Keywords
INTRODUCTION
Acute coronary syndrome (ACS) is an uncommon complication in patients with endocarditis,1 whether in the acute phase of infection or at later times. We therefore do not know the most appropriate treatment.
The aim of this study was to describe the epidemiological, clinical, microbiological, and echocardiographic characteristics of patients with ACS caused by endocarditis, as well as the course of ACS, and to propose a treatment plan for these patients.
METHODS
Patient Groups
Between June 1995 and December 2005, the data on the episodes of patients admitted to 5 hospitals with diagnosis of definitive endocarditis according to the Duke University criteria were prospectively analyzed. All hospitals had a heart surgery service. The episodes were recorded in a standard case report form and the data were entered into a general database. For the present study, 586 episodes of endocarditis were examined. Of these, 481 corresponded to left-sided endocarditis in a total of 460 patients. The 14 patients of this series who presented ACS form the target population of our study.
For all patients, demographic data (age, sex, ethnic origin) and data on the history of prior predisposing heart disease, underlying diseases, the triggering factor, clinical signs, and laboratory abnormalities were collected. Microbiological data, the number of blood cultures, the type of microorganism, and studies of drug sensitivity, drug interactions, and serology were also recorded. Echocardiographic findings from both transthoracic and transesophageal examinations were collected together with information on valvular lesions. Likewise, the type of antibiotics given, their duration, and data on the clinical course were also collected. When heart surgery was done, the indication and the type of intervention were recorded. Finally, the date of discharge or the date and cause of death were recorded.
Definitions
We defined ACS as the presence of characteristic chest pain accompanied by at least one of the following signs: electrocardiographic (ECG) abnormalities and/or elevated enzymatic markers, that followed a characteristic course.2,3
The echocardiographic definitions of vegetation, abscess, pseudoaneurysm, and fistula have been described in previous articles.4
Statistical Analysis
Data were expressed as absolute frequencies or percentages for qualitative variables. Quantitative variables were presented as mean (SD) or median and interquartile range according to whether the data were normally distributed or not. In all cases, the distribution was tested against theoretical models and the hypothesis of homogeneous variance was tested.
The association of qualitative variables was assessed with the χ2 or the Fisher exact test, as indicated. The association between quantitative variables was assessed with the nonparametric Mann-Whitney U test.
For all hypothesis testing, the null hypothesis was ruled out with a type 1 error or an α error of less than 5% (P<.05).
The statistical package used for the analysis was the SPSS version 12.0.
RESULTS
Clinical Characteristics
Of the 586 episodes of infectious endocarditis diagnosed in the study centers, 481 corresponded to left-sided valve endocarditis. Acute coronary syndrome presented as a complication in 14 of these (2.9%). The mean age of these patients was 50 (17) years, 10 patients were less than 70 years old (71%), and 12 were male (85%). Previous heart disease was documented in 10 patients (71%). Seven of these had prosthetic valves, 1 had a mitral valve prolapse, and 2 had degenerative valve disease. In addition, 3 patients had suffered previously from endocarditis. The distribution of prior heart disease in the group without ASC was as follows: 51 patients had rheumatic valve disease (11%), 182 had prosthetic valves (39.3%), 47 had degenerative diseases (10.2%), 24 had congenital heart disease (5.2%), and 17 had mitral prolapse (3.7%), with no significant differences between groups. Of the 14 episodes with ACS, 9 were of community origin (64%), 4 occurred in intravenous drug users (IDUs), and 3 in patients infected with the human immunodeficiency virus (HIV). In the overall series, 21 patients were IDUs (4.5%), and 14 (3%) were HIV positive. Most patients with ACS did not present with triggering factors (71%). Two patients had a history of dental surgery, 1 had undergone prior surgery, and 1 had an intravascular catheter. A range of concomitant diseases were reported: 4 patients were immunosuppressed (28%), 1 had a history of alcoholism (7%), 1 was diabetic (7%), 1 met the diagnostic criteria for chronic obstructive pulmonary disease (7%), 2 had chronic anemia (14%), and 2 had renal failure (14%). One of the patients with renal failure was undergoing dialysis.
The most common clinical presentation on admission was fever, reported in all patients and accompanied by chills in half of the cases. Five patients had sought medical attention because of chest pain. Other common symptoms were presentation of a new murmur in 8 patients and the presence of dyspnea in 7. Only 1 patient presented with functional class II heart failure. Another patient presented with septic shock. The clinical characteristics of the 2 groups are shown in Table 1.
Endocarditis was acute in most patients, presenting in the first 15 days in 10 patients (71%) and between the first and second months in 2 (14%). In 2 patients, endocarditis presented later, after about 3 months.
Microbiology
The causative agent could be isolated in 11 episodes (78.6%). Blood cultures were used to identify the causative microorganism in all patients except one, in whom the microorganism was isolated from a valve culture. The following microorganisms were identified: Staphylococcus aureus in 5 cases, Staphylococcus epidermidis in 1, Streptococcus viridans in 2, Propionibacterium acnes in 1, Candida species in 1, and multiple bacteria (S aureus and Candida species) in 1. The etiologic distribution for the 2 groups is shown in Table 2.
Valve Lesion and Echocardiographic Findings
Vegetations were visualized with transesophageal echocardiography (TEE) in all but 2 patients. In 1 of these patients, vegetations were documented in an autopsy whereas the other only presented periannular complications and no vegetations. In 7 patients, the vegetations had been detected previously by transthoracic echocardiography. In our series, the most common site of infection was the aortic valve. This valve was affected in 12 patients (85.7%). The types of involvement were as follows: 4 patients had native aortic valve involvement, 6 had prosthetic aortic valve involvement (2 mechanical and 4 biological), 1 had native mitral valve involvement, and 3 had multivalvular involvement (mitral prosthesis and native tricuspid valve; aortic valve and native tricuspid valve; and native aortic and mitral valves). Five episodes of early prosthetic endocarditis and 2 cases of late prosthetic endocarditis were reported. In our series, 10 patients presented periannular complications (4 abscesses, 6 pseudoaneurysms, and 1 fistula between the aorta and the left ventricular outlet tract). The patient with the fistula had previously had a large abscess. Thirteen patients had at least moderate valve regurgitation (9 severe and 4 moderate) and moderate stenosis was reported in 1 patient with a biological prosthesis.
The median of the maximum extent of the perinnular complications in patients with ACS was found to be 32.5 mm (30.0-45.75 mm) compared to 12.0 mm (10.0-20.0 mm) in those without ACS (P=.001). The median of the maximum extent of abscesses and pseudoaneurysms was also determined. The median of the maximum extent abscesses in patients with ACS was 30 mm (23.25-33.75 mm) compared to 11.5 mm (10.0-19.25 mm) in those without ACS (P=.005). The median size of pseudoaneurysms in patients with ACS was 39 mm (30.0-48.0 mm) compared to 10.5 mm (10.0-20.0 mm) in those without ACS (P=.001). In the analysis of the size of vegetations, the median in patients with ACS was 11.5 mm (7.75-18.25 mm) compared to 14.5 mm (9.0-20.0 mm) in those without (P=.486).
The site of the periannular complication, which could equally be an abscess or a pseudoaneurysm, was determined by TEE. They were found between 12 o'clock and 3 o'clock in the aortic annulus in 6 cases, whereas the site of the abscess in the other patient was circumferential. In 4 cases, periannular complications, in addition to compressing the left main coronary artery, were also found to increase diastolic flow velocity as measured by the Doppler technique.
Clinical Course
Six patients (42.85%) presented with heart failure and 5 (35%) had septic embolisms--4 prior to treatment and 1 afterwards. The following embolic sites were reported: 3 in the central nervous system (CNS), 1 in the spleen, 1 in the legs, and 3 in the coronary arteries. The 3 patients with coronary embolism had suffered previous embolization, 1 in the CNS, 1 in the spleen, and 1 in the legs. In addition, 2 patients presented with complete atrioventricular block (AVB), 5 patients suffered cardiogenic shock at some point during the clinical course, and 4 had signs of persistent infection. One patient, who had already presented with pericardial effusion on admission, progressed to cardiac tamponade which required pericardiocentesis. The clinical course of the 2 groups is shown in Table 3.
Nine patients (64%) required cardiac surgery. In 2 patients, surgery was elective and in the remaining 7 patients, emergency surgery was done. Multiple indications for cardiac surgery were reported in most patients and the underlying causes were severe valve regurgitation in 6 patients (42%), and perivalvular complications in 8 (57%). Other reasons for remitting a patient for surgery were presence of heart failure in 2 patients, multiple embolisms in 2 patients, and because of the infection itself in a further 2 patients. The reasons why patients indicated for surgery did not finally undergo an operation were as follows: 1 patient died before surgery, 1 HIV-positive patient refused the operation, and in 1 mentally retarded patient, the family did not consent to surgery. Both these patients died. A further 2 patients were not indicated for surgery and survived the follow-up period.
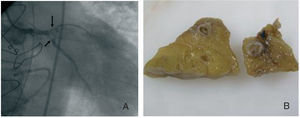
Nine patients (64%) died. An autopsy was available for 4 of these patients (Figure 1). Five of the patients who died had undergone emergency surgery. The cause of death was ACS itself in 8 patients (due to cardiogenic shock or heart failure). The remaining patient died of multiorgan failure.
Figure 1. A: Image of total distal occlusion of the left main coronary artery due to aortic valve vegetation. B: Anatomical slices of the left anterior descending artery of the same patient, in which vegetation can be discerned within the artery.
As shown in Table 3, patients with ACS suffered periannular complications and AVB more often. During the clinical course, these patients had heart failure and cardiogenic shock more often than those without ACS. The mortality rate was also higher in patients with ACS.
Acute Coronary Syndrome
Most episodes of ACS occurred during the first week after diagnosis. In fact, ACS was the reason for admission in 5 patients, and appeared during the first week in a further 5. In 2 patients, presentation occurred during the second week whereas a further 2 patients presented with late ACS--1 at 3 weeks after admission and the other 3 months after finishing the antibiotic course while waiting for elective surgery for valve dysfunction and perivalvular complications.
Although septic coronary embolism was responsible for ACS in 3 patients, most cases were due to extrinsic compression of the coronary arteries secondary to periannular complications (abscesses and pseudoaneurysms in 8 patients). One patient had a history of severe multivessel disease prior to endocarditis and had already suffered additional episodes of ACS. In 2 patients, the cause could not be determined, though it might have been multifactorial: severe aortic regurgitation, fever, anemia, and/or sepsis. One of the patients who suffered ACS of embolic origin also had a large periaortic abscess.
Data were available on cardiovascular risk factors for the last 10 patients. Only 1 of these patients was diabetic, 4 had hypertension, 4 dyslipidemia, and 3 were smokers or former smokers.
The electrocardiographic findings are presented in Table 4. ST-segment depression was observed in 4 patients (2 at an anterolateral site, 1 at an inferolateral site, and 1 at an anterior site). ST-segment elevation was also observed in 4 patients (2 at an anterolateral site and 2 at an inferolateral one). In 1 patient, only T-wave inversion was reported and 1 patient had a previously undocumented left bundle branch block and first-degree AVB that quickly progressed to complete AVB. Furthermore, 2 patients presented with ventricular tachycardia during ACS. At least 7 patients had elevated enzymatic markers of myocardial necrosis, although the values ranged widely. Troponin ranged from 0.23 to 10 ng/mL and creatine kinase from 295 to 2895 U/L. Troponin values were not available for the first patients of the series.
Eight patients had no significant arteriosclerotic coronary lesions, as determined either by catheterization during ACS (3 patients) or prior coronary angiography (less than a year previously, 1 patient), or by autopsy (4 patients). Angioplasty was done in 1 patient in an attempt to dilate an artery occluded by septic embolism. Fibrinolysis was not done for any patient. One patient with severe multivessel disease underwent revascularization surgery at the same time as valve replacement.
DISCUSSION
Several authors have described an increased incidence (up to 90%) of miliary infarctions and microembolization in patients with endocarditis.5-8 On the other hand, obstruction of the epicardial coronary arteries or their main branches with clinical consequences (ACS) is an uncommon complication in patients with left-sided endocarditis, as has been noted occasionally in literature.9-13
Miliary Infarctions
In 1950, Saphir et al14 reviewed the histological and electrocardiographic findings of 79 patients with endocarditis and found intramyocardial abnormalities in all of them, with areas of inflammatory infiltration, myocytic degeneration, perivascular fibrosis, small scars at different stages of repair, miliary infarctions, abscesses, and septic and aseptic microembolization. The electrocardiographic correlation was limited and it was evident that these lesions were much more common than suggested by the cases detected clinically. This finding has been corroborated by other authors.5-8 In one of these studies,5 the authors found necrotic foci in the papillary muscles of 58% of the 38 patients for whom multiple histologic sections were available. Twelve patients had coronary embolism but with involvement of small intramural coronary branches only in 9 of these. In some patients with miliary infarctions and microembolization, the endothelial cells of the coronary capillaries and arterioles were edematous, and perivascular cell infiltrates, arteriolitis, and even necrosis of the medial or adventitial layers of the arterioles were present. Another more recent study15 showed once again that miliary infarctions are rarely reported in clinical practice. Due to the discrepancy between the low incidence of coronary embolism and the high frequency of these myocardial lesions, several factors have been implicated in the etiology of these lesions, such as bacterial toxins or direct tissue invasion by microorganisms, or deposition of circulating immunocomplexes.
Acute Coronary Syndrome
The incidence of ACS in infectious endocarditis is hard to ascertain. In a Russian series of 104 patients, 11 (10.6%) had an infarction as a result of septic embolism.16 In our series of 586 episodes of endocarditis, the incidence of ACS was 2.9%. This is a serious complication of endocarditis; in our series 64% of the patients died. Some patients even required a heart transplant because of ventricular dysfunction and heart failure.17 In a very recent study, increased troponin T levels in patients with endocarditis was a predictor of increased mortality and cerebrovascular accident.18 Normally, ACS occurs early in the course the endocarditis; in fact, many patients present with ACS as the initial manifestation of infection or ACS occurs within a few days of admission to hospital. However, it can also occur after finishing treatment, as was the case in one of our patients. It is more common in patients with aortic valve infection and is not linked to any microorganism in particular,1,10,11,19 although it was associated with virulent microorganisms in our series.
The presentation and clinical course of ACS in patients with endocarditis are similar to those observed in individuals with arteriosclerotic coronary arteriopathy.1 In most cases, the infarction is anterior or anterolateral. We were able to find only 1 case in the literature of an infarction at a purely inferior site.20 Many of these patients have embolisms at other sites (kidney, spleen, etc).21,22 In our series, the most common mechanism responsible for myocardial ischemia was coronary compression due to large periannular aortic complications (abscess and pseudoaneurysms), particularly when they were located between 12 o'clock and 3 o'clock on the aortic annulus. Other investigators have also reported this type of complication.23-26 Some groups have found that the most common pathogenesis of ACS in patients with endocarditis is coronary embolism.16,27 Other less common mechanisms responsible for myocardial ischemia in patients with endocarditis include obstruction of the coronary ostium by a large vegetation,16 such as in cases of fungal endocarditis with large vegetations; coexistence of coronary arteriosclerotic lesions that become apparent during active infection, associated with anemia, fever, and activation of the coagulation system in septic patients; and the presence of severe acute aortic valve regurgitation which can by itself cause myocardial ischemia through reduced coronary perfusion pressure and decreased coronary reserve28 (Table 5).
Treatment of ACS in these patients is complicated by the higher risk associated with anticoagulants and fibrinolytic agents in patients with endocarditis. In some cases, these drugs have proved successful,29 but in most patients they have been accompanied by cerebral hemorrhage with a fatal outcome.1,9-12 For this reason, for some investigators,12 and indeed for us as well, endocarditis is a contraindication for the use of fibrinolytic agents.
Although coronary angiography in patients with endocarditis is a safe procedure according to the experience of some investigators,30 we think there is a risk that fragments of vegetation may become dislodged in cases of active aortic valve endocarditis if the catheter comes into contact with the valve surface or when the contrast is injected. Therefore, in view of the results of these studies, when a patient presents with ACS and endocarditis, our initial diagnostic procedure of choice is TEE. If periannular complications are present, particularly without ST-segment elevation in the ECG, the patient is referred for surgery without prior coronary angiography because ischemia is likely to be secondary to extrinsic compression of the left main coronary artery or the proximal segment of the left anterior descending artery. In contrast, a diagnostic coronary angiogram is done if no aortic valve abscesses or pseudoaneurysms are detected, or ST-segment elevation is found in the ECG. If a coronary artery is found to be occluded, we can opt for mechanical reperfusion by means of balloon angioplasty and stent placement if necessary (Figure 2). A number of authors have described the subsequent appearance of a mycotic aneurysm at the site of angioplasty.1,31,32 Therefore, we advise angiographic follow-up after angioplasty. Surgery would be indicated if a coronary mycotic aneurysm were detected because of its tendency to rupture.31,33
Figure 2. Treatment of acute coronary syndrome in patients with infectious endocarditis. TPCA indicates transluminal percutaneous coronary angioplasty; TEE, transesophageal echocardiography; ACS, acute coronary syndrome.
CONCLUSIONS
At present, ACS is an uncommon complication in patients with endocarditis. It normally occurs in the acute phase of the disease (first 15 days) and is more often associated with virulent microorganisms, aortic valve infection, severe valve regurgitation, and large periannular complications. The mechanism responsible for myocardial ischemia varies, but extrinsic coronary compression by these periannular complications is common. This syndrome is associated with high mortality in patients with endocarditis.
ABBREVIATIONS
ACS: acute coronary syndrome
AVB: atrioventricular block
ECG: electrocardiography
TEE: transesophageal echocardiography
See editorial on pages 5-6
Correspondence: Dr. I. Vilacosta.
Instituto Cardiovascular. Hospital Universitario San Carlos.
Martín Lagos, s/n. 28040 Madrid. España.
E-mail: mcmanzano@lycos.es
Manuscript received March 24, 2006.
Accepted for publication September 14, 2006.