare metal stents were less exposed to statins, the influence of baseline treatment on incidence of revascularization of the treated lesion in this group was analyzed, but no significant differences were found (16% without statins, 14% with statins).
Figure. Kaplan-Meier event-free survival curves (all-cause mortality, infarction or revascularization) for the 3 groups: BMS (solid line), PES (dotted line), and RES (broken line). P=.002 for comparison RES vs BMS and P=.004 for the comparison PES vs BMS.
DISCUSSION
The large studies done so far with RES and PES have only assessed lesions with slight or moderate risk of restenosis. Patients with lesions less than 30 mm, total obstructions, ostial lesions, lesions requiring stents with diameters less than 2.5 mm or in-stent restenosis have been excluded. In these types of lesion, the effectiveness of drug-eluting stents is not completely known, although series have been published that suggest a good outcome.8-16
Drug-eluting stents may be most beneficial in these types of lesion because clinical restenosis with bare metal stents is high (10%-30%),17-28 but studies have yet to be done that compare the efficacy and safety of the 2 types of drug-eluting stent. Clinically relevant differences in the outcomes of the 2 types of stent, if they do exist, would be more readily detected in high-risk lesions.
We therefore undertook this study in which we compared 3 types of treatment for the same lesion profile (diffuse lesions, lesions in small vessels, complete occlusion, and in-stent restenosis). The groups were consecutive because RES and PES were not introduced at the same time. The clinical and angiographic characteristics of the patients were very similar. The only difference of note was less in-stent restenosis in the PES group because RES had been introduced before study of the PES group, thus notably reducing in-stent restenosis. The lower incidence of restenosis in the group with bare metal stents compared to the RES group can be explained by a greater tendency for these patients to be referred for bypass surgery when drug-eluting stents were not available or for balloon-only treatments, which were more common at the time. These, then, were high-risk groups with a high rate of multilesion and multivessel revascularization and prior procedures.
Stent Thrombosis
With regard to safety, the overall incidence of stent thrombosis was similar but thrombosis occurred at different times. The incidence of thrombosis with drug-eluting stents (2%) lies within acceptable ranges, bearing in mind that this was not a general series patients but rather a selected series with more complex lesions. One patient treated with PES had acute thrombosis and another treated with PES had late thrombosis. Both patients had something in common, namely, suboptimal flow in the diseased distal bed. Moreover, both patients underwent in-stent placement of drug-eluting stents. Abciximab was not used in the patient with acute thrombosis. The case of late thrombosis occurred 3 months after the procedure within 3 days of suspending treatment with clopidogrel, suggesting that a combined treatment of aspirin-clopidogrel for longer than 3 months, and maybe for as long as 6 months, is indicated in patients at highest risk (for example, very long or multiple stents or in-stent restenosis).
Need for Repeat Revascularization
In high-risk patients, the rate of new revascularization in target lesions during follow-up for both groups of drug-eluting stent is doubtlessly a spectacular finding. Likewise, the lower prevalence of symptoms of stable angina in the event-free patients is also an important finding. These results would be good even for a patient population with unselected lesions. The findings in the drug-eluting stent groups contrast with that observed in the group receiving bare metal stents, in which the need for repeat procedures was significantly higher.
The findings may appear too good--the differences are even higher than those reported in randomized trials and higher than the experience of other centers.2-14 First, it could be argued that the lesions selected for treatment with drug-eluting stents might have been less complex, but the opposite is in fact true; there was a selection bias against the groups treated with drug-eluting stents. The patients who received such stents were those with the highest risk of restenosis and only those with lesions that met only 1 risk criterion (diffuse lesion or small vessel lesion, but not both) were given a bare metal stent. No patients receiving bare metal stents had complete occlusion or in-stent restenosis. Thus, the lesion profile might have been even more adverse in the groups who received drug-eluting stents.
Second, it might be argued that there is a bias toward lower repeat catheterization in the RES and PES groups, but the rate of repeat intervention in the group treated with bare metal stenting is just as low as that reported for other series of patients receiving bare metal stents.17-28 Direct and independent evaluation of the clinical state of the patients at the end of follow-up confirms that this is the case, as only 2 patients in the RES group and 3 in the PES group presented class II stable angina at the end of follow-up. The real reasons for the lower rate of repeat intervention in the 3 groups compared to studies and series in other centers are as follows:
- In the randomized studies, it has been shown that angiographic follow-up increases the rate of revascularization with respect to clinical follow-up only.29 Angiographic follow-up therefore does not reflect clinical impact, as angiography detects either clinically silent restenosis or restenosis leading to stable angina that is readily controlled by medical treatment. These findings suggest that revascularizations are performed that would never have been done in clinical practice. These observations are also applicable to studies with drug-eluting stents where many of the revascularization events coincide with when angiographic follow-up was done.30
- With regard to the experience of other centers, clinical cardiologists in Spain are not as predisposed to intervention as in other countries (particularly the United States and Western Europe).31 This affirmation is supported by 2 observations. First, a significantly lower number of coronary angiograms are performed per million inhabitants and, second, stable angina or postsurgical angina figures notable less often among the indications for coronary angiography in Spain. This would explain why fewer repeat catheterizations are done in Spain in patients who only have class I or II stable angina that is controlled medically.31
Antiplatelet Treatment
The duration of antiplatelet treatment varies according to the study and the stent used. Treatment lasted 6 months in studies with PES5-7 and 2-3 months in studies with RES.2-4 In our series, patients with RES were treated for 3 months and those with PES were treated for 6 months. A period of up to 6 months of treatment (given empirically) is probably recommended for both types of stent in patients with in-stent restenosis, a long stent, or multiple stents. The cases of late thrombosis described in the RES group support this approach, and we currently also take this approach.
Limitations
This was an observational study that describes the results obtained in selected consecutive, series of patients. These patients were not randomized and angiographic monitoring was not done, which detracts from the findings of the study. Nevertheless, we stress that the study was done in the clinical practice setting. This study aimed to investigate and compare the impact that these new stents have within clinical practice on safety (incidence of thrombosis) and decreased need for repeat interventions, as well as on the clinical state of the patients at the end of a reasonable clinical follow-up. The direct and independent assessment of the clinical state of the patients at the end of follow-up confirms that the low need for repeat revascularization was realistic, as only 2 patients in the RES group and 3 in the PES group had class II stable angina.
A further limitation was that we did not systematically determine enzyme levels after the procedure in all patients (such determinations were only done in complicated cases), thus we have no information on the incidence of procedural necrosis in noncomplicated cases. In this respect, our group have recently assessed the incidence of elevated troponin I levels in consecutive series of patients treated with bare metal stents (200 patients) and RES (100 patients) in patients with noncomplicated lesions. We found no significant differences (15% vs 19%, respectively), despite a more adverse lesion profile in the group treated with RES.32
CONCLUSIONS
Use of RES and PES in lesions at high risk of restenosis (diffuse lesions, vessel ≤2.5 mm, complete occlusion and in-stent restenosis) seems to be as safe as bare metal stents and more effective. Given the aforementioned limitations of this study, larger series with randomized comparisons are needed to be more certain of these findings.
Models that predict restenosis are, however, difficult to construct,33 so the main contraindication to more widespread use will probably continue to be the ever-present dispute about costs, at least for the foreseeable future.34
Correspondence: Dr. J.M. de la Torre Hernández.
Unidad de Hemodinámica y Cardiología Intervencionista
Hospital Universitario Marqués de Valdecilla.
Avda. Valdecilla, s/n. 39008 Santander. Cantabria. España.
E-mail: hemodinamica@humv.es