The cardiac manifestations of coronavirus disease 2019 (COVID-19) are not well established, but there have been reports of cardiovascular complications.1
We describe the case of a 74-year-old man with a past history of hypertension, type 2 diabetes mellitus, and ischemic stroke who underwent a thrombectomy in 2017. He had been in solitary confinement since returning from a trip to a COVID-19 risk area 13 days earlier. He presented at the emergency room with general malaise and shortness of breath. He had had flu-like symptoms and fever for 2 days before admission, as well as self-limiting chest pain.
On arrival at the emergency room, the patient had severe hypoxemic respiratory failure and was administered oxygen via a high-flow nasal cannula. His condition progressively worsened and he required endotracheal intubation and invasive mechanical ventilation.
The admission electrocardiogram (figure 1A) showed sinus tachycardia with minimal isolated ST-segment elevation in lead III and ST-segment depression in V2-V4. The tachycardia was not observed on successive electrocardiograms. The chest radiograph showed mainly peripheral cotton-wool infiltrates in both pulmonary fields (figure 1B), and the admission blood test showed acute kidney failure (creatinine, 2mg/dL), and significant enzyme elevation with a creatine kinase MB level of 731U/L and a high-sensitivity cardiac troponin T level of 1162ng/L. Elevated levels were also observed for interleukin 6 (135pg/mL), ferritin (145μg/L), lactate dehydrogenase (992U/L), D-dimer (55mcg/mL), and N-terminal pro-brain natriuretic peptide (4076pg/mL).
A transthoracic echocardiogram was performed and showed left ventricular dysfunction with inferolateral hypokinesis. Given the high index of suspicion for COVID-19 based on the clinical presentation and the patient's recent trip, the patient was tested for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and tested positive.
In the following hours, the patient developed clear hemodynamic deterioration followed by mixed shock, which required initiation of vasoactive support with noradrenaline up to a dose of 0.44mg/kg/min. Emergency cardiac catheterization (figure 1C, D) showed 3-vessel coronary artery disease with acute thrombotic occlusion of the right coronary artery. This was treated with percutaneous coronary intervention and the placement of 2 drug-eluting stents; the thrombus migrated to the posterior descending artery.
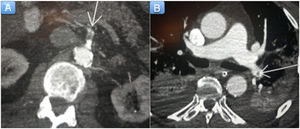
The patient was administered dual antiplatelet therapy (aspirin and clopidogrel) and anticoagulation with sodium heparin. He was also started on hydroxychloroquine and tocilizumab. His condition progressed slowly over the following hours, with further hemodynamic deterioration. We therefore decided to perform a computed tomography scan of the chest and abdomen, which showed multiple arterial thrombosis and findings consistent with mesenteric ischemia (figure 2A), splenic infarction, and pulmonary thromboembolism (28%) (figure 2B). The patient died 72hours after admission.
We have presented the case of an elderly patient who developed acute coronary syndrome, mixed shock, and shortness of breath during the course of SARS-CoV-2 infection.
COVID-19 mainly causes complications such as pneumonia and acute respiratory distress syndrome. Cardiovascular complications have been reported in several cases and are a marker of poor prognosis.1 Acute cardiac injury, defined as a significant elevation of cardiac troponins, is the most widely reported cardiac abnormality in COVID-19.1 Numerous cases of concomitant heart failure have also been described. Acute coronary events appear to be relatively uncommon, perhaps because of the high levels of systemic inflammation and prothrombotic effects caused by SARS-CoV-2. There have also been reports of ventricular dysfunction and acute myocarditis.1
Of note in the present case was the co-occurrence of rapid-onset mixed shock and inferior ST-segment elevation acute coronary syndrome (STEACS). We considered implanting an intra-aortic balloon pump, but decided not to because of the risk of movement due to the need for prone ventilation.
A hypercoagulable state with disseminated intravascular coagulation favoring the development of thrombotic events has also been described in COVID-19.2 Recent studies have shown that D-dimer levels are predictive of mortality. Our patient had a very high D-dimer level (55μg/ml), leading us to hypothesize that severe SARS-CoV-2-19 infection could trigger thrombotic events, particularly in patients with cardiovascular risk factors.
Primary percutaneous coronary intervention should also be the reperfusion method of choice in patients with COVID-19 and STEACS, although there are exceptional cases where fibrinolysis could be considered.3 Just as with any patient in cardiogenic shock, only the culprit vessel should be revascularized. Extracorporeal membrane oxygenation may be more advisable than other mechanical circulatory support systems in patients with COVID-19 and shock.3
Antiplatelet therapy with prasugrel should be prioritized, as antiretrovirals potentiate the effect of ticagrelor and may reduce that of clopidogrel.3 We did not administer prasugrel because of the patient's history of stroke. Close monitoring of the QTc interval is essential because of drug-drug interactions. Although the evidence is not clear, anticoagulant therapy appears to be associated with a better prognosis in patients with severe COVID-19 and significantly elevated D-dimer levels.2
We have presented a case of acute coronary syndrome in a patient with COVID-19. The case is of particular interest because of the patient's susceptibility to severe thrombotic events and rapid-onset shock.
.