The 2024 Interamerican Society of Cardiology (SIAC) guidelines on cardiorespiratory rehabilitation (CRR) in pediatric patients with congenital heart disease aim to gather and evaluate all relevant evidence available on the topic to unify criteria and promote the implementation of CRR programs in this population in Latin America and other parts of the world. Currently, there is no unified CRR model for the pediatric population. Consequently, our goal was to create these CRR guidelines adapted to the characteristics of congenital heart disease and the physiology of this population, as well as to the realities of Latin America. These guidelines are designed to serve as a support for health care workers involved in the care of this patient group who wish to implement a CRR program in their workplace. The guidelines include an easily reproducible program model that can be implemented in any center. The members of this Task Force were selected by the SIAC on behalf of health care workers dedicated to the care of pediatric patients with congenital heart disease. To draft the document, the selected experts performed a thorough review of the published evidence.
Keywords
Our guidelines for cardiorespiratory rehabilitation (CRR) in pediatric patients with congenital heart disease (CHD) are intended as a roadmap for implementing a rehabilitation program tailored to the unique characteristics of this population. These include ongoing physiological development and growth, and the evolving nature of their condition, setting them apart from adults. To this end, the Inter-American Society of Cardiology (SIAC) established the Task Force on Cardiopulmonary Rehabilitation in Pediatric Patients with Congenital Heart Disease within the Chapter on Cardiovascular Prevention in Children and Adolescents of the Pediatric Cardiology Council and Congenital Heart Disease in Adults of the SIAC. This working group includes representatives of various scientific and academic societies across the continent, as well as experts in several subspecialties, indicated in appendix 1.
We have taken into account the sociodemographic characteristics of Latin America to ensure that the program can be implemented in multiple health care and home care settings, regardless of the available infrastructure.
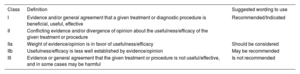
The level of evidence and strength of the recommendation for each therapeutic option were assessed according to predefined scales (table 1 and 2).
Classes of recommendations
| Class | Definition | Suggested wording to use |
|---|---|---|
| I | Evidence and/or general agreement that a given treatment or diagnostic procedure is beneficial, useful, effective | Recommended/Indicated |
| II | Conflicting evidence and/or divergence of opinion about the usefulness/efficacy of the given treatment or procedure | |
| IIa | Weight of evidence/opinion is in favor of usefulness/efficacy | Should be considered |
| IIb | Usefulness/efficacy is less well established by evidence/opinion | May be recommended |
| III | Evidence or general agreement that the given treatment or procedure is not useful/effective, and in some cases may be harmful | Is not recommended |
Levels of evidence
| Level | Evidence |
|---|---|
| Level of evidence A | Data derived from multiple randomized clinical trials or meta-analyses |
| Level of evidence B | Data derived from a single randomized clinical trial or large randomized studies |
| Level of evidence C | Consensus of opinion of experts and/or small studies, retrospective studies, registries |
CHD has a prevalence of 1% among live births. Approximately 70% of patients with this condition will require surgical interventions or cardiac catheterizations, while only 30% will need follow-up and medical treatment.1 Physical activity during childhood is crucial for proper social, intellectual, and physical development, as well as for preventing noncommunicable chronic diseases, such as obesity, hypertension, hypercholesterolemia, insulin resistance, metabolic syndrome, and cardiovascular conditions.2
According to current recommendations of the World Health Organization, the pediatric population should engage in moderate to vigorous physical activity for 60minutes per day, every day, and strength exercises 3 times per week to achieve significant metabolic changes.3
Most children with CHD show decreased functional capacity (FC) and are at a higher risk of mid-term morbidity and mortality.4 This can be attributed to both central causes (reduced cardiac output due to myocardial dysfunction or chronotropic incompetence) and peripheral causes (skeletal muscle impairment,5 inadequate tissue perfusion,6 intrinsic metabolic defects causing inefficient energy use, early anaerobic metabolism leading to rapid lactate accumulation, and a higher proportion of type IIb muscle fibers).7
Moreover, pulmonary function and perfusion are disrupted, with a restrictive ventilatory pattern resulting from phrenic nerve injury, diaphragmatic plications, thoracosternotomies, and chest deformities. Respiratory muscle weakness, pulmonary hypoplasia due to compression, and intrapulmonary shunts also contribute to reduced FC and an exaggerated increase in ventilation rate per minute during physical exertion. This occurs independently of elevated carbon dioxide levels due to changes in the ventilation-perfusion ratio.8
Physical exercise and cardiorespiratory rehabilitation programs (CRRP) are useful for improving: a) the patient's FC; b) peak oxygen consumption (VO2); c) left ventricular ejection fraction; d) peripheral muscle pump efficiency; e) ventilatory pump efficiency; f) morbidity associated with complex CHD9; g) oxygen saturation (SaO2); h) self-esteem and functional independence; and i) overall quality of life (QoL). These benefits are achieved with no reported adverse effects10 and the improvements are significant and sustained (6-9 months).11
CRRP should include aerobic and muscle strength exercises to enhance the patient's physical capacities and metabolic systems. For prepubescent children, the approach should be entertaining, involving games and challenges, to be effective and sustainable. Unlike adults, this population experiences less muscle fatigue due to greater use of the oxidative system and a higher proportion of slow-twitch muscle fibers (type I), with lower lactate accumulation, acidosis, and oxygen debt, and faster recovery following high-intensity exercise.12 In addition, muscle strength exercises increase physical power and bone density, reduce the risk of injuries, and improve motor skills, sports performance, body composition, insulin sensitivity, the lipid profile, and cardiovascular function.13
OBJECTIVESThe primary objective of this study was to design a muscular and metabolic CRRP for children and adolescents with CHD, taking into account the circumstances of our continent. Secondary goals include improving the FC, QoL, and self-esteem of these patients, while also reducing cardiovascular risk factors, morbidity, and mortality.
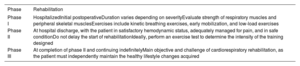
CARDIORESPIRATORY AND MUSCLE REHABILITATION PROGRAMSA multidisciplinary team is essential, comprising a pediatric cardiologist, pediatrician, dietitian, pediatric nutritionist, nurse, kinesiologist, physiotherapist, social worker, and psychologist. All members should have a thorough understanding of exercise physiology, CHDs, management and alleviation of these conditions, and pre- and postintervention pathophysiology, and be adept at recognizing signs and symptoms of alarm (recommendation class IIa, level of evidence C). All rehabilitation programs involve 3 phases (recommendation class IIa, level of evidence C) (table 3).14
Rehabilitation phase
| Phase | Rehabilitation |
|---|---|
| Phase I | HospitalizedInitial postoperativeDuration varies depending on severityEvaluate strength of respiratory muscles and peripheral skeletal musclesExercises include kinetic breathing exercises, early mobilization, and low-load exercises |
| Phase II | At hospital discharge, with the patient in satisfactory hemodynamic status, adequately managed for pain, and in safe conditionDo not delay the start of rehabilitationIdeally, perform an exercise test to determine the intensity of the training designed |
| Phase III | At completion of phase II and continuing indefinitelyMain objective and challenge of cardiorespiratory rehabilitation, as the patient must independently maintain the healthy lifestyle changes acquired |
The target population includes individuals meeting the specified inclusion and exclusion criteria, evaluated by the rehabilitation team to initiate CRR (recommendation class IIa, level of evidence C) (table 4).
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Age between 6 and 21 years, with CHD, awaiting a heart transplant, or following heart transplantation | Unable to follow or maintain simple instructions to carry out assessment or CRR |
| HR decreased | Lack of motivation on the part of the patient or guardians |
| Stable clinical condition, with steady heart rhythm and hemodynamics, and no signs of decompensation or acute exacerbation | Acute inflammatory or infectious condition |
| Attending physician approves initiation of CRR | |
| Guardians provide informed consent and patient agrees to start and continue in the CRR program | Withdrawal of informed consent |
CHD, congenital heart disease; CRR, cardiorespiratory rehabilitation; FC, functional capacity.
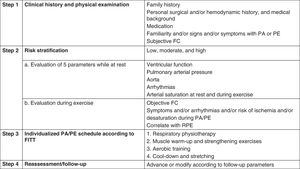
CRRPs involve 3 essential steps: conducting a comprehensive initial assessment to stratify risk, setting safety limits to minimize adverse effects, and determining the positive impact of the program upon completion (recommendation class IIa, level of evidence C) (figure 1).
Central illustration. Steps for proper cardiorespiratory rehabilitation. Modified from Budts et al.15 with permission. FC, functional capacity; FITT, frequency, intensity, time, and type; PA, physical activity; PE, physical exercise; RPE, rating of perceived exertion.
Comprehensive medical history: underlying heart disease, surgical interventions and catheterizations, noncardiac comorbidities, medication, and signs and symptoms triggered by physical exercise (table 5).
Main features of individualized exercise prescription
| Physical examination | Laboratory biometric evaluation* |
| Exercise testing | Functional capacity assessment |
| Musculoskeletal evaluation | StrengthBalanceFlexibilityCoordination |
| Quality of life assessment | Questionnaires (PedsQL, ConQol) |
| Recommendations for healthy lifestyle | Patient- and family-centeredRegarding physical activity and self-efficacy questionnaires |
The important tests for risk stratification include the following (recommendation class IIa, level of evidence C):
- •
Resting ECG and 24-hour Holter monitoring for arrhythmias.
- •
Transthoracic echocardiography study.
- •
6-minute walk test. This is a simple, accessible, low-cost, submaximal evaluation that is well tolerated and does not require complex equipment: measuring tape, 2 cones, a 30-meter track, a heart rate (HR) monitor, SaO2, and a standardized protocol. It is preferably administered in children less than 8 years of age, along with a subjective effort scale (RPE, rating of perceived exertion) for the initial assessment and subsequent monitoring.
- •
Conventional exercise testing or cardiopulmonary exercise testing (CPET) with analysis of gases. These tests are used to evaluate the cardiovascular response to physical activity in CHD patients. Conventional exercise tests monitor blood pressure, HR, and SaO2 during exertion and can detect arrhythmias and other ECG abnormalities. CPET, however, is the reference technique, delivering data on peak and maximum VO2, respiratory efficiency, respiratory reserve, anaerobic threshold, oxygen pulse, and ventilation-perfusion ratio, among numerous other parameters. The drawbacks of this test include its high cost and limited availability. CPET is not recommended for prescribing exercise regimens in children younger than 8 years due to inadequate quality (recommendation class IIa, level of evidence C).15
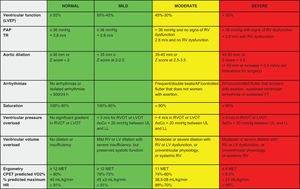
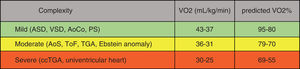
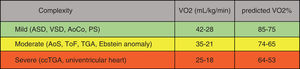
Risk stratification should be carried out (figure 2). Patients are assigned to 1 of the 3 training intensity levels described by Budts et al.,15 and subsequently incorporated into the CRRP (recommendation class IIa, level of evidence C) (figure 3 and figure 4).
Cardiovascular factors to assess for risk stratification. AoCo, aortic coarctation; AF, atrial fibrillation; CPET, cardiopulmonary exercise testing; HR, heart rate; LL, lower limbs; LV, left ventricle; LVEF, left ventricular ejection fraction; LVOT, left ventricular outflow tract; MET, metabolic equivalent of task; PAP, pulmonary arterial pressure; RV, right ventricle; RVOT, right ventricular outflow tract; TR, tricuspid regurgitation; UL, upper limbs; VT, ventricular tachycardia; VO2, oxygen consumption.
Expected aerobic capacity in children and adolescents with CHD up to 16 years old. Compiled using data from Amedro et al.16 and Ten Harkel et al.17 ASD, atrial septal defect; AoCo, aortic coarctation; AoS, aortic stenosis; ccTGA, congenitally corrected transposition of great arteries; PS, pulmonary stenosis; TGA, transposition of great arteries; ToF, tetralogy of Fallot; VO2, oxygen consumption; VSD, ventricular septal defect.
Expected aerobic capacity in children with CHD older than 17 years and adults. Compiled using data from Abella et al.,18 Rhodes et al.,19 and Kempny et al.20 AoCo, aortic coarctation; AoS, aortic stenosis; ASD, atrial septal defect; ccTGA, congenitally corrected transposition of great arteries; PS, pulmonary stenosis; TGA, transposition of great arteries; ToF, tetralogy of Fallot; VO2, oxygen consumption; VSD, ventricular septal defect.
Use of the FORCE21 tool is recommended, an acronym for the following analysis: F, ventricular function; O, O2 saturation; R, heart rhythm; C, complexity of the coronary anatomy, E, elevated pressure or elevated ventricular volume.
Currently, hybrid programs are being implemented: initially, patients and guardians undergo training and education in the hospital, and thereafter, they continue activities at home. This approach fosters acceptance, adherence, and favorable results.22 Patients with values in red must undergo fully monitored hospital-based CRR due to the associated risk, while those at low to moderate risk may transition to home-based CRR, as further explained below (recommendation class IIa, level of evidence C).
Step 3At the start, a meeting will be held with the patient and guardians to explain the assessment and training schedule. A local informed consent form detailing potential adverse effects during CRR is then signed. A record of the planned activities should be maintained for monitoring and adjustment purposes.
Programming physical activityUse of the FITT acronym (frequency, intensity, time, and type of exercise) is recommended for designing the exercise regimen (recommendation class IIa, level of evidence C) (table 6).23
Exercise prescription for aerobic and resistance training
| Prescription | Aerobic | Resistance |
|---|---|---|
| Frequency (per week) | 5-7 d | 3 d |
| Intensity (load) | Moderate | Light to moderate |
| Time (min) | 60 | 30 |
| Type of exercise | JoggingJump ropeScissor jumpsJump squatsCyclingSwimming | Body weight: push-ups. Squats.Static and dynamic plank |
FITT, frequency, intensity, time, and type.
The sessions will include groups of 2 to 6 children, 2 to 3 times per week for 12 weeks, with each session lasting 45 to 60minutes, all under the supervision of a professional. Groups will be organized based on pubertal development and familiarity with the exercises performed, rather than age, sex, or body size (recommendation class IIa, level of evidence C).
A kinesiologist, physical education specialist, or sports medicine physician will conduct the functional assessment of strength, flexibility, and coordination. All exercises should be supervised to ensure proper technique and prevent injuries (recommendation class IIa, level of evidence C).
Each CRR session consists of 4 stages: a) respiratory physiotherapy; b) muscle warm-up and strengthening exercises; c) aerobic training; and d) cooling down and stretching (table 7).
Training prescription for a cardiorespiratory rehabilitation session
| Stages | Training prescription |
|---|---|
| Respiratory physiotherapy (10 min; 5 times/wk) | At least 2 sets of 30 repetitions/d, at least 5 times/wkAt 30%-60% of the MIP obtainedAlways use a nasal clipMaintain a respiratory rate of 12 to 16 breaths per minute (avoid hyperventilation) and with a diaphragmatic breathing pattern |
| Muscle warm-up and strengthening exercises(20 min; 3/wk) | Initial exercises with body weight:Squats, lunges, jumps to work lower limbsArm push-ups on wall or floor, triceps push-ups to work upper limbsStatic, dynamic, and side planks or Swiss ball planks to work the coreAdjust load using the RPE or 1-RM test. Start with low intensity and gradually increase to the recommended levelIncrease the number of sets according to capacity (3 sets of 8 to 12 repetitions)Resting for more than 60 s between sets allows BP and HR to return to resting valuesAvoid performing Valsalva maneuvers during exertion to prevent a CO decrease and syncope |
| Aerobic training (20min 3 times/wk) | Start training at low intensity and progress to moderate and vigorous according to tolerance, usually within 8 to 10 wksafter starting trainingMICT (± 30 min): 5min warm-up, 20min at the target HR, and 5min cool-downHIIT (± 20 min): 5min warm-up, 15min of high intensity (alternating 1min at high intensity with 1min of low-intensity rest), and 5min cool-down |
| Cool-down and stretching (5-10 min) | Low intensity exercises that enable gradual recovery of BP and HR |
HR, heart rate; CO, cardiac output; HIIT, high-intensity interval training, MICT, moderate-intensity continuous training; BP, blood pressure; MIP, maximum inspiratory pressure; 1-RM, 1-repetition maximum; RPE, rating of perceived exertion.
Inspiratory muscle strength should be assessed24 by measuring the maximum inspiratory pressure25 or maximum nasal inspiratory pressure (SNIP, sniff nasal inspiratory pressure)26 (recommendation class IIa, level of evidence C) (table 8). There is a good correlation between these 2 parameters, but the correlation decreases in the presence of airway obstruction.26
Methods for assessing inspiratory muscle strength
| Pressure | Measurement of inspiratory muscle strength |
|---|---|
| Maximum inspiratory pressure (MIP) | From age 6 y, while seated and using a nasal clip, following a maximal expirationPerform at least 3 measurements with <10% difference between themAccept the highest value obtained |
| Maximum nasal inspiratory pressure (SNIP, sniff nasal inspiratory pressure) | Measure inspiratory pressure in one nostril during a deep, rapid inhalation.Perform 10 short, quick sniff maneuvers, with the mouth closed, following quiet breaths at residual functional capacity, with a 30-sec interval between each maneuverAccept the maximum value obtained |
The inspiratory muscles should be trained using inspiratory valves, such as the Threshold IMT (Philips Respironics, United States) or POWERbreathe (POWERbreathe Intl Ltd, United Kingdom). To work on muscle strength, pressures should be increased with fewer repetitions per session. These exercises improve maximum inspiratory pressure, vital capacity and total lung capacity, fatigue resistance, and peak VO2 in heart failure patients.27 In addition, they enhance diaphragm thickness,28 promote greater systemic venous return during inspiration,29 and improve ventilatory pump function (recommendation class IIa, level of evidence C).30 Furthermore, when combined with abdominal or abdominal plus diaphragmatic breathing, they help to reduce dyspnea and enhance HR on exertion, and improve QoL.31
Muscle warm-up and strengthening exercisesIt is important to train the major muscle groups, such as the deltoids, biceps, triceps, core muscles, quadriceps, hamstrings, and calf muscles. These exercises improve and enhance the peripheral muscle pump, leading to increased heart rate due to greater venous return and cardiac output, both at rest and during exercise (recommendation class IIa, level of evidence C).
Training for prepubescent patients focuses on promoting greater agility, balance, coordination, flexibility, and strength (recommendation class IIa, level of evidence C).15,25
Aerobic trainingAerobic training can be done on a treadmill, stationary bicycle, rowing machine, or arm bicycle. Moderate-intensity continuous training (MICT) and high-intensity interval training (HIIT) are both effective for improving FC.32 MICT is preferable for older patients with pulmonary or cardiac limitations, as it is better tolerated, although it demands more time. HIIT is more appealing to prepubescent patients and induces greater metabolic stress compared with MICT. It also requires better cardiorespiratory adaptation, because peak effort is rapidly reached. Patients with CHD can undertake HIIT, but only after a period of low- to moderate-intensity training to gradually build tolerance.33 Risk stratification is particularly important for these high-intensity activities. In postpubescent individuals, programs can be structured similarly to those for adults, focusing on aerobic and muscle strength training (recommendation class IIa, level of evidence C).
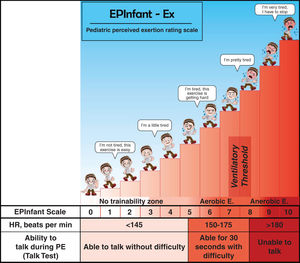
Exercise intensity can be adjusted through: a) HR reserve; b) maximum HR, determined by conventional exercise testing or estimated using Tanaka's (208 – [0.7 × age]) or Karvonen's (220 – age) formula; c) maximum or peak VO2; d) subjective effort scale; and e) 1-repetition maximum test (recommendation class IIa, level of evidence C) (table 9).
Exercise intensity based on various prescription methods
| Intensity | Aerobic training target (%) | Subjective aerobic training | Ventilatory thresholds for CPET | Resistance training (%) |
|---|---|---|---|---|
| Low (mild) | 20–39 RHR40–54 HRmax20–39 VO2max/peak | RPE: 2–3 | 30–49 1-RM | |
| Moderate | 40–59 RHR55–69 HRmax 40–59 VO2max/peak | RPE: 4–5 | Below VT1 | 50–69 1-RM |
| Vigorous | 60–84 RHR70–89 HRmax60–84 VO2max/peak | RPE: 6–7 | Between VT1 and VT2 | 70–79 1-RM |
| High (intense) | ≥85 RHR≥90 HRmax≥85 VO2max/peak | RPE:≥8 | Above VT2 | ≥80 1-RM |
1-RM, 1-repetition maximum; HRmax, maximum heart rate; CPET, cardiopulmonary exercise test; RHR, resting heart rate; RPE, rating of perceived exertion – EPInfant-Ex (1-10); VO2max/peak, maximum or peak oxygen consumption; VT1, ventilatory threshold 1; VT2, ventilatory threshold 2.
Table compiled using data from Tran et al.33
The subjective effort scale, SaO2, blood pressure, and HR should be monitored before, during, and after exercise, while always being attentive to signs and symptoms of alarm (recommendation class IIa, level of evidence C).
Cooling down and stretchingThese are low-intensity exercises that should last from 5 to 10minutes. Omitting the cooling down stage could result in a temporary decrease in venous return and coronary flow when HR and myocardial oxygen consumption are still high, leading to hypotension, angina, ST-segment changes, and ventricular arrhythmias.34
Step 4Periodically (weekly or monthly) perform a reassessment of the type of training, the technique, and the workload, making adjustments based on any changes (recommendation class IIa, level of evidence C).
Upon completion of CRRP, follow-up is conducted to evaluate whether the benefits achieved are sustained. It is recommended to monitor patients at 3, 6, and 12 months following completion (recommendation class IIa, level of evidence C).
HOME-BASED REHABILITATION AND TELEREHABILITATIONRemote cardiorespiratory rehabilitation (RCRR) for CHD patients is feasible, safe and effective, providing similar benefits to those described (class IIb recommendation, level of evidence B).35 RCRR should be supervised in person by a family member and overseen by a remote professional.
The same 4 steps outlined in hospital-based CRR (figure 1) should be used. However, only individuals classified with low or moderate risk are able to undertake this approach. The initial individual assessment and prescription should be conducted in person to teach the proper exercise technique and instruct patients and guardians on signs and symptoms of alarm; thereafter, rehabilitation can be done remotely (recommendation class IIa, level of evidence C).36,37
For RCRR, it is advisable to provide a printed or digital manual containing recommendations, care instructions, and details of the activities, in order to determine compliance and adjustments (recommendation class IIa, level of evidence C).14 To boost adherence and compliance, weekly activity manuals and contact (via WhatsApp or e-mail) are recommended, as well as alternating synchronous and asynchronous sessions using video tutorials (class I recommendation, evidence level B).36 Weekly telephone contact increases adherence by addressing concerns, encouraging activities, and monitoring QoL36 (recommendation class IIa, level of evidence B). An in-person or virtual motivational interview is recommended for patients and their families to inform and educate on healthy lifestyle habits and HR improvements (class I recommendation, evidence level B).37 RCRR fosters adherence and self-care in an every day, family setting at no cost. It is particularly useful in primary care, where there may be limitations, such as work and school obligations and geographic constraints (recommendation class IIa, level of evidence C).
The number of weekly sessions and their duration, length of the program, and interval between assessments are similar to those described for CRR. The FITT acronym is maintained for aerobic and resistance exercises. The exercises can be conducted using a treadmill or stationary bicycle, and by engaging in recreational activities that use body weight or household items for added weight (class I recommendation, evidence level B).38
Role of the physiotherapistA physiotherapist should be present throughout all phases of the CRRP. Their involvement starts in the immediate postoperative period, focusing on weaning patients off mechanical ventilation, providing respiratory physiotherapy, initiating early mobilization, and introducing light exercise, based on the patient's clinical and hemodynamic status. The objective is to prevent respiratory and thromboembolic complications, reduce the duration of mechanical ventilation, intensive care stay and hospitalization, ensure patients are discharged in the best physical condition, and provide educational guidance for prompt CRR initiation (recommendation class IIa, level of evidence C).39
After the initial physical evaluation, the physiotherapist will indicate the training program and identify any neuromuscular deficits that could hinder achievement of goals or aerobic training (recommendation class IIa, level of evidence C).
Role of the nutritionist and healthy habitsIn children with CHD, the prevalence of overweight ranges from 9.5% to 31.5% and that of obesity from 9.5% to 26%.40 Therefore, it is essential to encourage a healthy diet to prevent poor nutrition due to excess, decrease blood pressure, improve peak VO2, lengthen endurance time,41 and avert early cardiovascular disease. Evaluation of nutritional status (table 10) should be continuous, personalized, and involve the family (recommendation class IIa, level of evidence C).
Evaluation of nutritional status
| Evaluation of nutritional status |
| AnthropometryWeight and height for age and sex, body mass index for age and sex, and waist circumference. Cutoff point for diagnosing malnutrition due to excess:BMI/age: overweight,>+1 and <+2 SD; obesity,>+2SDWaist circumference: central adiposity excess ≥ 90th percentile or waist/height ratio> 0.5 |
| Healthy eatingFood intake routines (food frequency questionnaire and 24-h dietary recall) |
| LaboratoryComplete blood count, biochemical and lipid profile, and glucose, insulin, TSH, free T4, and vitamin D levels |
SD, standard deviation; BMI, body mass index.
Active and passive exposure to tobacco and electronic cigarettes, as well as alcohol consumption, should be avoided (recommendation class IIa, level of evidence C).42
Role of the psychologistPsychological interventions alleviate distress and improve blood pressure and cholesterol levels.43 Effective communication with health care staff is a key component in CRRPs. An approach to mental health care that promotes patient and family acceptance and commitment is important to motivate healthy behavior patterns (recommendation class IIa, level of evidence C).10
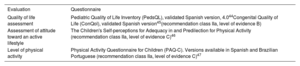
QoL questionnaires, such as PedsQL44 or ConQol,45 should be administered at the beginning and end of CRRP (recommendation class IIa, level of evidence B; table 11).
Recommendations for validated questionnaires
| Evaluation | Questionnaire |
|---|---|
| Quality of life assessment | Pediatric Quality of Life Inventory (PedsQL), validated Spanish version, 4.044Congenital Quality of Life (ConQol), validated Spanish version45(recommendation class IIa, level of evidence B) |
| Assessment of attitude toward an active lifestyle | The Children's Self-perceptions for Adequacy in and Predilection for Physical Activity (recommendation class IIa, level of evidence C)46 |
| Level of physical activity | Physical Activity Questionnaire for Children (PAQ-C). Versions available in Spanish and Brazilian Portuguese (recommendation class IIa, level of evidence C)47 |
The necessary equipment needed will depend on the type of patient, local infrastructure, and whether the approach is in-person or remote.
Professional teamThe optimal framework involves a multidisciplinary team. However, at the very least, a physician is required for risk assessment, together with a qualified professional for prescribing and conducting training.
Physical settingThe setting can be a closed, climate-controlled environment or an open space, such as a plaza or sports field.48 Closed environments should have an area of at least 24 m2, be well-ventilated and illuminated, with a ceiling height of >2.5 m, a temperature between 22°C and 25°C, and nonslip flooring (recommendation class IIa, level of evidence C).48
EquipmentIn a closed environment, the following should be available: a) a treadmill with front and side support, a safety lock, and adjustable speed and incline, or a cycle ergometer with cadence or speed readings and power in watts10,49; b) suspended ropes or bands, dumbbells, weights, or elastic bands with various resistance levels for muscle strengthening48; and c) additional material, such as balls, trampolines, and recreational items (recommendation class IIa, level of evidence C).
SurveillanceAt a basic level, the following items should be available: a) a stethoscope, digital oximeter, sphygmomanometer, and anthropometry equipment48; b) subjective effort scale, such as EPInfant-Ex50 (figure 5), OMNI, or Borg (recommendation class IIa, level of evidence C); c) continuous ECG and saturation monitoring for patients at high risk48; d) smart watch for RCRR (recommendation class IIa, level of evidence C); and e) platform for communication between the attending center and patients and guardians for RCRR. The platform should be user-friendly, enabling video calls to answer exercise-related questions, oversee proper execution, and provide periodic encouragement (recommendation class IIa, level of evidence B).48,49
Subjective effort scale, EPInfant-Ex. PE, physical exercise; HR, heart rate. Reproduced with permission from Rodríguez-Núñez.50
Given that any patient can experience a serious adverse event, it is essential to have an emergency protocol in place. Both the guardians and health care team should be trained in basic and advanced cardiopulmonary resuscitation and use of an automated external defibrillator with a full crash cart and supply of supplemental oxygen therapy (recommendation class IIa, level of evidence C).48
CONCLUDING REMARKSCRR for children and adolescents with CHD is still largely unexplored and underused, yet it is an absolutely essential resource, allowing these patients and their families to reach their full potential in life and improving integration into education, higher learning, and society in general. Multidisciplinary teamwork and motivation within and among our countries should be the focus for ensuring proper, effective pediatric CRR.
FUNDINGNone.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCENo artificial intelligence tools were used in the preparation of this article.
AUTHORS’ CONTRIBUTIONSAll authors, members of the working group, contributed equally and have reviewed and approved the final version of the article.
CONFLICTS OF INTERESTNone.
Chile: Sociedad Chilena de Cardiología (SOCHICAR); Sociedad Chilena de Pediatría (SOCHIPE): Paulo Valderrama Erazo, Carlos Fernández, María Eugenia Salinas Cisternas.
Argentina: Sociedad Argentina de Cardiología (SAC); Sociedad de Cardiología Buenos Aires (SOCABA): Romina Carugati, Angela Sardella, Inés Teresa Abella.
Colombia: Sociedad Colombiana de Cardiología y Cirugía Cardiovascular (SCCCC): Sandra Flórez Muñoz, Manuel Huertas-Quiñones. Asociación Colombiana de Medina Física y Rehabilitación (ACMF); Asociación Colombiana de Medina Interna (ACMI): Astrid Fajardo.
Brazil: Sociedad Brasileña de Cardiología (SBC); Sociedad Brasileña de Pediatría (SBP): Isabela de Carlos Back, Aida Luiza Ribeiro Turquetto, Michele Honicky, Luiz Rodrigo Augustemak de Lima, Yara María Franco Moreno, Tales de Carvalho, Liane Hulle Catani.
Dominican Republic: Sociedad Dominicana de Cardiología (SDC): Angelica Grullón.
Uruguay: Sociedad Uruguaya de Pediatría (SUP); Sociedad Uruguaya de Cardiología (SUC): Pedro Chiesa Corrados.
Spain: Sociedad Española de Cardiología Pediátrica y Cardiopatías Congénitas (SECPCC); Sociedad Española de Cardiología (SEC); Asociación Española de Pediatría (AEP): Luisa Garcia-Cuenllas Álvarez.
Mexico: Asociación Nacional de Cardiólogos de México (ANCAM): Lucelli Yáñez-Gutiérrez.