Keywords
INTRODUCTION
Pheochromocytomas are rare tumors originating in the adrenal or extra-adrenal chromaffin tissue and characterized by excessive secretion of catecholamines. This excess, in addition to hypertension, nausea, sweating, and palpitations, can be accompanied by various cardiovascular symptoms such as arrhythmia, acute coronary events, and organic or functional myocardial involvement, even without coronary disease. Although the literature contains several reports of acute myocardial ischemia related to pheochromocytoma, there are only a few cases in which the myocardial condition is accompanied by intraventricular thrombosis.1 We report on the case of a patient with an adrenal pheochromocytoma and catecholamineinduced symptoms, diffuse myocardial ischemia in the electrocardiogram (ECG), echocardiographic signs of left ventricular dysfunction with apical akinesia, and a left ventricular thrombosis of early onset.
CASE STUDY
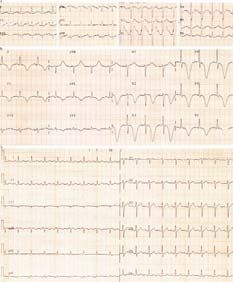
A 59-year-old man with a history of hypertension diagnosed five months previously was admitted in November 2002 for severe general malaise, epigastralgia, nausea, sweating, tachypnea and palpitations lasting for 3 hours. Physical examination in the emergency room showed rhythmic tachycardia of 132 bpm and blood pressure (BP) of 210/90 mm Hg, with no other relevant findings. Baseline arterial blood findings were: pH, 7.34; pCO2, 25 mm Hg; pO2, 64 mm Hg, and bicarbonate 14 mmol/L. The hemogram, coagulation study and ion levels were normal; blood glucose was 238 mg/dL and serum amylase, 443 U/L (10-220). The ECG (Figure 1A) showed sinus tachycardia with 132 beats per minute and nonspecific alterations of ventricular repolarization. The clinical condition was self-limiting, and the patient was hospitalized. The next day he presented similar symptoms, with a BP of 170/110 mm Hg and evidence of diffuse ischemia in the ECG (Figure 1B). The creatine kinase (CK) level was not higher than 220 U/L and the MB fraction was normal. An echocardiogram performed 48 h post-admission showed regional wall motion abnormalities akinesia of the middle and apical segments, an ejection fraction of 25%, and a 30*6-mm left intraventricular thrombus adhering to the apex and posterior wall (Figure 2). Abdominal computed tomography performed on the basis of suspected pheochromocytoma showed a contrast-enhancing left adrenal mass with a diameter of 3.5 cm (Figure 3). Catecholamine levels in 24-h urine were: free adrenaline, 227 µg (normal, 0-20); free norepinephrine, 487 µg (normal, 10-70), and vanillylmandelic acid, 18 mg/24 h (normal, 0-5). A isotopic study with 123I-meta-iodobenzylguanidine confirmed uptake by the left adrenal mass; the coronary angiography was normal. On day 12 post-admission, the patient still showed the same electrocardiographic signs indicated in Figure 1B, but presented sudden speech disturbances and a left retrosylvian ischemic infarction in the cerebral CT scan. Ultrasound study of the supra-aortic trunks showed only slight atheromatous disease. An echocardiogram performed 30 days after admission showed recovery of global systolic function, an ejection fraction of 66%, and a decrease in thrombus size. Resolution of the thrombus was confirmed 2 weeks later on echocardiography. After treatment with heparin and phenoxybenzamine, and with the electrocardiogram shown in Figure 1C, the patient underwent surgical left adrenalectomy on day 58 post-admission. Histological examination of the specimen confirmed the diagnosis of pheochromocytoma. One year after the surgery, the mixed speech alteration persisted but blood pressure was normal without hypotensive treatment.
Figure 1. A) Electrocardiogram at admission, showing sinus tachycardia with 132 beats per minute. B) ECG on day 2 post-admission, with sinus rhythm, diffuse myocardial ischemia, or involvement. C) ECG at discharge: normal.
Figure 2. Echocardiographic study during admission. Left ventricular thrombosis of 30*6 mm (arrow).
Figure 3. Abdominal computed tomography: 3.5-cm mass at the largest diameter (large arrow) in the left adrenal gland. A 2-cm nodule was observed in the right adrenal (small arrow).
DISCUSSION
Pheochromocytoma can produce the characteristic clinical symptoms of hypertension (which may be sustained, paroxysmal, or without these features), palpitations, sweating, and headache, or it can manifest only with nausea and nonspecific sweating due to hyperglycemia and metabolic acidosis induced by acute catecholamine release, as occurred in the patient reported here.2-4 The common cardiovascular manifestations include hypertension, ST segment and T-wave electrocardiographic abnormalities (24% in the series of Liao et al), and acute myocardial infarction, even without coronary disease.5-7 The pathogenesis of the heart disease has been related to functional myocardial hypoxia, coronary spasm, changes in membrane permeability for Ca2+ and Mg2+ and myocardial cell metabolic changes, all caused by the oxidative metabolites of catecholamines.8,9
The interest of our patient lies in the early development of left ventricular thrombosis, despite the presence of sinus rhythm. In addition, our patient had signs of diffuse ischemia or myocardial involvement, despite a normal coronary angiography and no myocardial infarction (ruled out on the basis of the clinical, enzymatic and echocardiographic evidence). We associate this with the ischemic stroke presented by the patient on day 12 post-admission. Although an atherothrombotic origin cannot be ruled out because of the patient's age and history of hypertension, the scant echocardiographic evidence of atherosclerotic carotid involvement makes this etiology unlikely. The pathophysiology of this complication is probably related to that of the transient left ventricular apical ballooning, which manifests as chest pain or discomfort, ECG alterations suggestive of an acute coronary event, little or no enzyme elevation and left ventricular apical dyskinesia which normalizes in a few days. Although this syndrome, first described by Tsuchihashi et al in Japan, is more prevalent among women,10-12 its relationship with situations of severe emotional stress and its clinical evolution share many of the same characteristics observed in our patient. In any case, we believe that pheochromocytoma should be considered in the differential diagnosis of acute coronary syndrome, particularly if the clinical symptoms, electrocardiographic evidence and enzyme results are abnormal.
Correspondence: Dr. S. Prieto.
Servicio de Medicina Interna. Hospital Universitario 12 de Octubre. Planta 13.
Ctra. de Andalucía, km. 5,400. 28041 Madrid. España.
E-mail: yebra22@hotmail.com
Received April 20, 2004.
Accepted for publication October 5, 2004.