Keywords
INTRODUCTION
Fractional flow reserve (FFR) has been shown to be useful in determining the functional repercussion of angiographically moderate or dubious lesions1-5 and in deciding whether to proceed with revascularization or not in patients with stable ischemic heart disease.6-10 An FFR measuring >0.75 or 0.8 in a specific lesion means revascularization can safely be postponed in the knowledge that long-term adverse events are unlikely to occur, while symptoms can be monitored as they would be in patients who do undergo treatment.6,8 Currently, most routine cardiac catheterizations are indicated for acute coronary syndrome (ACS). In these patients, the percentage of coronary angiographies that find no significant lesions, or show stenosis that is angiographically moderate or difficult to quantify, varies. In these cases, the prognostic value of pressure-wire measured FFR has either been little studied or proven controversial.3,11 The dynamic nature of lesions in ACS—presence of disturbed vasomotor tone, thrombus, areas of stunned myocardium or distal embolizations—can make decisions based on FFR questionable.3,11
In the present study, we analyze prognosis at 1 year in a series of patients with ACS and nonrevascularized angiographically moderate lesions based on FFR measured via intracoronary pressure wire.
METHODS
This is a descriptive observational study of a consecutive cohort of patients. We analyzed all procedures in our center between January 1, 2006 and June 30, 2008, that involved pressure-wire study of an angiographically moderate lesion (50%-70% visual stenosis). From these procedures, we selected patients hospitalized for ACS. We only included those whose medical record included a diagnosis of ACS made by a cardiologist (according to the definition current at the time)12 and then, only if the coronary angiography had been requested because of the indication of ACS. We conducted a follow-up of those patients who did not undergo revascularization of a lesion because of the FFR measurement.
We excluded coronary angiography studies indicated for chest pain of uncertain origin or in patients with valvular heart disease or cardiomyopathy which might have caused their clinical condition. We also excluded patients who underwent catheterization of a causal lesion and in whom the pressure wire was used to study lesions other than those being treated. A pressure-wire functional study of the lesion was performed at the criteria of the interventional cardiologist. Standard practice in our center is to not perform a pressure-wire study if—despite the fact we are dealing with an angiographically moderate lesion—the presence of thrombus is clear, the lesion causes <3 TIMI distal flow, or an image compatible with spontaneous dissection or ulcerated plaque can be seen.
Coronary Angiography, Invasive Study, and Treatment
Following our standard protocol, before the procedure all patients received aspirin (100 mg/ day or 300 mg loading dose if not previously administered) and clopidogrel (75 mg/day or 600 mg loading dose if not previously administered). Unless contraindicated, patients admitted for ACS received dual oral antiplatelet therapy for 1 year after discharge. On deciding to perform a pressure-wire study, we administered 5000 U intravenous sodium heparin if this had not been administered previously. Once the decision to perform a functional study of an angiographically moderate lesion had been taken, the diagnostic catheter was replaced by a 6 Fr guide catheter. With this, we repeated the projections, obtaining the best possible view of the lesion, with greater visual stenosis, and without superimposed branches or loss of length due to curvature. Functional measurement was with a 0.014" intracoronary pressure wire (Pressure Wire, Radi Medical Systems, Uppsala, Sweden). The guidewire was calibrated externally and then advanced to the distal end of the guide catheter. We verified the balance between the pressure curves in the catheter and the pressure wire. After administering 200-300 µg intracoronary nitroglycerin, the guide was advanced until the sensor was ≥10 mm distal from the lesion being studied. We measured FFR by administering 300-500 µg intracoronary adenosine. We took special care to avoid wedging the catheter in the coronary ostium after bolus injection of the drug. We measured FFR through the coefficient, beat by beat, between mean aortic pressure (aP) (at the tip of the guide catheter) and mean distal pressure (dP) on the lesion (recorded with the pressure wire), in maximum hyperemia. We measured FFR at least 3 times. Decision-making was based on the lowest FFR measurement. We only attempted a maximum 500 µg dose of intracoronary adenosine if a lower amount failed to produce a period of ≥6 s asystole. Patients with lesions of FFR ≥0.75 did not undergo coronary revascularization.
Medical treatment regimens before and after the procedure were always at the criteria of the physician responsible.
Variables
Patient baseline characteristics and procedure results were gathered from hospital medical records and catheterization laboratory registries of procedures in the hospital where the study took place or the center where the angiographic recording of the procedure was viewed. We considered enzyme elevation compatible with myocardial necrosis had occurred when, prior to coronary angiography, troponin I or T, or MB fraction creatine kinase (CK-MB) data were greater than figures considered normal in the laboratory where extraction took place.
Quantitative Analysis
Quantitative analysis was performed offline by an experienced interventional cardiologist blinded to the functional study results. Measurements were with MEDIS QAngio XA v 7.1 software (Medis Medical Imaging Systems, Leiden, The Netherlands).
Follow-up
Follow-up was conducted 1 year after the functional study by telephone and by consulting the medical records of patients who had required readmission. In patients undergoing repeat coronary angiography, we viewed the recording again to determine the state of the lesion previously studied. During follow-up, our primary outcome variables were cardiac- or unknown-cause death, non-fatal acute myocardial infarction, need for revascularization of the lesion studied, and the combination of all 3 events. We also recorded non-cardiac mortality, need for readmission due to ischemic heart disease, and need for revascularization of a lesion other than the one studied.
We considered myocardial infarction during follow-up to be hospitalization with a medical record giving that diagnosis upon discharge.
Statistical Analysis
Quantitative variables are expressed as mean (SD) and categorical variables as absolute values and percentage. For comparisons, we used Student t test for quantitative variables if the Kolmogorov-Smirnov test proved the distribution was normal. For non-normal distributions, we used the non-parametric Mann-Whitney U test. We performed linear regression analysis of the percentage of stenosis by diameter figures generated by offline digital quantification for each lesion studied and the FFR measurement determined by intracoronary pressure wire. We constructed the corresponding Kaplan-Meier survival analysis curves for each event analyzed in the 1-year follow-up. Statistical analysis was done with SPSS 15.0 for Windows.
RESULT S
Between January 1, 2006 and June 30, 2008, 111 patients fulfilled our inclusion criteria. A priori, we excluded 5 patients who were visitors to Spain and would not, therefore, be available for 1-year follow-up. The final sample consisted of 106 patients. During the study period, another 37 moderate lesions were treated because they presented an FFR <0.75 and were suspected of causing the ACS episode in 33 patients. The 144 patients undergoing pressure-wire studies in moderate lesions that possibly caused the clinical signs and symptoms of ACS were 7.8% of the total 1843 patients undergoing cardiac catheterization in our center and diagnosed with ACS in this period.
Baseline patient characteristics are in Table 1. Twenty-one percent of patients presented myocardial necrosis marker elevation and 28% presented dynamic ST-segment changes during episodes of pain (13% ST-segment elevation; 15% ST-segment depression) when these were observed. Some 12% of patients with non-ST segment elevation acute coronary syndrome (NSTEACS) were discharged with a diagnosis of non-ST segment elevation acute myocardial infarction (NSTEAMI). Of these, 80.4% were diagnosed with unstable angina and the rest with chest pain without significant lesions. Over 95% of patients received antiplatelet drugs before coronary angiography and 73% received dual oral antiplatelet therapy with aspirin and clopidogrel. Other treatment regimens are in Table 2.
We studied 127 lesions in the 106 patients enrolled. In 14 patients, we studied 2 lesions (13%); in 2 patients, 3 lesions (1.9%); and in 1 patient, 4 lesions (0.9%). In most patients, 89 (86%), we studied a single lesion. Of the 127 lesions studied, 8 were restenosis in the stent (6%) and the rest, de novo lesions.
During procedures, we observed no complications other than frequent episodes of atrioventricular block and one case of paroxystic atrial fibrillation after the adenosine-induced pause, which reverted spontaneously at 3 hours. All episodes of bradycardia ended spontaneously.
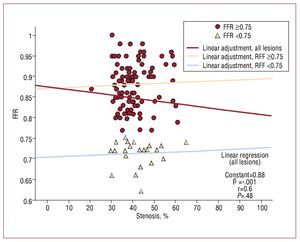
The results of computerized quantification of the lesions are in Table 3. We found statistically significant differences in reference diameter and minimum lumen diameter of lesions with FFR greater and less than 0.75, although their size was not relevant. We found a clear superimposition of the percentage of stenosis between lesions that were functionally significant and those that were not (Figure 1). Ten lesions (7.9%) had an FFR between 0.75 and 0.8. Linear regression analysis found no correlation (r=0.06) between FFR measurements and computerized quantification of lesions (Figure 1).
Figure 1. Correlation between angiographic stenosis (by diameter) obtained using offline digital quantification and fractional flow reserve measurement. FFR indicates fractional flow reserve.
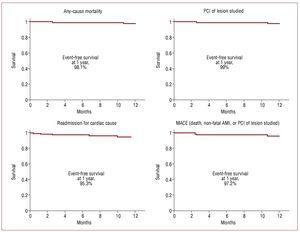
In the follow-up, we found no in-hospital complications. We achieved complete follow-up at 1 year in 103 patients (97.2%). Two men, aged 78 and 73 years, died during follow-up (FFR 0.85 and 0.96, respectively). Both had severe ventricular dysfunction at the time of the functional study. The first died in-hospital following admission for heart failure at 78 days after coronary angiography (without presenting new associated symptoms of angina or cardiac marker elevation); the second died in his sleep, at home, 325 days after coronary angiography. One patient (FFR=0.92) was readmitted at 70 days following coronary angiography for a new episode of angina at rest and underwent percutaneous coronary intervention (PCI) of the lesion previously studied on finding clear angiographic progression of the stenosis. We recorded no episode of acute myocardial infarction during 1-year follow-up. Similarly, 97.2% of patients remained free of the combined outcome. Survival curves are in Figure 2.
Figure 2. Kaplan-Meier survival curves for the different events analyzed. PCI indicates percutaneous coronary intervention; MACE, major adverse cardiovascular event.
Twelve patients (11.3%) were readmitted during the first year of follow-up. Only 5 readmissions were for cardiac causes (4.7%). Repeat coronary angiography revealed no significant lesions in 2 patients: one underwent the PCI described above; in the other, we found angiographic improvement of the lesion studied.
DISCUSSION
The present study shows the good prognosis of a consecutive series of >100 patients admitted for ACS with angiographically moderate lesions that were the only possible cause of their clinical signs and symptoms but who did not undergo revascularization because of their FFR measurement obtained by pressure-wire study. To date, this is the largest reported consecutive series in which FFR has been used to decide on the revascularization of the only lesions that could possibly have caused ACS. An earlier study13 of 124 patients with ACS also used FFR to decide on the revascularization of angiographically moderate lesions. However, in contrast to the present study, 28% of patients received treatment for other significant lesions, which were probably the cause of their clinical condition, in the same procedure.
Fractional flow reserve determined with intracoronary pressure wire has proved useful in measuring angiographically moderate lesions1-10 and, recently, in deciding on the revascularization of angiographically significant lesions.14 Most studies were conducted in patients with stable ischemic heart disease but the value of pressure-wire studies in the evaluation of lesions in ACS has been questioned.3,11,15,16
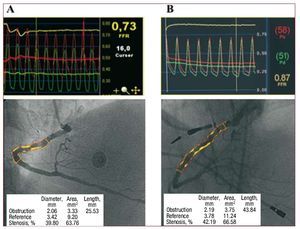
In daily clinical practice, ACS is the most frequent indication for coronary angiography. Early invasive management of ACS and the availability of coronary angiography mean many such interventions are conducted without a prior test for ischemia. Up to 6%-10% of coronary angiographies indicated for ACS reveal moderate lesions or the absence of significant lesions.17 To this, we should add the indeterminate number of patients in whom we find chronic lesions or diffuse disease unrelated to ACS and lesions of dubious functional significance elsewhere in the coronary tree. In our experience, angiography was insufficient to determine the functional repercussion of lesions analyzed (Figure 3).
Figure 3. Example of 2 patients with acute coronary syndrome. Both present lesions in right descending coronary artery. A: long stenosis in right descending coronary artery quantified in 39.8% and significant FFR (0.73). B: stenosis in right descending coronary artery quantified in 42.2% and non-significant FFR (0.87).
The decision to revascularize moderately significant lesions can be taken in the catheterization laboratory itself on the basis of the clinical and angiographic data available. Alternatively, this decision can be taken on the basis of an invasive functional test during the procedure, or of noninvasive tests. Decision-making, together with a possible revascularization, can then be postponed until a second intervention. In this context, in a small study18 FFR measured with pressure wire at the time of the coronary angiography showed cost-reduction benefits with the same incidence of long-term clinical events as did isotopic gammagraphy in patients with dubious lesions and ACS.
Although there is insufficient scientific evidence to support it, the intracoronary pressure wire is used on a daily basis to determine the functional significance of lesions in ACS.7,10,13,14,19 Doubts about the validity of the pressure wire in ACS are justified, on the one hand, by the transitory changes in microcirculation in the first hours of ACS (presence of thrombus, microvascular ischemic dysfunction, myocardial contusion)20 that can temporarily limit the vasodilatory response to the drug administered and give rise to an overestimation of FFR because maximum hyperemia is not achieved. On the other hand, the dynamic nature of the lesions means the pressure wire cannot predict the progress of the stenosis studied.
In our series, we found no adverse events directly attributable to the lesions studied and not revascularized, except in one patient who needed revascularization during follow-up. In line with current guidelines on ACS, the standard practice of anticoagulation and antiplatelet therapy at admission and dual antiplatelet therapy after discharge, together with statin treatment,12 doubtless favors the stabilization of lesions in which, due to our selection criteria, stenosis is not important, flow is normal, and angiographic evidence of instability does not exist.
In our study, only 1 (0.8%) of 127 lesions studied required revascularization during follow-up because stenosis had progressed since functional evaluation. A similar case was reported earlier.11 The patient evolved as would be expected for a new readmission for angina at rest without infarction or any other major event. In 99.2% of the remaining lesions, although coronary angiography was not performed during follow-up, the patients' favorable clinical evolution suggests the stability of the lesions studied.
Diagnosis of ACS is fundamentally clinical. In our series, following the inclusion criteria, all patients had been diagnosed with ACS by a cardiologist and coronary angiography was requested for this indication. Given the coronary angiography findings, we cannot ignore the fact that the clinical condition of some patients included may have been of noncoronary origin. Far from diminishing the value of pressure-wire studies in these patients, we believe this enhances it because we avoid revascularizations that might be considered even less necessary.
Based on these results, we are unable—nor is it our intention—to consider FFR measured with an intracoronary pressure wire as the parameter that, on its own, would enable us to decide about the revascularization of angiographically moderate lesions in ACS. In our study, we excluded lesions presenting clear angiographic signs of instability. The value of the intracoronary pressure wire in the presence of visible thrombus, ulcerations, dissections or coronary flow deterioration has not been studied, and should not be used as a decision-making tool in these clinical situations. The results of this study lead us to believe that FFR measured with the intracoronary pressure wire is a useful tool that, added to angiography and clinical data, safely enables us safely to not revascularize patients admitted with a diagnosis of ACS and moderate coronary lesions, even when doubt exists about a possible relationship with the clinical signs and symptoms motivating hospitalization.
Limitations
Over 80% of patients had normal troponin levels, indicating we are dealing with an ACS population at low risk and/or with chest pain of uncertain origin. However, this does not undermine the validity of the study, which aims to evaluate FFR as a means of responding to clinical doubt arising in a real context, in patients hospitalized for chest pain, arriving at the catheterization laboratory and presenting the interventional cardiologist with a dubious lesion.
As we have discussed, the conclusions of this study are only applicable to lesions with the characteristics specified. We cannot possibly confirm the validity of FFR in decision-making in cases of visible thrombus, dissection or ulceration, or <3 TIMI flow.
In all cases, FFR measurement was with intracoronary adenosine. Several studies have shown this approach achieves a lower level of hyperemia than intravenous adenosine.21-24 To date, all published studies have used <250 µg intracoronary adenosine.21-25 In fact, one comparative study found no significant differences between intravenous and intracoronary administration of 150 µg adenosine.26 One recent study has found that intracoronary administration of high doses of adenosine in perfusion can be better than intravenous administration to ensure maximum hyperemia.27 Our research group routinely uses >300 µg intracoronary adenosine, carefully administered and with equally careful FFR calculation, with no evidence of adverse effects. We believe that significant overestimation of FFR figures is unlikely. However, given the objective of our study (to test the safety of non-revascularization of specific lesions on the basis of FFR measurements), small overestimations of FFR would not modify the conclusions.
We cannot disregard the fact that in some patients included in the study, the causal lesion might differ from that studied and might not cause even moderate stenosis. Nor can we discount the possibility, as mentioned in the discussion, of a noncardiac cause for the signs and symptoms of some patients. However, these issues do not detract from the validity of the study. Even in this minority of patients, the study would answer the question as to whether or not it is valid to use FFR in moderate lesions considered the potential cause (whether correct or not) in patients diagnosed (correctly or not) with ASC to avoid unnecessary revascularization procedures.
CONCLUSIONS
In ACS, as in stable ischemic heart disease, FFR measured by intracoronary pressure wire can be a useful tool to avoid the unnecessary revascularization of angiographically moderate coronary lesions when and if they have been carefully selected to exclude those cases with angiographic signs of instability.
ABBREVIATIONS
ACS: acute coronary syndrome
FFR: fractional flow reserve .
Correspondence: Dr. R. López Palop.
Vía Láctea, 38. Urbanización la Glorieta. 30110 Churra. Murcia. España.
E-mail: mlopezs@meditex.es
Received August 25, 2009.
Accepted for publication January 20, 2010.