Advances in 3-dimensional (3D) printing over the past 10 years have converted this technology from a specialized industrial process into a widely used tool with applications in many areas, including cardiology.1,2
The 3D printing methodology that has expanded most is fused deposition modeling, and commercially accessible printers today provide 20μm resolution with practically no geometric limitation.
Previous reports have shown the usefulness of 3D printing for pretreatment trials,3 training,4 physiological simulations,5 and other applications. To our knowledge, the approach described here is the first specifically designed for training in percutaneous coronary intervention that reproduces structures while preserving the spatial distribution found in the patient and maintaining high-precision anatomic detail.
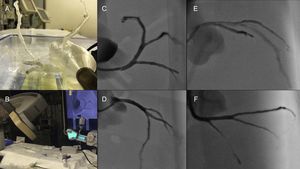
The model was built from synchronized cardiac computed tomography images. The ascending aorta and coronary arteries were segmented using the HOROS open-code software program (The Horos Project), resulting in a mesh of the intravascular volume of these structures. Subsequent processing in the Rhinoceros 3D modeling program produced vessels with a defined wall thickness while maintaining the intravascular lumen dimensions. A bespoke stand was then designed to hold the model in the correct anatomical orientation. The model was prepared for printing in the CURA program (Ultimaker inc).
The resulting model precisely replicated the spatial orientation of the intravascular lumens in the aorta and coronary tree. Blood flow was simulated by continuous pumping of saline solution through the model in an open hydraulic circuit.
A 7-Fr, 3.75 extra-backup curve guide catheter (Medtronic) was introduced into the left coronary artery through a 7-Fr introducer sheath (Terumo), and contrast agent was injected with a contrast pump (ACIST).
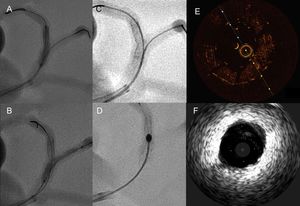
This is the first report of the on-site production of a 3D model for simulated coronary intervention built from patient-specific anatomical characteristics of the aorta and coronary vessels. The correct anatomical positioning of structures in the model reliably reproduced the orientation of the arteries in standard angiographic projections (Figure 1). This level of precision allowed us to verify the applicability of different intracoronary imaging techniques: intravascular ultrasound (Eagle Eye Platinum Digital IVUS, Vulcano Philips) and optical coherence tomography (OCT; Dragonfly OPTIS, St Jude) (Figure 2E and F and ). Furthermore, the model was used to simulate coronary stent implantation (Figure 2A-C) and rotablation (Rotablator, Boston Scientific) (Figure 2D and ).
A-C, Simulation of coronary intervention at the bifurcation of the left anterior descending and primary diagonal arteries. D, Stent rotablation. E, Optical coherence tomography image at the level of a segment with an implanted stent. F, Intravascular echocardiography image at the level of the left coronary branch.
Despite being an accurate replica of the patient's coronary tree, the model has limitations for the simulation of coronary intervention: a) it does not reproduce the mechanical properties of the tissues that form the artery wall; and b) exposure of the model to light and sound mean that the OCT and IVUS images obtained differ from those obtained in the patient. However, as our report shows, the 3D model proved useful for stent evaluation.
In our view, 3D opens up a multitude of possibilities for coronary intervention in both coronary and structural heart disease. The potential of this technology has been demonstrated in diverse industrial applications and in biomedicine, with the implantation in patients of 3D printed prostheses made with biocompatible materials. The cardiological applications of these types of models range from teaching anatomy and angiographic projections to training in complex interventions, such as imaging-guided coronary interventions, treatment of bifurcations or ostial lesions, the development of new procedures, and support for structural interventions. Finally, it is possible to envision a future in which 3D modeling is used to generate personalized devices for cardiovascular intervention.
CONFLICTS OF INTERESTD3 Applied Technologies provided assistance and equipment used in the performance of this study.
.
The authors thank the Cardiology and Radiology Service staff at the Hospital Clínico Universitario in Santiago de Compostela for their collaboration in this study.