Acute coronary syndrome (ACS) in patients with normal coronary arteries has a prevalence of between 8% and 25%.1,2 Several mechanisms have been implicated in its etiopathogenesis, including coronary vasospasm, hypercoagulable states, and embolization.2 Coronary angiography can assess the extent of stenosis but not the state of atheromatous plaques. The technique is therefore of limited use when complicated plaques are present, particularly in the absence of significant lesions.3 Atherosclerotic plaques can, however, be characterized by optical coherence tomography (OCT).2,3 Previous studies with this technique in ACS have focused on characterizing the substrates of angiographically significant lesions.4,5 None, however, have studied unstable substrates in patients with insignificant findings on angiography. In a recent study of patients who were resuscitated after sudden death and had lesion-free coronary arteries, intracoronary ultrasound allowed identification of unstable plaque substrates in all patients.6 OCT has demonstrated better resolution than intracoronary ultrasound in the characterization of atheromatous plaques.4,5 The objective of our study was to identify the presence of unstable substrates using OCT in patients with ACS and angiographically normal coronary arteries or angiographically insignificant lesions (< 50%).
Between April 2012 and September 2014, 1178 patients with high-risk ACS underwent coronary angiography. Of these, 53 (5.14%) had normal coronary arteries and 58 (5.63%) had angiographically insignificant lesions. Of these 111 patients, 21 met the following criteria: a) clinical manifestations of angina or equivalent; b) electrocardiographic findings indicative of ischemia; c) elevated levels of biomarkers of myocardial damage (troponin I or ultrasensitive troponin I), and d) wall motion abnormalities on echocardiography, magnetic resonance imaging, or ventriculography. Based on angiographic irregularities and electrocardiographic and wall motion abnormalities, the artery considered the cause of ACS was selected and OCT (Dragonfly™ Duo OCT Imaging Catheter, St Jude Medical; St. Paul, Minnesota, United States) performed. Patients with ST-segment elevation ACS underwent emergency catheterization. None received fibrinolytic agents. In patients with non-ST-segment elevation ACS, an early invasive strategy was followed with coronary angiography in the first 24 to 48hours. Only 1 patient had a Q-wave infarction and all had elevated troponin I or ultrasensitive troponin I and creatine kinase.
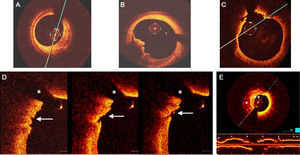
The baseline characteristics of the patients are summarized in Table. The mean age was 54.7±14.79 years and 7 patients (33.3%) presented with ST-segment elevation ACS. The artery most frequently considered the cause of the event was the left anterior descending artery (66.7%). Quantitative coronary angiography and OCT showed an acceptable correlation (Table). Qualitative analysis with OCT (Table) showed that 20 patients had signs of arteriosclerosis and 9 had stable plaques (Figure A). Of these 9 plaques, 2 were considered vulnerable as they had a very thin fibrous cap with a large necrotic core. In 8 patients, residual thrombotic material was found (Figure B), associated with the presence of ruptured plaques. Ten patients had ruptured plaques (Figure C), 2 had plaque erosion (Figure D), and 3 had superficial calcified nodules with thrombus (Figure E) or rupture of a thin fibrous cap. Eleven patients had several remarkable findings, 6 had only stable plaques, and 1 had normal coronary arteries with no findings on OCT; 5 patients (22.7%) had anterior ST-segment elevation ACS and apical akinesis with subsequent normalization of ventricular function, indicative of tako-tsubo syndrome. Only 1 patient had a normal left anterior descending artery on OCT and 4 had unstable substrates. In summary, of the 21 patients studied, 20 showed signs of coronary arteriosclerosis and 14 (66.7%) had signs of complicated atherosclerotic plaque that could cause ACS, despite the absence of angiographically significant lesions on coronary angiography.
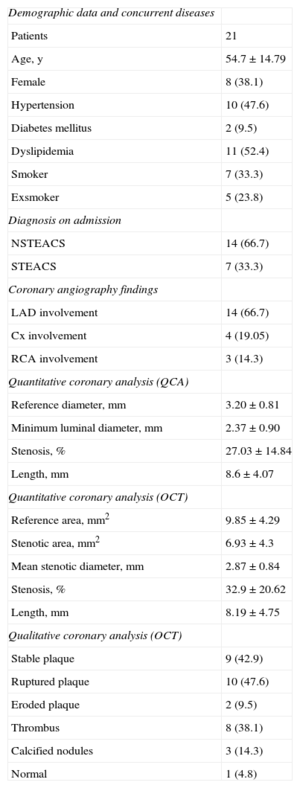
Baseline Characteristics of the Study Patients
| Demographic data and concurrent diseases | |
| Patients | 21 |
| Age, y | 54.7±14.79 |
| Female | 8 (38.1) |
| Hypertension | 10 (47.6) |
| Diabetes mellitus | 2 (9.5) |
| Dyslipidemia | 11 (52.4) |
| Smoker | 7 (33.3) |
| Exsmoker | 5 (23.8) |
| Diagnosis on admission | |
| NSTEACS | 14 (66.7) |
| STEACS | 7 (33.3) |
| Coronary angiography findings | |
| LAD involvement | 14 (66.7) |
| Cx involvement | 4 (19.05) |
| RCA involvement | 3 (14.3) |
| Quantitative coronary analysis (QCA) | |
| Reference diameter, mm | 3.20±0.81 |
| Minimum luminal diameter, mm | 2.37±0.90 |
| Stenosis, % | 27.03±14.84 |
| Length, mm | 8.6±4.07 |
| Quantitative coronary analysis (OCT) | |
| Reference area, mm2 | 9.85±4.29 |
| Stenotic area, mm2 | 6.93±4.3 |
| Mean stenotic diameter, mm | 2.87±0.84 |
| Stenosis, % | 32.9±20.62 |
| Length, mm | 8.19±4.75 |
| Qualitative coronary analysis (OCT) | |
| Stable plaque | 9 (42.9) |
| Ruptured plaque | 10 (47.6) |
| Eroded plaque | 2 (9.5) |
| Thrombus | 8 (38.1) |
| Calcified nodules | 3 (14.3) |
| Normal | 1 (4.8) |
Cx, circumflex artery; LAD, left anterior descending artery; NSTEACS: non-ST-segment elevation acute coronary syndrome; RCA, right coronary artery; STEACS: ST-segment elevation acute coronary syndrome.
Qualitative coronary analysis (optical coherence tomography). A: Stable plaque. B: Residual ruptured plaque. C: Ruptured plaque D: Consecutive panels that show rupture of the intima, indicating plaque erosion (arrows), acoustic shadow of the guide (*). E: Superficial calcified nodule (*) with adhered laminar thrombus (**).
The findings of this small series of patients with angiographically insignificant lesions suggested destabilization of vulnerable plaques as the most probable cause of ACS. OCT has been shown to be a useful technique in the characterization of substrates causing ACS, as it can detect vulnerable plaques, plaque rupture, thrombi, superficial calcified nodules, and plaque erosion. Identification of these substrates could have important prognostic and therapeutic implications.
One limitation of this study is its small sample size. Further study limitations include the lack of OCT studies of the other coronary arteries not considered as the cause of the clinical manifestations and the lack of a control group. Furthermore, we did not perform coronary vasomotor tests and, finally, we did not definitively identify the cause of ACS in 6 patients with identification of stable plaques only. In these patients, the manifestations may have been the result of coronary vasospasms, embolism, or even acute myocarditis. Nevertheless, when coronary angiography fails to clearly detect any causative lesions in patients with ACS despite clinical suspicion, imaging techniques such as OCT can identify unstable coronary substrates in a substantial proportion of individuals (66.7% of our series). In such cases, the technique could be used as an additional imaging technique to try to clarify the cause of ACS.